Abstract
Background:
To investigate whether closed-loop systems under bispectral index anesthesia depth monitoring can reduce the intraoperative propofol dosage.
Methods:
All randomized controlled trials (RCTs) on reducing propofol dosage under closed-loop systems were collected, and the literature was screened out, the abstracts and full texts were carefully read, and the references were tracked, data extraction and quality evaluation were conducted on the included research, and the RevMan5.3 software was used for meta-analysis. The main results were propofol and the incidence of adverse reactions such as hypertensive hypotension and postoperative cognitive dysfunction. A total of 879 cases were included in 8 articles, including 450 occurrences in the closed-loop system group and 429 cases in the open-loop system group.
Results:
Compared with manual control, closed-loop systems under bispectral index anesthesia depth monitoring reduced the dose of propofol (MD: −0.62, 95% CI: −1.08–−0.16, P = .008), with heterogeneity (I2 = 80%). Closed-loop systems significantly reduced the incidence of abnormal blood pressure (MD: −0.02, 95%CI: −0.05–0.01, P = .15, I2 = 74%) and postoperative cognitive dysfunction (MD: −0.08, 95% CI: −0.14 −0.01, P = .02, I2 = 94%).
Conclusion:
Bispectral index monitoring of propofol closed-loop target-controlled infusion system can reduce the amount of propofol, reduce the incidence of adverse reactions such as hypertensive or hypotension and postoperative cognitive dysfunction.
Keywords: closed-loop systems, bispectral index, propofol, meta-analysis
1. Introduction
The bispectral index mainly reflects the excited or inhibited state of the cerebral cortex and the information of sedation and hypnosis, which is not only closely related to healthy physiological sleep but also can well monitor the sedative components in the depth of anesthesia.[1–3] The appropriate depth of anesthesia is beneficial to the perioperative period's safety and the reduction of postoperative complications.[4] Target - controlled infusion (TCI) is divided into open - loop systems and closed-loop systems. Open-loop systems are that the anesthesiologist adjusts the infusion speed or target concentration of the drug according to his own clinical experience, to maintain a certain depth of anesthesia, likely to cause too deep or too shallow anesthesia.[5] The closed-loop system connects BIS and other anesthesia depth detectors to the computer executing TCI into a system that automatically adjusts the target concentration and independently forms a closed feedback loop. Therefore, we believe that the intravenous anesthesia closed-loop controlled drug delivery system guided by the bispectral index will be widely used in anesthesia. Closed-loop propofol systems have been used in general anesthesia, sedative anesthesia, and combined anesthesia with other anesthesia methods. However, long-term heavy use of propofol can lead to propofol infusion syndrome, especially in children.[6] The closed-loop system of propofol can avoid too deep anesthesia, reduce the use of propofol, and make the use of anesthesia personalized.
Propofol closed-loop systems can maintain a stable depth of anesthesia, avoid too deep or too shallow anesthesia, and reduce the incidence of postoperative delirium and cognitive dysfunction. The disadvantages of closed-loop systems of propofol are due to the influence of various factors on the double frequency index of EEG and the delay of feedback. However, whether the total dose of propofol is related to the use of the closed-loop system is controversial. Nevertheless, so far, the use of propofol closed-loop systems has been controversial. Although a number of randomized clinical trials have been published comparing BIS - guided closed - loop and open - loop systems, there has been no meta-analysis to explore the advantages of propofol closed-loop anesthesia. To determine the applicability of the propofol closed-loop methods, a systematic review of the previously published randomized controlled trials was conducted.[7]
2. Methods
2.1. Search strategy
We first searched several databases and then devised a search strategy for specific sources in consultation with information experts. The search was conducted to identify articles published before 2020, preferably in the last 5 years, using electronic sources MEDLINE, CINAHL, the Cochrane library (systematic reviews and trials), and EMBASE. Keywords such as “bispectral index,” “closed-loop systems,” “propofol,” and their synonyms were used in different combinations, and duplicates were removed. The search criteria (in titles, abstracts, and/or all fields) were as follows:
-
1.
closed-loop system;
-
2.
closed-loop control;
-
3.
closed-loop anesthesia control;
-
4.
manual;
-
5.
automated;
-
6.
bispectral index;
-
7.
