Abstract
Therapeutic strategies that target leukemic stem cells (LSC) provide potential advantages in the treatment of chronic myeloid leukemia (CML). Here we showed that selective blockade of plasminogen activator inhibitor-1 (PAI-1) enhances the susceptibility of CML-LSC to tyrosine kinase inhibitor (TKI), which facilitates the eradication of CML-LSC and leads to sustained remission of the disease. We demonstrated for the first time that the TGF-−PAI-1 axis was selectively augmented in CMLLSC in the bone marrow (BM), thereby protecting CML-LSC from TKI treatment. Furthermore, the combined administration of the TKI imatib plus a PAI-1 inhibitor, in a mouse model of CML, significantly enhanced the eradication of CML cells in the BM and prolonged the survival of CML mice. The combined therapy of imatinib and a PAI-1 inhibitor prevented the recurrence of CML-like disease in serially transplanted recipients, indicating the elimination of CML-LSC. Interestingly, PAI-1 inhibitor treatment augmented membrane-type matrix metalloprotease-1 (MT1-MMP)-dependent motility of CML-LSC, and the anti-CML effect of PAI-1 inhibitor was extinguished by the neutralizing antibody for MT1-MMP, underlining the mechanistic importance of MT1-MMP. Our findings provide evidence of, and a rationale for, a novel therapeutic tactic, based on the blockade of PAI- 1 activity, for CML patients.
Introduction
Chronic myeloid leukemia (CML) was the first luekemia to be identified with a specific tumorigenic chromosomal abnormality - the Philadelphia chromosome.1 Subsequent studies identified that the translocation event, occurred between t(9;22) (q34;q11), fused the breakpoint cluster region gene (BCR) with the Abelson kinase gene (ABL1) and produced the BCR/ABL oncogene.2,3 This BCR/ABL fusion protein possesses constitutive tyrosine kinase activity resulting in the development of myeloid leukemia through aberrant differentiation of hematopoietic stem/progenitor cells (HSPC) toward the myeloid lineage. Although development of tyrosine kinase inhibitors (TKI) that target the abnormal activation of tyrosine kinase, such as imatinib, has dramatically improved the prognosis of CML,4,5 the disease often relapses, even after complete remission achieved under TKI therapy, thus remaining a central problem in the treatment of CML. It has been hypothesized that leukemic stem cells (LSC), also identified as leukemic initiating cells, are the cells that possess the unique ability to resist the cytotoxic agents and are responsible for the relapse of leukemia,6–8 highlighting the need for therapeutic strategies that specifically target this population of cells.
LSC are thought to possess properties similar to those characterizing normal HSPC, including the capacity for self-renewal, cell cycle quiescence, and resistance to traditional chemotherapy.6,9 Studies have shown that transforming growth factor-(TGF-) signaling plays supportive roles in normal hematopoiesis and leukemogenesis. Yamazaki et al.10,11 reported that TGF-signaling is essential for the maintenance of HSPC within the bone marrow (BM) microenvironmental niche and promotes Smaddependent HSPC hibernation. In the same vein, Naka et al.12,13 showed that TGF-signaling is also essential for the maintenance of CML-LSC. Thus, suppression of TGF-signaling deserves investigation for the purpose of eliminating CML-LSC.
Like their normal hematopoietic counterparts, CMLLSC are presumed to reside in specific niches in the BM microenvironment, which likely contribute to relapse after chemotherapy.14–16 We have recently uncovered a pathway by which TGF-signaling regulates HSPC retention in the niche.17 TGF-induces the expression of plasminogen activator inhibitor-1 (PAI-1), a major physiologic serine protease inhibitor (serpin) of the fibrinolytic system. In HSPC, PAI-1, known conventionally as an extracellular fibrinolysis-related serpin, functions intracellularly (subsequently referred to as iPAI-1) and inhibits the proteolytic activity of proprotein convertase, furin, which consequently diminishes membrane type-1 metalloprotease (MT1-MMP) activity.17 MT1-MMP promotes HSPC motility by breaking down pericellular matrix proteins and adhesion molecules necessary for anchoring HSPC to the niche.18,19 Genetic or pharmacological inhibition of TGF--iPAI-1 signaling increases MT1-MMP-dependent cellular motility, causing detachment of HSPC from the niche, making them receptive to extraneous stimuli.17,20 In line with our report, a number of studies have demonstrated that both TGF-and PAI-1 play important roles in numerous physiological and pathological conditions, including wound healing, obesity, cardiovascular disease and cancer.21–23 Therefore, we hypothesize that blockade of iPAI-1 activity facilitates the dislocation of CML-LSC in the BM, which in turn renders CML-LSC susceptible to TKI therapy, resulting in the eradication of CML-LSC and sustained disease remission.
Methods
Additional methods are presented in the Online Supplementary Methods, available on the Haematologica web site.
Pharmacological properties of inhibitors
Three different PAI-1 inhibitory compounds (TM5275, TM5509 and TM5614) were used.24 All three selectively and effectively inhibited PAI-1 activity with a half-maximal inhibition (IC50) value <6.95 M in a tPA-dependent hydrolysis assay. The PAI-1 inhibitors (up to 100 M) did not interfere with other serpin/serine protease systems such as 1-antitrypsin/trypsin and 2-antiplasmin/plasmin. The TGF-inhibitor, LY364947, is a potent and selective inhibitor of the TGF- receptor I, inhibiting phosphorylation of Smad3 by TGF-receptor I kinase (IC50=59 nM).
CML mouse model
Several different mouse models of CML-like disease were utilized in this study. First, we used a BCR/ABL1 transduction/transplantation- based CML model (BCR/ABL1-CML mice) as previously described.12,25 Briefly, normal LSK cells (4–5×104 cells per recipient mouse) isolated from mononuclear cells of fetal liver (embryonic day E14.5) or adult BM (8-12 weeks old) were transduced with the human BCR/ABL1-ires green fluorescent protein (GFP) retrovirus and transplanted into irradiated (9 Gy) recipient C57BL/6J mice purchased from CLEA Japan (Tokyo). Another set of experiments, gene-modified 32D cell lines were also transplanted into non-irradiated C3H/HeNCrl mice (CLEA Japan). CMLlike disease developed in these recipient mice by 12–20 days post transplantation.
A tetracycline (tet)-inducible CML mouse model26,27 was also used in this study. Tal1-tTA mice (JAX, #006209) and TREBCR/ ABL1 transgenic mice (JAX, #006202), both on an FVB/N genetic background, were purchased from the Jackson Laboratory. Tal1-tTA and TRE-BCR/ABL1 transgenic mice were interbred to generate Tal1-tTAxTRE-BCR/ABL1 double-transgenic mice. These animals were maintained in cages supplied with drinking water containing 20 mg/L doxycycline (Sigma-Aldrich). At 8-10 weeks after birth, BM cells of Scl/Tal1-tTAxTRE-BCR/ABL double-transgenic (Ly5.2; CD45.2) mice were mixed with competitor BM cells obtained from congenic (Ly5.1; CD45.1) mice and then were transplanted to lethally irradiated (9 Gy) wild-type (WT) hosts. The recipients bred in the presence of doxycycline, and BCR/ABL expression was induced by doxycycline withdrawal 2 months after transplantation. All induced recipient mice progressively developed CML-like disease associated with a severe myeloid cell expansion in the BM, spleen and peripheral blood (PB), and splenomegaly. The mice became moribund ~3 weeks after induction.
