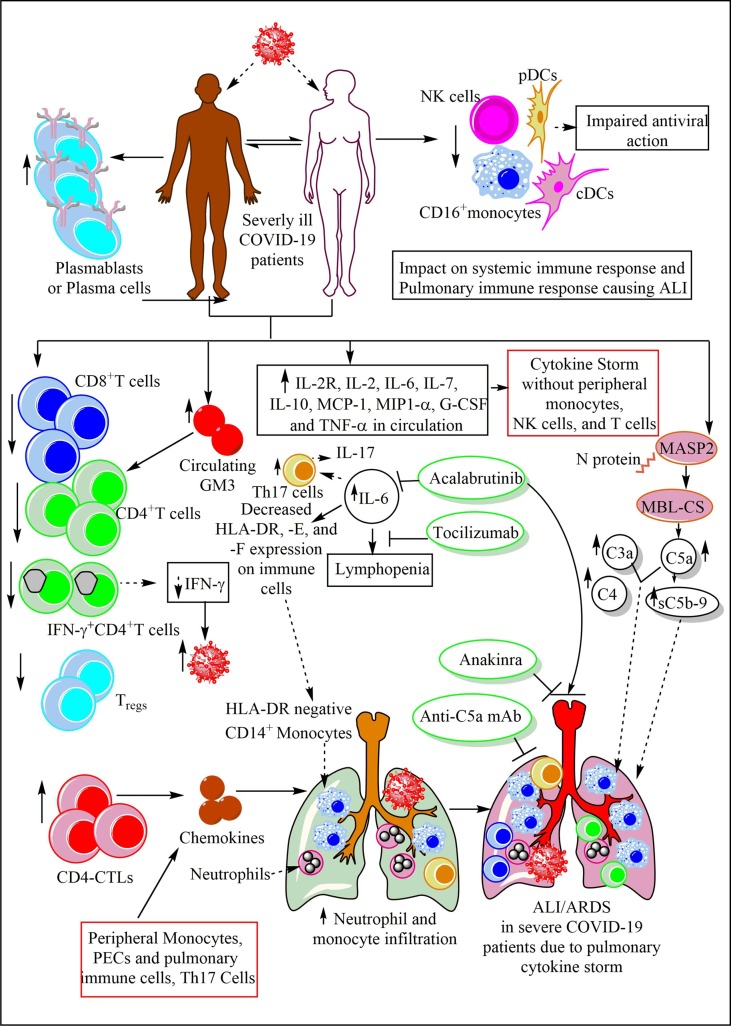
Fig. 6.
The immune response in the severe COVID-19 patients. These sever COVID-19 patients show a decrease in the CD4+T cells, CD8+T cells, IFN-γ+CD4+T cells, and Tregs. Due to decreased IFN-γ levels the viral load increases. The increase in the circulating GM3 is well correlated with the decreased CD4+T cell number in the circulation. The increased CD4-CTLs along with peripheral monocytes, pulmonary epithelial cells (PECs) and pulmonary Th17 cells secrete various chemokines, which increase the neutrophil and monocyte infiltration in the lung. The increased accumulation of neutrophils, monocytes, CD4+T cells, and Th17 cells induce pulmonary cytokine storm to cause ALI/ ARDS. The systemic cytokine also generates but does not involve monocytes, NK cells, and T cells. The increased IL-6 levels cause lymphopenia, increase Th17 cells secreting pro-inflammatory cytokines (IL-17, IL-22 etc.). IL-6 also decreases HLA-DR expression on immune cells, including monocytes, which migrate to the lungs. The HLA-E and HLA-F expression on immune cells also decreases. Tocilizumab inhibits IL-6-mediated immune response to protect against COVID-19-induced pneumonia and ALI. Acalabrutinib, a BTK inhibitor also inhibits IL-6 production and the associated lymphopenia and other severe COVID-19 symptoms, including ALI. The CS activation also play a crucial role in sever COVID-19. The increased C5a, C3a, C4, and membrane attack complex (MAC) levels well correlate with COVID-19 severity and ALI. The anti-C5a mAb protects against severe COVID-19 and ALI. Anakinra, an IL-1R antagonist also inhibits neutrophils and monocytes infiltration in the lung to protect against severe COVID-19-induced ALI. These patients show increased levels of plasma cells than mild or moderate COVID-19 patients. A decrease in the systemic NK cells, pDCs, cDCs (CD1c+ and CD141+DCs), and CD16+ monocytes occurs systemically causing an impaired antiviral immune response.