(7)propofol;
-
8.
Randomized Controlled Trial;
-
9.
1 OR 2 OR 3 OR 4 OR 5 AND 6 AND 7 AND 8.
Furthermore, to ensure that all relevant literature was collected, we manually searched the references of eligible articles. This study is a systematic review and meta-analysis and is a summary of previous literature. Therefore, ethical approval from the Ethics Committee is not required. Patient consent is not involved in this article.
2.2. Selection criteria
2.2.1. Inclusion criteria
-
1.
Published comparative study on closed-loop systems and open-loop systems of propofol under the guidance of BIS;
-
2.
The study of all by intravenous anesthesia;
-
3.
The included studies were randomized controlled trials and included at least 2 groups, namely the BIS-guided propofol closed-loop system group (no limitation on equipment and pharmaceutical model, plasma TCI or effector compartment TCI) and the propofol open-loop system group (no restriction on infusion algorithm).
-
4.
Languages included in the research are limited to Chinese and English.
2.2.2. Exclusion criteria
-
1.
The study of intravenous anesthesia combined with inhalation anesthesia;
-
2.
Unintubated study of general anesthesia;
-
3.
Reviews, abstracts, conference proceedings, letters to the editor, meta-analyses, case reports, and retrospective and preliminary studies.
2.2.3. Data extraction and quality assessment
Two researchers searched the literature based on the inclusion and exclusion criteria above and then extracted data from all the included articles, including publication time, first author name, geographical area, subject age, number of cases, and results, tabulated and analyzed the extracted data.[8] Researchers read the original literature and visited the clinical trial public management platform and clinical trial registry to obtain data. If we encounter documents outside of English and China, we will use Google and other translation software for literature and data translation, or contact the corresponding author of the article to understand the original data. In the case that the data could not be publicly stored, researchers contacted the corresponding author of the article to get the original data researchers needed. Cochrane review system was used to evaluate the quality of the included studies.[9] Cochrane evaluation system consists of the actual contents of bias such as allocation concealment, random sequence generation, blind method of outcome evaluation, blind method of participants and personnel, selective report, incomplete result data, and so on, which can objectively and comprehensively evaluate various biases in the study.
2.2.4. Statistical analysis
Data as median and range are converted to mean and SD, following a published formula.[34] We calculated MD and 95% CI to summarize the heterogeneity test of continuous data using either the Chi-Squared test or the Cochran-based I2 test.[10] When significant heterogeneity (I2 > 50%) was observed, a random effect model was used. Otherwise, the fixed-effect model was used for meta-analysis. Propofol dosage, the incidence of hypertension or hypotension, and the impact of postoperative cognitive impairment were determined in each eligible study. The effect of closed-loop systems and open-loop systems on anesthesia of patients with different operation duration was analyzed in a subgroup. To evaluate the stability of the results, we conducted a sensitivity analysis by removing each one study at a time. For all the reviews, a P value of less than .05 was considered statistically significant.
3. Results
3.1. Study selection
The process of searching, screening, and study selection is summarized in Figure 1. Our researches found 1169 articles through database searching (Pubmed = 349, Medline = 131, Web of Science = 122, Embase = 127, Cochrane Library = 134, Ovid = 32, Springer = 44, CKNI = 155, WanFang Data = 75). What is more, 245 additional articles were identified through other sources. After removing duplicates (n = 654) and articles not satisfying the inclusion criteria (n = 577), 183 articles were assessed for eligibility. One hundred seventy five articles were removed because they were not RCT, and the data reported were incomplete. Finally, 8 studies were included in qualitative sysnthesis.[11–18]
Figure 1.