In order to examine the in vivo effects of the combined administration of imatinib (IM) plus PAI-1 inhibitors, BCR/ABL1-CMLaffected mice received vehicle alone, or IM (Gleevec; 150-400 mg/kg/day; Novartis) and/or PAI-1 inhibitor (TM5257, 100 mg/kg/day; TM5009 or TM5614, 10 mg/kg/day) in vehicle, and, at the same time, mice were intraperitoneally injected with 1 mg/kg anti-MT1-MMP antibody (Merck Millipore) or nonimmune species- and isotype-matched control antibody for 5 consecutive days. Treatment was delivered by oral gavage on days 8–30 post transplantation. Three to 4 months after transplantation, PB, spleen, and BM samples were collected from individual recipients and subjected to analyses and secondary transfer experiments.
Protocols concerning animal experiments and recombinant gene experiments were approved by the Animal Care Committee and the Gene Recombination Experiment Safety Committee of Tokai University.
Results
TGF--iPAI-1 axis is activated in CML-LSC
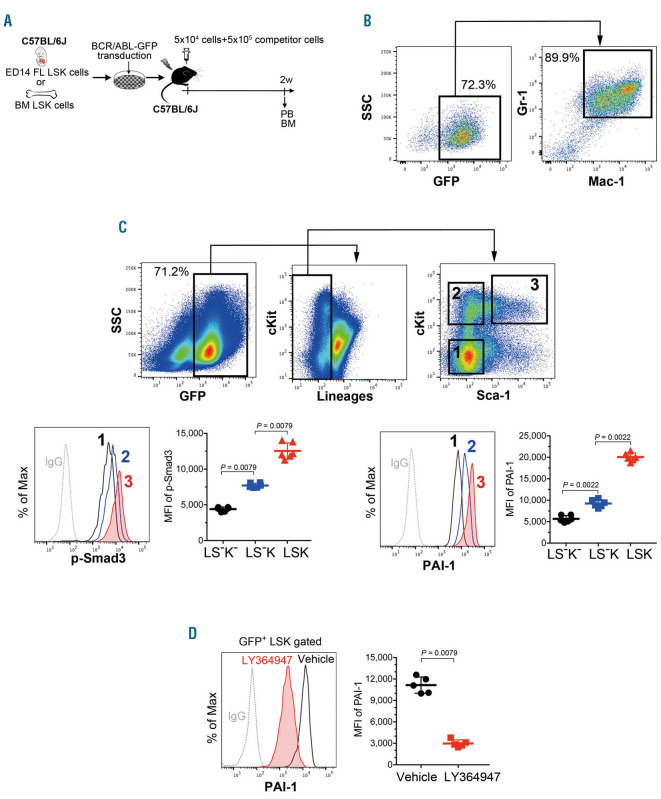
LSC are analogous to HSPC in so many aspects; both cell types are characteristically slow cell-cycling and have a high tendency to localize in particular sites, so called niche dependency.14,15,28–30 In addition, the surface markers of CML-LSC and normal HSPC are shown to be almost identical both in murine models and in human samples. For example, transplantation studies of BCR/ABL-induced murine CML models demonstrated that BCR/ABLexpressing LSC activity is confined to the fraction of Lineage (Lin)–Sca1+c-Kit+ (LSK) cells that contains murine HSPC population.12,31 We have recently shown that TGF-signaling regulates the motility of HSPC in the niche through selective upregulation of iPAI-1 expression in HSPC.17,20 Therefore, we hypothesized that the TGF-−iPAI-1 axis is similarly operational in CML-LSC. In order to investigate the activation of TGF-−signaling in CML cells in vivo, we generated a CML-like myeloproliferative disease mouse model. Normal immature LSK cells obtained from fetal liver (FL) or adult BM were transduced with retrovirus carrying a human BCR/ABL-ires-GFP vector and transplanted into irradiated (9 Gy) recipient mice (Figure 1A). Consistent with previous reports,12,13 we found that BCR/ABL-transduced LSK cells efficiently induced CML-like disease in recipient mice by 12-20-day post transplantation (Figure 1B). In line with our previous reports, the highest levels of TGF-signal activation was confined to LSK cells, the majority of which are considered to be CML-LSC, as demonstrated by flow cytometric analysis for the phosphorylation of Smad-3 protein, a downstream signaling molecule of TGF-which forms a complex with Smad4 in the PAI-1 promoter and enhances transcriptional activation of PAI-1 gene (Figure 1C). A gradual increase in TGF activity in the CML-LSC fraction correlated with an increase in iPAI-1 expression within the same fraction (Figure 1C). The higher expression of iPAI-1 in CML-LSC was abolished by administration of TGF-inhibitor (LY364947, 10 mg/kg) (Figure 1D), indicating that the TGF-−iPAI-1 axis is indeed activated in CML-LSC.
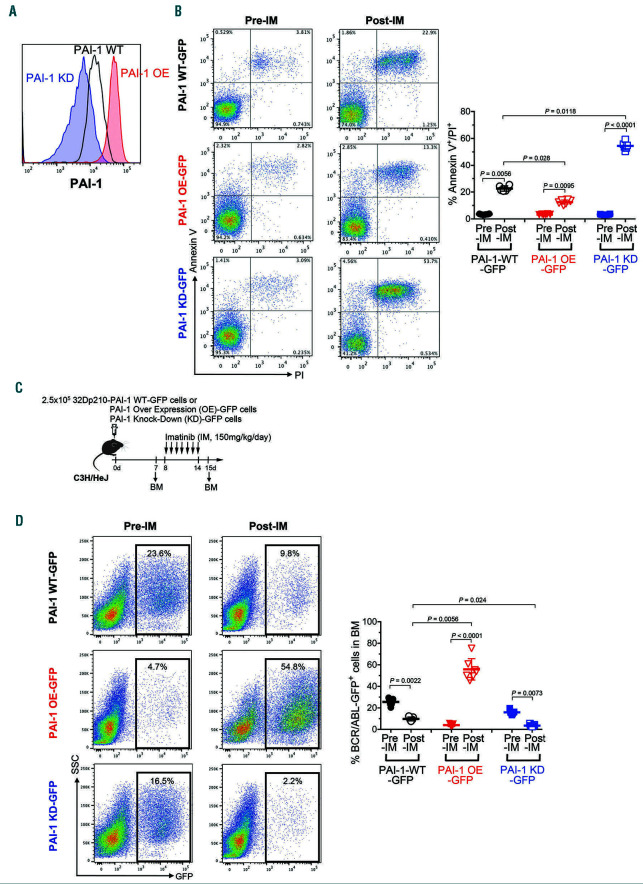
iPAI-1 protects CML cells from TKI treatment
HSPC are known to be remarkably resilient (in part) because they are kept in cell cycle dormancy through activation of TGF-signaling where iPAI-1 plays a pivotal role in retaining HSPC in their protective niche.17,20 Since we found that the TGF-−iPAI-1 axis is similarly activated in CML-LSC (Figure 1), we hypothesized that functional activation of the TGF-−iPAI-1 axis contributes to TKI resistance of CML-LSC by facilitating the supportive interaction within the niche. In order to test this hypothesis, we systemically investigated the influence of iPAI-1 on sensitivity of CML cells to TKI by using established CML-like cell lines (32D cells transduced with retrovirus carrying the human BCR/ABL-ires-GFP vector) that are genetically modified to enhance (PAI-1 overexpression [OE]) or nullify (PAI-1 knockout [KD]) the expression of iPAI-1 (Figure 2A). Twenty hours after being treated with IM in vitro, where extracellular fibrinolytic factors, such as tissue plasminogen activator, a PAI-1 target, did not exist, the apoptotic response of these cells was assessed by annexin V/PI staining. We found that a significantly higher percentage of PAI-1 OE cells survived IM treatment than parental 32D cells while a majority of PAI-1 KD cells underwent apoptosis (Figure 2B). This in vitro experiment clearly ruled out the involvement of extracellular anti-fibrinolytic function of PAI-1 in TKI resistance and suggested direct involvement of iPAI-1 in TKI resistance.
