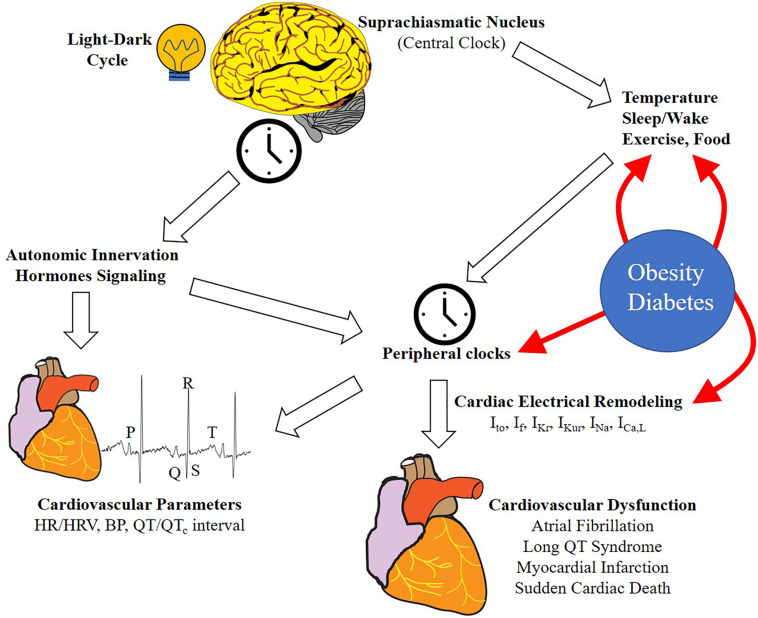
FIGURE 1.
Schematic representation of the regulation of circadian rhythms of cardiovascular function. Light/dark cycle entrains the central clock in the SCN, which in turn regulates rhythmic oscillation in peripheral tissues clocks through neurohumoral signaling. Peripheral clocks are also regulated by other stimuli including sleep/wake, food intake, exercise, and temperature. In the heart, this regulation results in the rhythmicity of different physiological (cardiovascular parameters and ion channel expression) and pathological processes (cardiovascular diseases and arrhythmia). Lifestyle can influence and alter the effect of some external cues (HFD, shiftwork etc.). Metabolic diseases (e.g., obesity and diabetes) can influence the circadian rhythms in different tissues and processes, particularly in the heart, leading to ion channel expression remodeling and increasing the risk of cardiovascular disease (CVD) and arrhythmias. HR, heart rate; HRV, heart rate variability, BP, blood pressure; Ito, transient outward potassium current, If, funny current, IKr, rapid delayed rectifier potassium current; IKur, ultra-rapid delayed rectifier potassium current; INa, sodium current; ICaL, L-type calcium current.