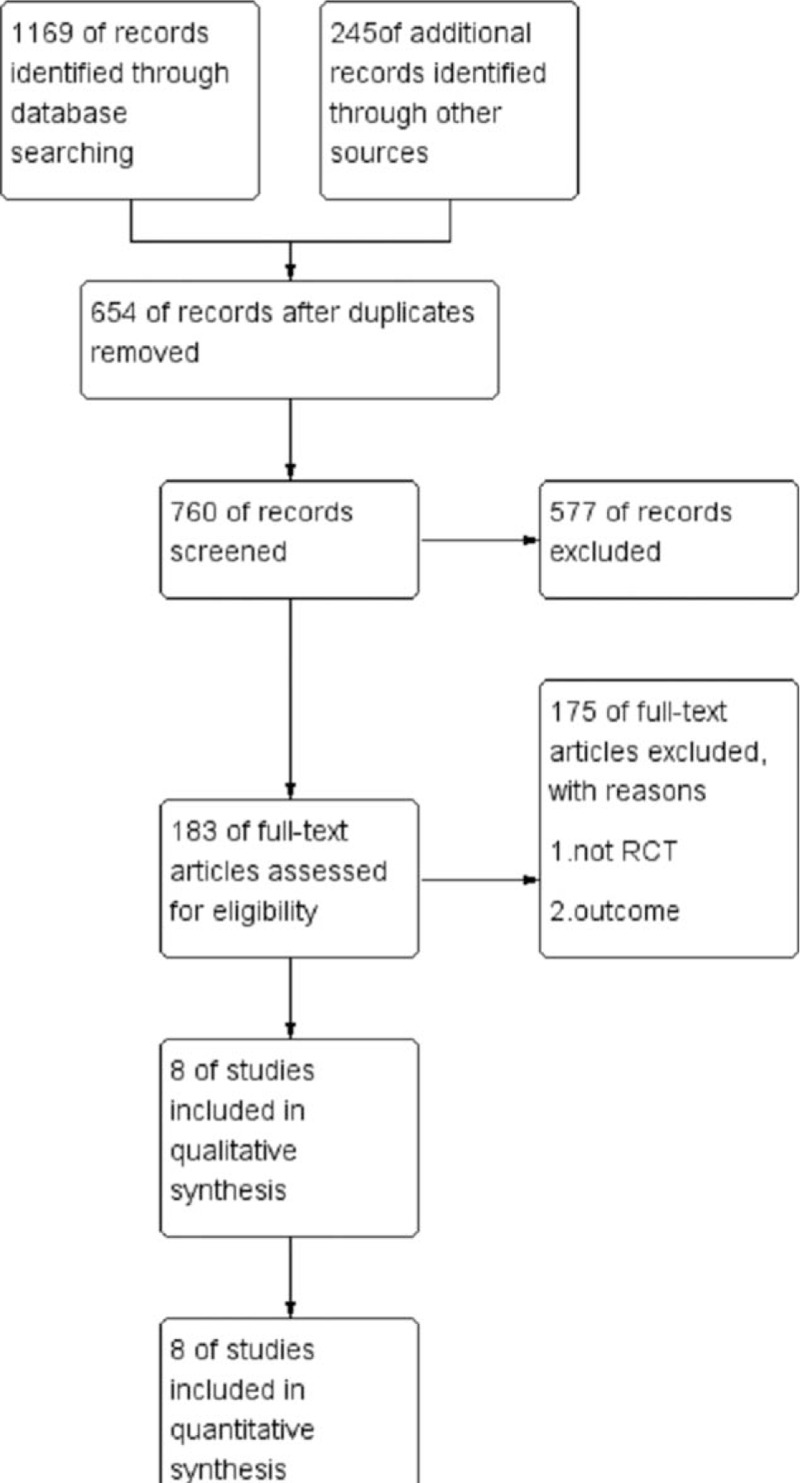
The flow chart showing the process of study selection and the retrieved results.
3.2. Study characteristics
The characteristics of the selected studies are summarized in Table 1.[11–18] In these 8 articles, 2 were multicenter studies.[12,15] A total of 8 sections, including 879 patients, included 450 patients in the closed-loop system group and 429 patients in the manually controlled open-loop system group. The quality of these articles was assessed using the Cochrane manual evaluation criteria, as shown in Figure 2. All RCTs employed BIS as guidance for experiment groups. The majority of RCTs included adults (18–80 years), except for 1 RCT conducted by Louvet that included elective patients aged 4 to 14. Patients from 2 studies underwent short-time surgery, such as ear, nose and throat surgery, ophthalmic surgery, and dermatologic surgery.[13,16] Whereas; patients from 2 studies underwent long-time surgery, such as liver transplantation surgery and open cardiac surgery.[11,14]
Table 1.