Next, we examined the effect of iPAI-1 overexpression on the sensitivity to TKI in vivo (Figure 2C). Seven days after transplantation, the presence of BCR/ABLGFP+ CML cells were confirmed in mice that received any of the genetically modified CML cells. IM was orally administered to these recipient mice for 7 consecutive days, and the percentage of GFP+CML cells in the BM was analyzed on the day after final IM administration. At day 7 of post transplantation, initial engraftment of PAI-1 KD CML cells in the BM was found to be slightly lower than that of WT CML cells. In addition, consistent with the in vitro findings described above, downregulation of iPAI-1 expression resulted in a significant reduction of CML cells in the BM of TKI-treated mice (Figure 2D). On the contrary, although PAI-1 OE CML cells were significantly less successful in initial engraftment compared to WT CML cells and PAI-1 KD CML cells, PAI-1 OE CML cells were resistant to TKI treatment and overgrew in the BM. These results confirmed that the intensity of iPAI-1 expression governs the susceptibility of CML cells to TKI treatment.
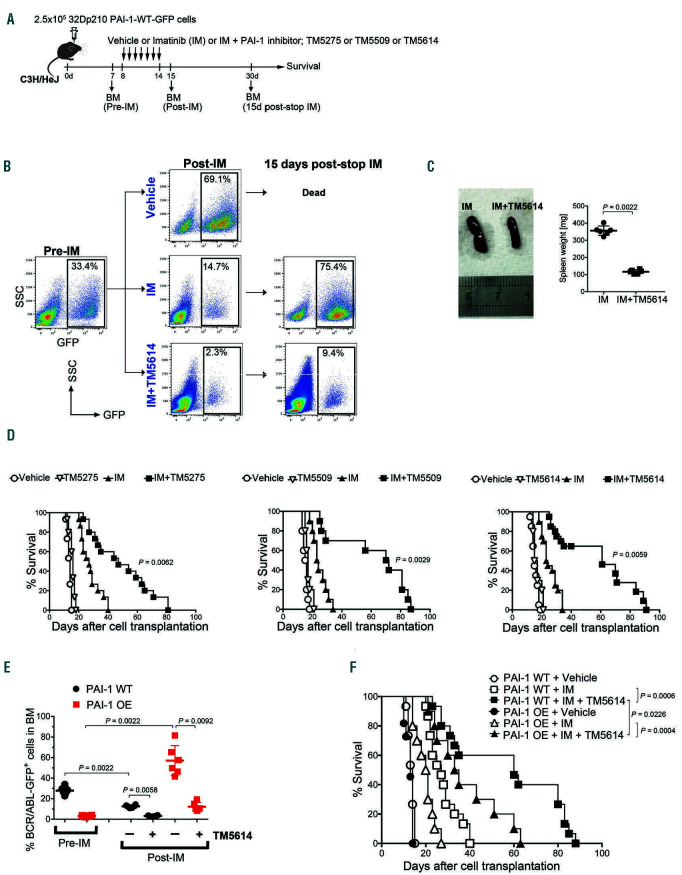
Pharmacological inhibition of iPAI-1 activity increases the susceptibility of CML cells to TKI treatment
The findings described above prompted us to investigate whether PAI-1 inhibitor administration can increase the susceptibility of CML cells to TKI treatment. CMLbearing mice created by transplantation of the parental BCR/ABL-ires-GFP-transduced 32D cells to non-irradiated mice were treated with either IM alone, a PAI-1 inhibitor alone or IM in combination with a PAI-1 inhibitor for 7 consecutive days and were observed for the following 40 days (Figure 3A). In this study, three different orallyactive, selective PAI-1 inhibitors, namely TM5275, TM5509 and TM5614 were used. The effect of the PAI-1 inhibitors was evaluated by assessing the percentage of BCR/ABL-GFP+CML cells in the BM and the overall survival of CML-bearing mice. Seven days after transplantation, all recipient mice developed a CML-like disease characterized by myeloid cell expansion in the BM, spleen and PB, accompanied by splenomegaly (Figure 3BC). Treatment with any one of the PAI-1 inhibitors alone did not markedly extend the survival of CML-bearing mice compared to the vehicle-treated CML mice (Figure 3D). Although treatment with IM by itself delayed disease onset, all IM-treated CML-bearing mice experienced relapse and died before the end of the observation period (Figure 3D). Interestingly, the combined treatment of IM plus any one of the PAI-1 inhibitors significantly inhibited the persistence of CML cells in the BM, reduced spleen size, and prolonged the survival of CML-bearing mice (Figure 3B-D). Furthermore, PAI-1 blockade combined with TKI was found to be effective in overcoming the TKI-resistance in CML-mice transplanted with PAI-1 OE CML cells (Figure 3E-F).
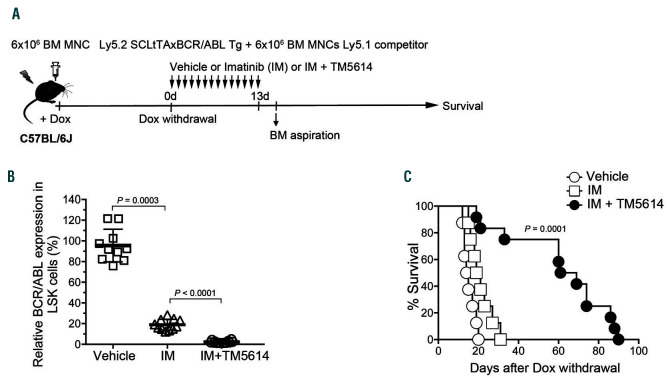
In order to further evaluate the potential therapeutic benefit of PAI-1 inhibitor treatment, we examined the effects of the PAI-1 inhibitor using a CML-induction mouse model, a model that closely resembles CML-development in human. In this previously described tetracycline (tet)–inducible CML mouse model,26,27 BM cells of Scl/Tal1-tTAxTRE-BCR/ABL doubletransgenic (Ly5.2; CD45.2) mice were transplanted to lethally irradiated (9 Gy) WT hosts, and the recipients were maintained in the presence of doxycycline at least for 2 months (Figure 4A). Within 3 weeks upon the withdrawal of doxycycline and induction of BCR/ABL expression, mice progressively developed CML-like disease. At the time of BCR/ABL induction, mice were treated with either IM alone, a PAI-1 inhibitor alone, or the combination of IM and a PAI-1 inhibitor for 14 consecutive days. On day 15, the expression of BCR/ABL in CML cells in the BM was determined by quantitative real-time PCR. IM treatment alone reduced the level of BCR/ABL–expression in the BM LSK fraction of CML cells to approximately 1/4 of saline treated mice, whereas combined treatment of IM plus the PAI-1 inhibitor reduced the expression of BCR/ABL in CML cells to barely detectable levels (Figure 4B). In addition, the overall survival of this CML-affected mice treated with IM plus the PAI-1 inhibitor was markedly extended (Figure 4C). These results are in accordance with our earlier experiments using genetically modified CML cell lines and BCR/ABL transduced LSK cells and indicate that inhibition of iPAI-1 activity increases the susceptibility of CML cells to TKI treatment.
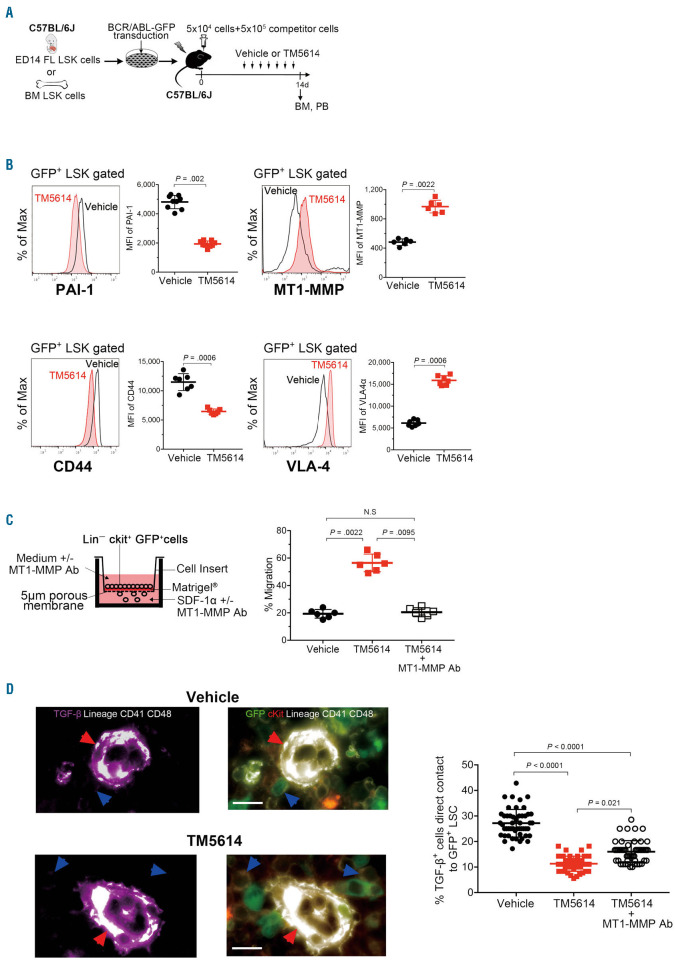
iPAI-1 blockade induces the dislocation of CML-LSC in the BM
We then sought to identify how iPAI-1 signaling influences the sensitivity of CML cells to TKI. Since the blockade of iPAI-1 causes detachment of HSPC from the niche,17,20 we hypothesized that iPAI-1 is similarly involved in the motility of CML-LSC in the BM. In order to test this hypothesis, we examined the expression of MT1-MMP, which has been shown to control the motility of HSPC,17–19 in CML-LSC derived from PAI-1 inhibitor treated mice. Mice were transplanted with normal FL LSK cells that were transduced with retrovirus carrying the human BCR/ABL-ires-GFP and were treated with a PAI-1 inhibitor for 7 consecutive days starting at day 7 post transplantation (Figure 5A). As expected, treatment with a PAI-1 inhibitor reduced the expression of iPAI-1 in the LSK fraction of BCR/ABL-GFP+ CML cells, which represent CML-LSC, and at the same time, increased the expression of MT1-MMP in the same fraction of cells (Figure 5B). Furthermore, iPAI-1 blockade altered the expression levels of CD44 and VLA-4, key adhesion/de-adhesion molecules known to determine the localization of hematopoietic cells within the BM14,30,32–34 (Figure 5B). Consistent with this in vivo observation, expression of CD44 and VLA-4 were altered in iPAI-1 OE and KO CML cells, confirming the link between the expression of adhesion/de-adhesion molecules and the iPAI-1 activity (Online Supplementary Figure S1). In order to confirm that iPAI-1 regulates the motility of CML-LSC through the action of MT1-MMP, we examined the directional motility of CML-LSC toward a chemokine gradient using a trans-reconstituted basement membrane (MatrigelTM) migration assay system. Lin–c-Kit+ immature CML cells isolated from PAI-1 inhibitor treated CML mice exhibited significantly higher trans-Matrigel migration activity compared to those of saline-treated mice (Figure 5C). Importantly, addition of anti-MT1-MMP neutralizing antibody to the culture abo-lished the enhanced migration activity of immature CML cells (Figure 5C), confirming the critical role of MT1-MMP in regulating the motility of CML-LSC. We therefore examined the effect of PAI-1 blockage in the localization of CML-LCS in vivo. BM sections were stained with antibodies against hematopoietic lineage markers (CD3, B220, Mac-1, Gr-1, Ter119, CD41, and CD48) and c-kit to identify CML-LSC and were simultaneously stained with antibody against TGF-to identify niche cells (Figure 5D, the fluorescence images in lower magnification are shown in the Online Supplementary Figure S2), and the sections were evaluated to determine the positional relationships between CML-LSC and niche cells. In PAI-1 inhibitor-treated mice, BCR/ABL-GFP+Lin–ckit+ CML-LSC were frequently found further away from TGF--expressing niche cells (Figure 5D), in contrast to vehicle-treated mice in which CML-LSC were often in contact with, or within close proximity to, TGF- -expressing niche cells (Figure 5D). Importantly, the administration of an anti-MT1-MMP neutralizing antibody counteracted the observed detachment of CML-LSC from niche cells in PAI-1 inhibitor-treated mice (Figure 5D). These results suggest that iPAI-1 activity is an important determinant of CML-LSC’ sensitivity to TKI, whereby controlling the MT1-MMP dependent retention of CML-LCS in the BM protective environment.
Figure 1.
TGF-−iPAI-1 signaling is activated in chronic myeloid leukemia - leukemic stem cells. (A) Schema for experiments. (B) Representative flow cytometric profiles of contribution of BCR/ABL-GFP+ cells to the myeloid (Mac-1+/Gr-1+) peripheral blood (PB) output post transplantation. (C) Representative flow cytometric profiles and mean fluorescent intensity (MFI) (n=6) for p-Smad3 and intracellular plasminogen activator inhibitor-1 (iPAI-1) expressions in freshly isolated BCR/ABL-GFP+ immature chronic myeloid leukemia (CML) cells in the bone marrow (BM). MFI of LSK: Lin–c-kit+Sca-1+; LS–K: Lin–c-kit+Sca–1–; LS–K–: Lin–c-kit–Sca-1–. (D) Representative flow cytometric profile and MFI for iPAI-1 expression in freshly isolated BCR/ABL-GFP+ immature CML cells in the BM of vehicle- or LY364947-treated mice (n=5). Data represent means ± standard deviation. Statistical significance was determined by Mann-Whitney unpaired t-test. P<0.001, by a Kruskal-Wallis test. TGF-: transforming growth factor-; BCR: breakpoint cluster region; ABL: Abelson kinase; GFP: green florescent protein; SSC: side scatter.