The characteristics of the selected studies.
| Study | Patient recruitment | Country | Sample size | Age (years) | Study design | Surgery |
| Cao 2017 | January 2014–December 2015 | China | 60 | 40–60 | RCT | liver transplantation surgery |
| Joosten 2019 | May 2017–February 2018. | Belgium | 89 | >60 | RCT | noncardiac surgery |
| Louvet 2016 | March 2006–February 2007. | France | 72 | 4–14 | RCT | middle ear surgery |
| Mahajan 2017 | January 2014–November 2014 | India | 40 | 18–65 | RCT | open cardiac surgery |
| Puri 2016 | January 2010–September 2012 | India | 242 | 18–60 | RCT | nonthoracic/nonvascular/non-neurosurgical surgery |
| Rüsch 2018 | February 2012–April 2013 | Germany | 235 | 18–80 | RCT | ear, nose and throat surgery, Ophthalmic surgery, and dermatologic surgery |
| Yong 2017 | January 2016–August 2016 | China | 60 | 65–75 | RCT | Gastrointestinal tumor resection surgery |
| Zhou 2018 | January 2014–November 2016 | China | 81 | 65–75 | RCT | colon carcinoma radical surgery |
Figure 2.
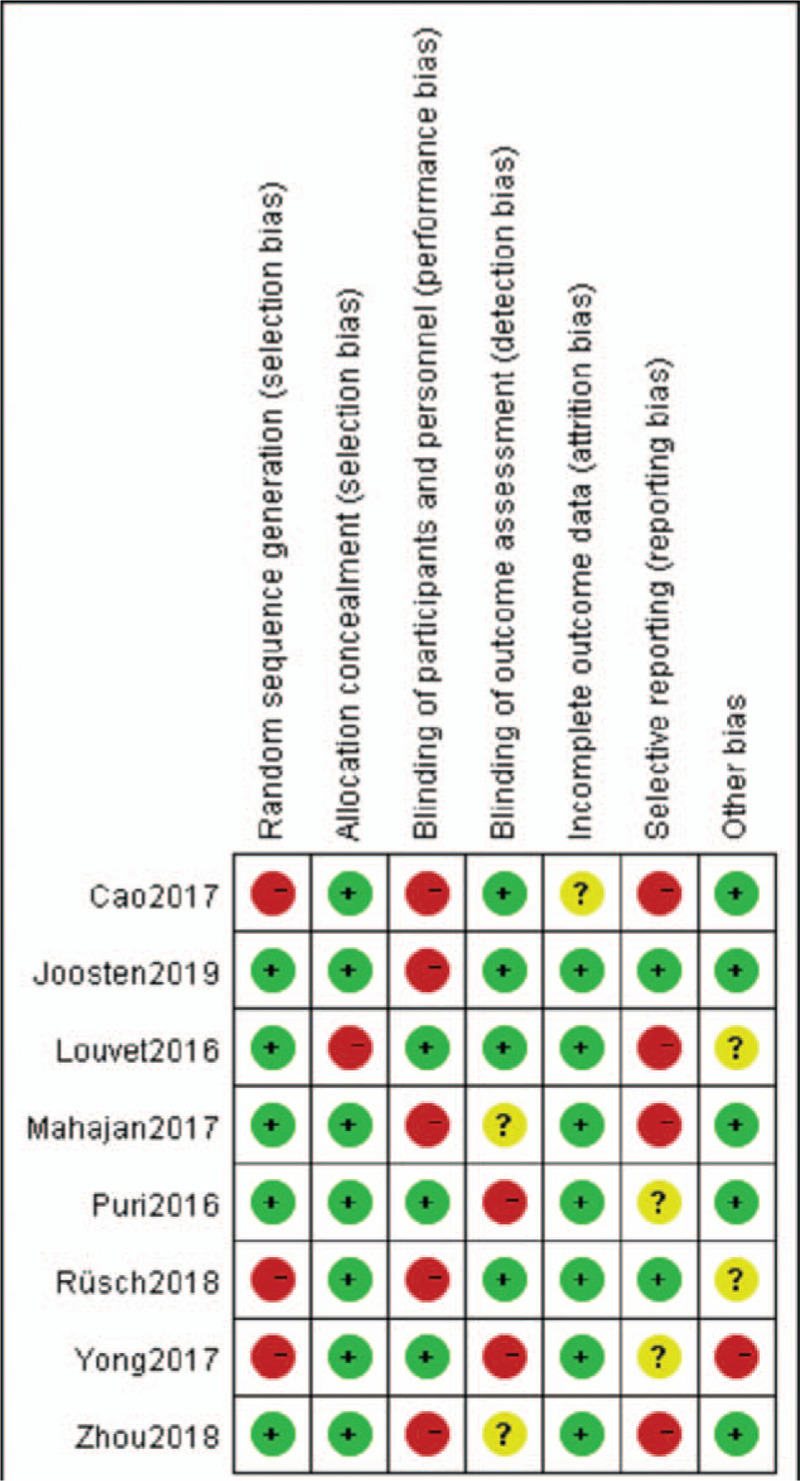
Sensitivity and specificity of the included studies.  represents a low risk of bias;
represents a low risk of bias;  stands for unclear risk of bias;
stands for unclear risk of bias;  represents a high risk of bias.