Figure 2.
iPAI-1 protects chronic myeloid leukemia cells from tyrosine kinase inhibitor treatment. (A) A representative flow cytometric profile for intracellular plasminogen activator inhibitor-1 (iPAI-1) expressions in PAI-1-overexpression (PAI-1 OE), PAI-1-knockdown (PAI-1 KD), or wild-type parental 32D p210 cells (PAI-1 WT). (B) Representative flow cytometric profiles and percentage of Annexin V+/PI+ population in PAI-1 OE, PAI-1 KD, or PAI-1 WT cells before imatinib (Pre-IM) and after imatinib (Post-IM) treatment in vitro (n=6). (C) Schema for in vivo experiments. (D) Representative flow cytometric profiles and percentages of leukemic cells in the bone marrow (BM) (n=7). Data represent means ± standard deviation. Statistical significance was determined by Mann-Whitney unpaired t-test. P<0.001, by a Kruskal-Wallis test. GFP: green fluorescent protein.
Figure 3.
Combined treatment with tyrosine kinase inhibitor plus PAI-1 inhibitor prolongs survival of chronic myeloid leukemia-bearing mice. (A) Schema for experiments. (B) Representative flow cytometric profiles for the percentage of chronic myeloid leukemia (CML) cells in the bone marrow (BM) at the indicated time points. (C) Analysis of spleen taken from imatinib (IM)- and IM plus plasminogen activator inhibitor-1 (PAI-1) inhibitor-treated mice (n=6). (D) Kaplan Meier survival curves of CML-bearing mice treated with saline (n=10), PAI-1 inhibitors (TM5275, TM5509, and TM5614) alone (n=10), IM alone (n=10), and IM plus PAI-1 inhibitor (n=15). (E) Percentages of leukemic cells in the BM (n=6). (F) Kaplan Meier survival curves of PAI-1 wild-type (PAI-1 WT) or PAI-1-overexpression (PAI-1 OE) CML cell-bearing mice treated with saline (n=0), IM alone (n=10), or IM plus PAI-1 inhibitor (TM5614) (n=10). Data represent means ± standard deviation. Statistical significance was determined by a log-rank non-parametric test (D, F) or Mann-Whitney unpaired t-test (E). P<0.001, by a Kruskal-Wallis test. SSC: side scatter.
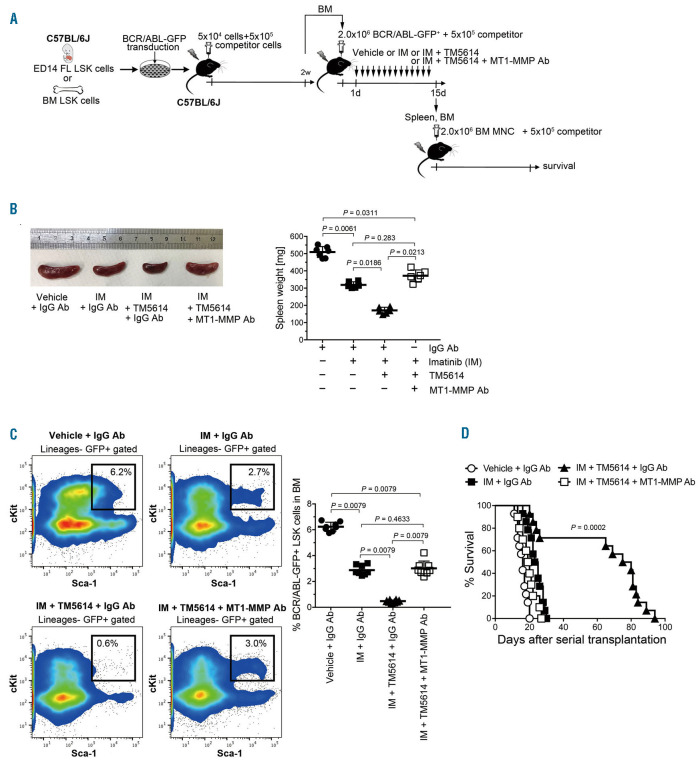
Blockade of iPAI-1 activity in combination with TKI efficiently eliminates CML-LSC
As shown earlier in this study that CML-LSC exhibited higher iPAI-1 expression (Figure 1), we focused on the effectiveness of iPAI-1 targeting therapy on primitive CML-LSC. Recipient mice that received BCR/ABL-GFP+ cells obtained from the BM of mice transplanted with human BCR/ABL-ires-GFP retrovirus transduced FL LSK cells were treated with IM alone or with IM plus a PAI-1 inhibitor for 14 consecutive days (Figure 6A). IM treatment alone reduced the percentage of BCR/ABL-GFP+ LSK cells in the BM approximately by half and mildly decreased the spleen size (Figure 6B-C). Notably, the combined treatment of IM plus a PAI-1 inhibitor diminished BCR/ABL-GFP+ LSK cell numbers in the BM and the size of spleen (Figure 6B-C).
Figure 4.
Blockade of iPAI-1 increases the sensitivity of chronic myeloid leukemia cells to tyrosine kinase inhibitor treatment. (A) Schema for experiments. (B) Quantitative real-time PCR analysis of the expression of BCR/ABL+ in bone marrow (BM) LSK cells of SCLtTAxBCR/ABL Tg mice that were treated with saline (n=10), imatinib (IM) alone (n=11), or IM plus plasminogen activator inhibitor-1 (PAI-1) inhibitor (TM5614) (n=12). (C) Kaplan Meier survival curves of SCLtTAxBCR/ABL Tg mice treated with saline (n=10), IM alone (n=10), or IM plus PAI-1 inhibitor (TM5614) (n=10). Data represent means ± standard deviation. Statistical significance was determined by Mann-Whitney unpaired t-test (B) or a log-rank non-parametric test (C). P<0.001, by a Kruskal-Wallis test. BCR: breakpoint cluster region; ABL: Abelson kinase: GFP: green fluorescent protein; LSK: Lineage (Lin)Sca1c-Kit.
Figure 5.
iPAI-1 blockade increases membrane type-1 metalloproteasedependent cellular motility. (A) Schema for experiments. (B) Representative flow cytometric profiles and mean fluorescent intensity (MFI) (n=6-9) for iPAI-1, MT1-MMP, CD44, and VLA-4 expressions in freshly isolated bone marrow (BM) BCR/ABL-GFP+ LSK cells of saline or PAI-1 inhibitor treated mice. (C) Percentages of migrated BCR/ABLGFP+ Lin−c-kit+ immature chronic myeloid leukemia (CML) cells in trans-Matrigel migration assay (n=6 each). Data represent means ± standard deviation. Statistical significance was determined by Mann-Whitney unpaired t-test. P<0.001, by a Kruskal-Wallis test. (D) Representative pictures of the BM cavity of vehicle- or TM5614-treated mice. BM sections were stained with antitransforming growth factor-(TGF-) (purple), anti-c-kit (red) and anti-lineage markers (white) antibodies. Red arrowheads indicate TGF--expressing niches. Blue arrow heads indicate BCR/ABLGFP+ Lin–c-kit+ CML cells. Bars represent 100 m. Graph indicates percentages of TGF--expressing niches closely contact to immature CML cells. More than 50 in random fields on a slide were counted for two independent experiments (n=4 each). Each dot represents % of contact cells in the one field. Statistical significance was determined by Mann-Whitney unpaired t-test. P<0.001, by a Kruskal-Wallis test. BCR: breakpoint cluster region; ABL: Abelson kinase: GFP: green fluorescent protein; LSK: Lineage (Lin)Sca1c-Kit L; MT1- MNP: membrane type-1 metalloprotease; Ab: antibody.
Next, we attempted to validate the rationale of PAI-1 inhibitor therapy for overcoming the IM resistance of CML-LSC using a serial BM transplantation assay system. Spleen and BM cells obtained from mice undergoing the drug treatment described above were transplanted to recipient mice. As expected, mice that received cells of saline-treated donor mice developed CML and died within 20 days post transplantation, indicating the persistence of CML-LSC. Even though IM treatment reduced BCR/ABL-GFP+ LSK cell numbers in the BM of donor mice by half, it did not protect recipient mice from relapse and all recipient mice died within 30 days. In contrast, more than 70% of mice that received cells from the donor mice that received the combined treatment survived until the end of the observation period (Figure 6D). In line with our in vitro findings, the effect of PAI-1 inhibitor on CML-LCS was completely abolished by the administration of a neutralizing antibody specific for MT1-MMP, indicating a critical role of this molecule in TKI sensitivity of CMLLSC (Figure 6B-D). These data confirmed that iPAI-1 blockade in combination with TKI effectively eliminates CML-LSC.
Figure 6.
Combined treatment with tyrosine kinase inhibitor plus PAI-1 inhibitor eradicates chronic myeloid leukemia - leukemic stem cells. (A) Schema for experiments. (B) Analysis of spleens taken from mice treated with saline, imatinib (IM) alone, or IM plus TM5614 in combination either with anti-MT1-MMP antibody or isotype-matched control immunoglobulin (n=6-7). (C) Representative flow cytometric profiles and percentage of chronic myeloid leukemia - leukemic stem cells (CMLLSC) in the bone marrow (BM) (n=9). (D) Kaplan Meier survival curves of serially transplanted mice (n=10-14). Data represent means ± standard devaition. Statistical significance was determined by Mann-Whitney unpaired t-test (B) or a log-rank non-parametric test (D). P<0.001, by a Kruskal-Wallis test. PAI-1: plasminogen activator inhibitor-1; GFP: green fluorescent protein.
Discussion
An effective strategy to eliminate cancer stem cells is critical in securing a complete cure of patients with cancers such as CML. The evidence that the TGF-signaling pathway plays an essential role in the maintenance of immature CML-LSC12,13 led us to investigate the involvement of iPAI-1 in the function of CML-LSC and their susceptibility to TKI. Our data unambiguously demonstrate that the forced expression of iPAI-1 in a CML cell line endows tumor cells with resistance to TKI treatment both in vitro and in vivo, which likely explains why iPAI-1- expressing immature CML-LSC are refractory to TKI treatment in the CML-bearing mice. This intimate association of TGF-−iPAI-1 with CML has led to suggest that TGF-−iPAI-1 axis itself contributes directly to malignant behavior, and that the inhibition of the TGF-−iPAI-1 axis is beneficial in treating CML. A study has shown that iPAI-1 is able to directly bind to caspase 3,35 thus influencing activation of the apoptotic pathways. Indeed, our in vitro analysis demonstrated that the level of iPAI-1 expression is inversely correlated with the cellular susceptibility to TKI treatment, indicating that iPAI-1 contributes to TKI resistance by negatively regulating apoptosis in leukemic cells. Consistent with this, it has recently been reported that PAI-1 inhibitors induce apoptosis in vitro in a variety of tumor cell lines through the activation of the intrinsic apoptotic pathway,36,37 suggesting that PAI-1 inhibitors possess intrinsic anti-cancer activity. The combined administration of imatinib plus a PAI-1 inhibitor markedly improved the therapeutic outcome of TKI as evidenced by a reduction in the number of CML cells in the BM, reduced spleen size, and prolonged survival in a mouse model of CML. Furthermore, pharmacological blockade of iPAI-1 in combination with TKI effectively eliminated CML-LSC in the BM, which in turn prevented the recurrence of CML-like disease in recipients of serial transplantation experiments.
HSPC are localized in the niche where local factors that keep them in cell-cycle dormancy, such as TGF-, are abundantly present. LSC co-opt the HSPC BM niche to gain survival benefits by hijacking the molecular physiological mechanisms utilized by HSPC.15,28,29 Therefore, disruption of LSC localization has been proposed to be an effective means to eradicate LSC. Recently, we have shown that functional inhibition of iPAI-1 increased MT1- MMP-dependent cellular motility and caused a detachment of HSPC from the niche. In this report, we demonstrated that the therapeutic effect of a PAI-1 inhibitor appears to depend on the activity of MT1-MMP. Although the involvement of MT1-MMP has been implicated in physiology and pathophysiology of many types of cells, its exact role(s) has not been determined. One of the main functions of MT1-MMP is to break down pericellular matrix proteins. It also activates pro-MMP-2, which then activates other proteases such as MMP-9 and MMP-13. The interplay of these multiple protease controls motility of both normal and malignant cells. In addition, MT1- MMP can promote cellular motility by breaking down membrane-bound adhesion molecules necessary for niche-anchoring, such as CD44, which then triggers the induction of molecules involved in hematopoietic cell trafficking, such as VLA4.17,18 CD44 and VLA-4 have been shown to play key roles in homing and engraftment of LSC.14,30,32–34 Consistent with this, the present study indicates that CML cells overexpressing iPAI-1 (where the expression of MT1-MMP is consequently suppressed17), manifest poor migration activity in the BM environment. Furthermore, analogous to our HSPC study, treatment of CML mice with a PAI-1 inhibitor increased MT1-MMP activity and altered the surface expression of CD44 and VLA-4 on CML-LSC, which resulted in enhanced motility of CML-LSC. This altered expression of adhesion/deadhesion molecules appear to disrupt the interaction between CML-LSC and their protective environment, which renders CML-LSC susceptible to TKI therapy. In fact, it has been reported that blockade of CD44 and VLA- 4 markedly reduced LSC engraftment and prolonged the survival of LSC-transplanted mice.14,30,33,34,38 Thus, MT1- MMP activity appears to determine the therapeutic sensitivity of LSC. Taken together, these findings suggest that, besides its well-known role in cell cycle regulation, TGF-signaling, in which iPAI-1-MT1-MMP axis plays an integral part of its coordinated circuitry, controls the motility of both normal and malignant stem cells, thereby protecting them from environmental stimuli. In line with our findings, several studies have proposed mobilization of CML-LSC from the niche as a measure to counteract TKI resistance, using granulocyte-colony stimulating factor (G-GSF)39,40 or inhibitors for C-X-C motif chemokine receptor (CXCR) 4,41,42 E-selectin,43 or TGF-,13 further exploring the therapeutic potential of this approach. The present study also demonstrates that selective upregulation of the iPAI-1-MT1-MMP axis in CML-LSC provides a newly recognized mechanism of drug-resistance and that modulation of this signaling pathway overcomes TKI-resistance in CML mouse. The evidence we provide in this study has led us to suggest that iPAI-1 signaling contributes directly to pathology of cancers beyond the scope of this study, and that inhibition of the TGF-−iPAI- 1 axis can become an effective approach to treat a wide variety of cancers.