represents a high risk of bias.
3.3. Primary analysis
Our primary analyses aimed to compare the effect of closed-loop systems with open-loop systems. Our primary outcome was to evaluate the propofol dosage of automated control versus manual control (MD: −0.62, 95%CI: −1.08–−0.16, P = .008, Fig. 3), with heterogeneity (I2 = 80%). Compared with manual control, BIS-guided automated systems decreased the dosage of propofol. Three trials (2, 5, 7) reported the incidence of hypertension or hypotension as the outcome. Hypertension or hypotension is when a patients blood pressure during anesthesia is 20 percent higher or lower than when they enter the surgery room.[19] The pooled MD for the incidence of hypertension or hypotension from 3 studies (closed-loop system group versus open-loop system group) was −0.02 (95%, CI: −0.05–0.01, P = .15, Fig. 4), with heterogeneity (I2 = 74%). A total of 4 literatures[11,12,17,18] reported POCD-associated results. Using closed-loop systems during intravenous anesthesia significantly reduced postoperative cognitive dysfunction (MD: −0.08, 95%, CI: −0.14 –0.01, P = .02, Fig. 5), with significant heterogeneity among the studies (I2 = 94%). The results showed that the difference in the 3 outcomes mentioned above between the closed-loop system group and the open-loop system group was statistically significant.
Figure 3.
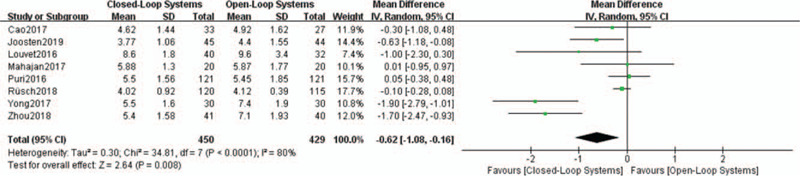
Forest plot of meta-analysis of the effects of closed-cloop systems versus open-loop systems on the dosage of propofol.
Figure 4.
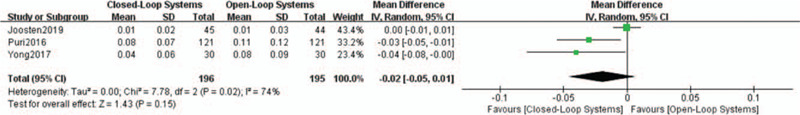
Forest plot of meta-analysis of the effects of closed-cloop systems versus open-loop systems on the incidence of hypertension or hypotension.
Figure 5.
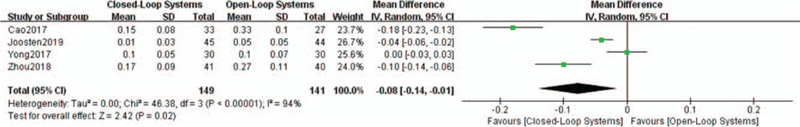
Forest plot of meta-analysis of the effects of closed-cloop systems versus open-loop systems on the incidence of POCD.
3.4. Subgroup analysis
Subgroup analyses were performed based on the surgery operation time (Fig. 6). For patients undergoing short time surgery less than 2 hours, MD for the dosage of propofol from 2 studies was −0.31 (95%, CI: −1.05–−0.44, P = .42), with no heterogeneity (I2 = 44%). For 2 to 4 hour surgical patients, MD was −0.99 (95%, CI: −1.89–−0.09, P = .03), with no heterogeneity (I2 = 88%). While, for patients undergoing liver transplantation and open cardiac surgery, MD was −0.18 (95%, CI: −0.78–0.43, P = .57), with no heterogeneity (I2 = 0%). The subgroup analysis showed that the difference of propofol dosage in short and medium time surgery such as non-cardiac surgery between the closed-loop system group and the open-loop system group was statistically significant.
Figure 6.
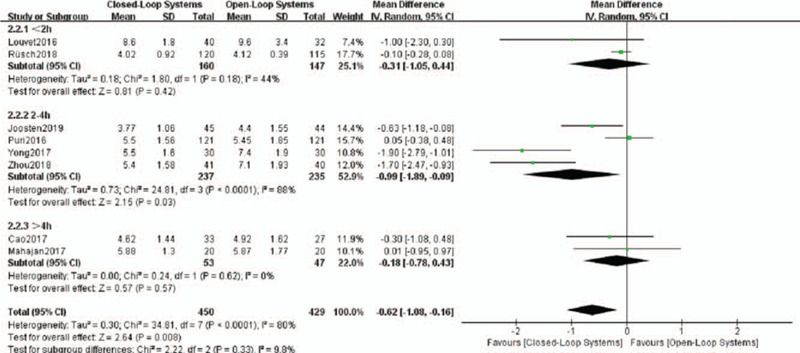
Forest plot of meta-analysis of the effects of closed-cloop systems versus open-loop systems on the subgroup analyses based on the surgery operation time.
3.5. Publication bias and sensitivity analysis
We assessed publication bias; no significant publication bias was found for propofol dosage (P = .01, Fig. 7). Sensitivity analysis and publication bias through removing one study per article, we found that the merged results were not stable (Table 2).
Figure 7.
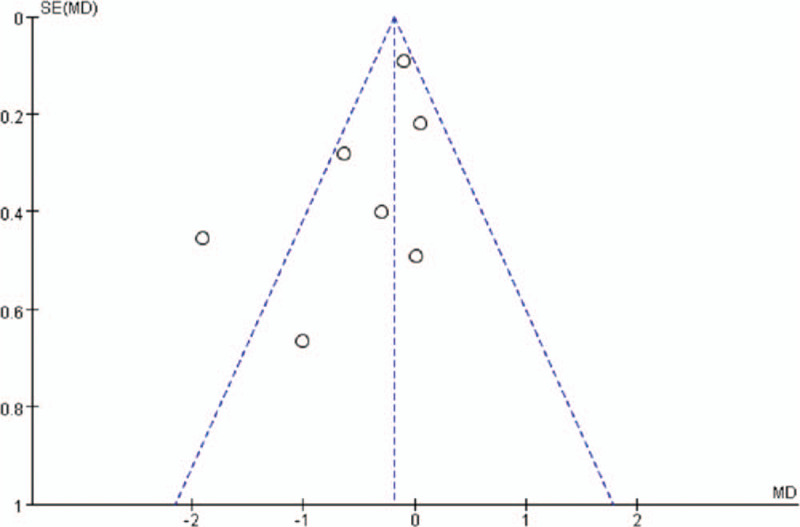
Funnel plot for assessing publication bias.
Table 2.
Sensitivity analysis and publication bias.