We have developed a low molecular weight synthetic inhibitor of PAI-1, TM5275 and a series of analogues with improved pharmacological and toxicological properties, including TM5509 and TM5614.44,45 A number of preclinical studies have demonstrated that this series of compounds is capable of affecting a number of metabolic, fibrotic, aging-related disorders, as well as hematopoietic regeneration.46–50 In this study, we provide the first evidence that inhibition of iPAI-1 can be of therapeutic benefit in the treatment of leukemia. iPAI-1 has almost identical roles in retaining normal HSC and LSC in the niche. In that sense, when CML patients are treated with a PAI-1 inhibitor, both HSC and LSC are supposed to be released from the niche. In a physiological setting, HSC are believed to be in a cycle of being released from and returning to the niche.17,20 Even in the presence of a PAI-1 inhibitor plus TKI, HSC should be able to return to the niche because they are refractory to TKI. On the contrary, TKI specifically targets CML cells once they are released from the niche. In fact, the PAI-1 inhibitor used in this study, has successfully completed a phase I trial without any noticeable adverse effects, including myelosupplession, and has advanced to the phase II trial. In summary, this study describes a novel role of iPAI-1 in drug-resistance in CML and suggests that the selective therapeutic targeting of this serpin may be of value in the treatment of patients with this malignant hematopoietic disorder.
Supplementary Material
Funding Statement
FundingTY, HK, and KA were supported by a grant-in-aid for Scientific Research and Strategic Research Foundation Grantaided Project for private universities from the Ministry of Education, Culture, Sports, Science and Technology, Japan (grant number: 15H04301 and 17H03072); TY was also supported by Project Research from the Tokai University School of Medicine, Takeda Science Foundation, and The Science Research Promotion Fund from The Promotion and Mutual Aid Corporation for private schools of Japan. AAI was supported by grant-in aid for young scientists from the Ministry of Education, Culture, Sports, Science and Technology, Japan (grant number: 18K14702). TY, TM, and KA were supported by the Project for Development of Innovative Research on Cancer Therapeutics (PDIRECT) and the Adaptable and Seamless Technology Transfer Program through Target-driven R&D (A-STEP), from the Japanese Agency for Medical Research and Development (grant number: 14533192, 12103262, and 14529205).
References
- 1.Nowell PC, Hungerford DA. Chromosome studies on normal and leukemic human leukocytes. J Natl Cancer Inst. 1960;25:85-109. [PubMed] [Google Scholar]
- 2.Rowley JD. Letter: A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature. 1973;243(5405):290-293. [DOI] [PubMed] [Google Scholar]
- 3.Bartram CR, de Klein A, Hagemeijer A, et al. Translocation of c-ab1 oncogene correlates with the presence of a Philadelphia chromosome in chronic myelocytic leukaemia. Nature. 1983;306(5940):277-280. [DOI] [PubMed] [Google Scholar]
- 4.Druker BJ, Guilhot F, O’Brien SG, et al. Fiveyear follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408-2417. [DOI] [PubMed] [Google Scholar]
- 5.Hochhaus A, Larson RA, Guilhot F, et al. Long-term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376(10):917-927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huntly BJP, Gilliland DG. Leukaemia stem cells and the evolution of cancer-stem-cell research. Nat Rev Cancer. 2005;5(4):311-321. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia R, Holtz M, Niu N, et al. Persistence of malignant hematopoietic progenitors in chronic myelogenous leukemia patients in complete cytogenetic remission following imatinib mesylate treatment. Blood. 2003; 101(12):4701-4707. [DOI] [PubMed] [Google Scholar]
- 8.Corbin AS, Agarwal A, Loriaux M, et al. Human chronic meyloid leukemia stem cells insensitive to imatinib despite inhibition of BCR-ABL activity. J Clin Invest. 2011; 121(1):396-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3(7):730-737. [DOI] [PubMed] [Google Scholar]
- 10.Yamazaki S, Iwama A, Takayanagi S, Eto K, Ema H, Nakauchi H. TGF-as a candidate bone marrow niche signal to induce hematopoietic stem cell hibernation. Blood. 2009; 113(6):1250-1256. [DOI] [PubMed] [Google Scholar]
- 11.Yamazaki S, Ema H, Karlsson G, et al. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell. 2011;147(5):1146-1158. [DOI] [PubMed] [Google Scholar]
- 12.Naka K, Hoshii T, Muraguchi T, et al. TGF- -FOXO signalling maintains leukaemia-initiating cells in chronic myeloid leukaemia. Nature. 2010;463(7281):676-680. [DOI] [PubMed] [Google Scholar]
- 13.Naka K, Ishihara K, Jomen Y, et al. Novel oral transforming growth factor-signaling inhibitor EW-7197 eradicates CML-initiating cells. Cancer Sci. 2016;107(2):140-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krause DS, Lazarides K, von Andrian UH, Van Etten RA. Requirement for CD44 in homing and engraftment of BCR-ABLexpressing leukemic stem cells. Nat Med. 2006;12(10):1175-1180. [DOI] [PubMed] [Google Scholar]
- 15.Krause DS, Fulzele K, Catic A, et al. Differential regulation of myeloid leukemias by the bone marrow microenvironment. Nat Med. 2013;19(11):1513-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guarnerio J, Mendez LM, Asada N, et al. A non-cell-autonomous role for Pml in the maintenance of leukemia from the niche. Nat Commun. 2018;9(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yahata T, Ibrahim AA, Muguruma Y, et al. TGF-–induced intracellular PAI-1 is responsible for retaining hematopoietic stem cells in the niche. Blood. 2017;130(21):2283-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vagima Y, Avigdor A, Goichberg P, et al. MT1-MMP and RECK are involved in human CD34+ progenitor cell retention, egress, and mobilization. J Clin Invest. 2009; 119(3):492-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shirvaikar N, Marquez-Curtis LA, Shaw AR, Turner AR, Janowska-Wieczorek A. MT1- MMP association with membrane lipid rafts facilitates G-CSF-induced hematopoietic stem/progenitor cell mobilization. Exp Hematol. 2010;38(9):823-835. [DOI] [PubMed] [Google Scholar]
- 20.Ibrahim AA, Yahata T, Muguruma Y, Miyata T, Ando K. Blockade of plasminogen activator inhibitor-1 empties bone marrow niche sufficient for donor hematopoietic stem cell engraftment without myeloablative conditioning. Biochem Biophys Res Commun. 2019;516(2):500-505. [DOI] [PubMed] [Google Scholar]
- 21.Ghosh AK, Vaughan DE. PAI-1 in tissue fibrosis. J Cell Physiol. 2012;227(2):493-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Placencio VR, DeClerck YA. Plasminogen activator inhibitor-1 in cancer: rationale and insight for future therapeutic testing. Cancer Res. 2015;75(15):2969-2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van De Craen B, Declerck PJ, Gils A. The biochemistry, physiology and pathological roles of PAI-1 and the requirements for PAI- 1 inhibition in vivo. Thromb Res. 2012; 130(4):576-585. [DOI] [PubMed] [Google Scholar]
- 24.Yamaoka N, Murano K, Kodama H, et al. Identification of novel plasminogen activator inhibitor-1 inhibitors with improved oral bioavailability: structure optimization of Nacylanthranilic acid derivatives. Bioorg Med Chem Lett. 2018;28(4):809-813. [DOI] [PubMed] [Google Scholar]
- 25.Daley GQ, Van Etten RA, Baltimore D. Induction of chronic myelogenous leukemia in mice by the P210bcr/abl gene of the Philadelphia chromosome. Science. 1990; 247(4944):824-830. [DOI] [PubMed] [Google Scholar]
- 26.Huettner CS, Zhang P, Van Etten RA, Tenen DG. Reversibility of acute B-cell leukaemia induced by BCR–ABL1. Nat Genet. 2000;24(1):57-60. [DOI] [PubMed] [Google Scholar]
- 27.Koschmieder S, Göttgens B, Zhang P, et al. Inducible chronic phase of myeloid leukemia with expansion of hematopoietic stem cells in a transgenic model of BCR-ABL leukemogenesis. Blood. 2005;105(1):324-334. [DOI] [PubMed] [Google Scholar]
- 28.Saito Y, Uchida N, Tanaka S, et al. Induction of cell cycle entry eliminates human leukemia stem cells in a mouse model of AML. Nat Biotechnol. 2010;28(3):275-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Medyouf H. The microenvironment in human myeloid malignancies: emerging concepts and therapeutic implications. Blood. 2017;129(12):1617-1626. [DOI] [PubMed] [Google Scholar]
- 30.Jin L, Hope KJ, Zhai Q, Smadja-Joffe F, Dick JE. Targeting of CD44 eradicates human acute myeloid leukemic stem cells. Nat Med. 2006;12(10):1167-1174. [DOI] [PubMed] [Google Scholar]
- 31.Neering SJ, Bushnell T, Sozer S, et al. Leukemia stem cells in a genetically defined murine model of blast-crisis CML. Blood. 2007;110(7):2578-2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lapidot T, Petit I. Current understanding of stem cell mobilization. Exp Hematol. 2002; 30(9):973-981. [DOI] [PubMed] [Google Scholar]
- 33.Lapid K, Glait-Santar C, Gur-Cohen S, Canaani J, Kollet O, Lapidot T. Egress and mobilization of hematopoietic stem and progenitor cells: a dynamic multi-facet process. Cambridge, MA: The Stem Cell Research Community, StemBook.; p1-37. [PubMed] [Google Scholar]
- 34.Krause DS, Lazarides K, Lewis JB, von Andrian UH, Van Etten RA. Selectins and their ligands are required for homing and engraftment of BCR-ABL1+ leukemic stem cells in the bone marrow niche. Blood. 2014; 123(9):1361-1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen Y, Kelm RJ, Budd RC, Sobel BE, Schneider DJ. Inhibition of apoptosis and caspase-3 in vascular smooth muscle cells by plasminogen activator inhibitor type-1. J Cell Biochem. 2004;92(1):178-188. [DOI] [PubMed] [Google Scholar]
- 36.Placencio VR, Ichimura A, Miyata T, DeClerck YA. Small molecule inhibitors of plasminogen activator inhibitor-1 elicit antitumorigenic and anti-angiogenic activity. PLoS One. 2015;10(7):e0133786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mashiko S, Kitatani K, Toyoshima M, et al. Inhibition of plasminogen activator inhibitor-1 is a potential therapeutic strategy in ovarian cancer. Cancer Biol Ther. 2015; 16(2):253-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lapidot T, Petit I. Current understanding of stem cell mobilization: the roles of chemokines, proteolytic enzymes, adhesion molecules, cytokines, and stromal cells. Exp Hematol. 2002;30(9):973-981. [DOI] [PubMed] [Google Scholar]
- 39.Borthakur G, Kantarjian H, Wang X, et al. Treatment of core-binding-factor in acute myelogenous leukemia with fludarabine, cytarabine, and granulocyte colony-stimulating factor results in improved event-free survival. Cancer. 2008;113(11):3181-3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holtz M, Forman SJ, Bhatia R. Growth factor stimulation reduces residual quiescent chronic myelogenous leukemia progenitors remaining after imatinib treatment. Cancer Res. 2007;67(3):1113-1120. [DOI] [PubMed] [Google Scholar]
- 41.Uy GL, Rettig MP, Motabi IH, et al. A phase 1/2 study of chemosensitization with the CXCR4 antagonist plerixafor in relapsed or refractory acute myeloid leukemia. Blood. 2012;119(17):3917-3924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beider K, Darash-Yahana M, Blaier O, et al. Combination of imatinib with CXCR4 antagonist BKT140 overcomes the protective effect of stroma and targets CML in vitro and in vivo. Mol Cancer Ther. 2014; 13(5):1155-1169. [DOI] [PubMed] [Google Scholar]
- 43.Godavarthy PS, Kumar R, Herkt SC, et al. The vascular bone marrow niche influences outcome in chronic myeloid leukemia via the E-selectin - SCL/TAL1 - CD44 axis. Haematologica. 2020;105(1):136-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Izuhara Y, Takahashi S, Nangaku M, et al. Inhibition of plasminogen activator inhibitor-1: its mechanism and effectiveness on coagulation and fibrosis. Arterioscler Thromb Vasc Biol. 2008;28(4):672-677. [DOI] [PubMed] [Google Scholar]
- 45.Izuhara Y, Yamaoka N, Kodama H, et al. A novel inhibitor of plasminogen activator inhibitor-1 provides antithrombotic benefits devoid of bleeding effect in nonhuman primates. J Cereb Blood Flow Metab. 2010; 30(5):904-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eren M, Boe AE, Murphy SB, et al. PAI-1-regulated extracellular proteolysis governs senescence and survival in Klotho mice. Proc Natl Acad Sci U S A. 2014;111(19):7090-7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boe AE, Eren M, Murphy SB, et al. Plasminogen activator inhibitor-1 antagonist TM5441 attenuates Nω-nitro-L-arginine methyl ester-induced hypertension and vascular senescence. Circulation. 2013; 128(21): 2318-2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pelisch N, Dan T, Ichimura A, et al. Plasminogen activator inhibitor-1 antagonist TM5484 attenuates demyelination and axonal degeneration in a mice model of multiple sclerosis. PLoS One. 2015;10(4): e0124510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ibrahim AA, Yahata T, Onizuka M, et al. Inhibition of plasminogen activator inhibitor type-1 activity enhances rapid and sustainable hematopoietic regeneration. Stem Cells. 2014;32(4):946-958. [DOI] [PubMed] [Google Scholar]
- 50.Eren M, Place AT, Thomas PM, Flevaris P, Miyata T, Vaughan DE. PAI-1 is a critical regulator of FGF23 homeostasis. Sci Adv. 2017;3(9):e1603259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.