| P | I 2 | MD | 95%, CI | |
| Original | .008 | 80% | −0.62 | [−1.08, −0.16] |
| Removed 1 | .01 | 83% | −0.67 | [−1.19, −0.16] |
| Removed 2 | .02 | 82% | −0.63 | [−1.16, −0.10] |
| Removed 3 | .02 | 82% | −0.59 | [−1.07, −0.11] |
| Removed 4 | .007 | 83% | −0.70 | [−1.20, −0.20] |
| Removed 5 | .009 | 82% | −0.76 | [−1.33, −0.19] |
| Removed 6 | .01 | 78% | −0.75 | [−1.34, −0.15] |
| Removed 7 | .03 | 72% | −0.44 | [−0.84, −0.04] |
| Removed 8 | .03 | 71% | −0.44 | [−0.84, −0.03] |
4. Discussion
The bispectral index is a digital scale based on the electrical activity of the brain, which decreases with the increase of the depth of anesthesia.[20–22] The bottom of anesthesia is an essential objective index to evaluate the effect of anesthesia, important feedback information in the closed-loop system, and a key to the establishment of closed-loop systems.BIS values are usually maintained between 40 and 60 during anesthesia maintenance.[23,24] There is evidence that monitoring and maintaining BIS values of 40 to 60 in TIVA can reduce the incidence of intraoperative awareness by more than 80%.[25–27] Hemodynamic stability is also an essential goal of anesthesia patient management. Clinical studies have found that intraoperative anesthesia depth monitoring can maintain hemodynamic stability and reduce the incidence of perioperative hypertension or hypotension.[28,29] This meta-analysis proved that closed-loop systems could control the depth of anesthesia better than open-loop systems, reduce the dosage of drugs, and reduce the incidence of perioperative adverse reactions. This conclusion is consistent with previous clinical studies. This may be because maintaining a reasonable depth of anesthesia can reduce the impact of intraoperative consciousness, reduce the violent fluctuation of circulation, increase the dosage of anesthetic drugs, accelerate the patient's recovery time, improve the quality of anesthesia, and reduce the occurrence of anesthesia complications. Abnormal blood pressure includes hypertension, hypotension and other human factors. Because some pieces of literature only listed the number of patients with abnormal blood pressure, this meta-analyzed hypertension and hypotension together.
In this study, meta-analysis proved that the closed-loop group could reduce the dosage of propofol and reduce the incidence of intraoperative hypertension, hypotension, and postoperative cognitive dysfunction. This is because under the guidance of BIS propofol closed-loop systems by the computer automatically extract the BIS value analysis and calculation, with high sensitivity, can adjust in time for the small fluctuations in the BIS value target concentration and infusion rate, reduce the lag of “BIS changing clinically→ target concentration regulation →clinical effects” in open-loop systems.[30] However, some studies have found that BIS value is specified in the judgment of consciousness, but the sensitivity is not enough.[31] There is a lag in the monitoring of knowledge, which cannot clearly distinguish the existence of consciousness from the disappearance of consciousness. At present, the anesthesia depth detector needs further development and improvement. This real-time intelligent intravenous closed-loop controlled drug delivery system can not only integrate the indicators of anesthesia depth monitoring and automatically adjust the drug delivery rate, but also adjust and intervene with vital signs, such as blood pressure and heart rate, in the future, to maintain the stability of satisfactory anesthesia depth and circulation function and achieve robot anesthesia.[32]
This study has some shortcomings. First of all, BIS values can be influenced by several factors, such as intraoperative opioid and muscle relaxant levels. Due to the limitation of conditions, it is impossible to control the use of the same analgesic and muscle relaxant during the operation, so there may be some errors in this study. Also, the sample size collected in this study was small, so some large sample size randomized controlled trials need to be further carried out to explore the clinical efficacy of BIS in monitoring closed-loop systems of propofol. Finally, this study did not classify the population according to age or surgical method. Future studies should refine the population classification and add subgroup analysis, to make the results more accurate and targeted.
In this study, the dosage of propofol in the closed-loop group was less than that in the open-loop group. This could not only control the anesthetic depth but also avoid the waste of anesthetic drugs and reduce the adverse reactions caused by overdose and accumulation of anesthetic drugs. However, the relevant factors cannot be extracted and analyzed in this study. A large number of reasonably designed and rigorous studies are needed to verify the results of this study further. Randomized controlled trials are required to reflect the features of closed-loop systems in the future.[33]
5. Conclusion
Our results showed that closed-loop systems can control the depth of anesthesia better than open-loop systems during the maintenance period of intravenous anesthesia, and can reduce the dosage of drugs and the incidence of intraoperative and postoperative adverse reactions. However, more studies with large sample sizes were still needed to support our results.
Author contributions
Danyang Wang and Zichen Song contributed to the study concept and design, analysis and interpretation of data, statistical analysis, and drafting of the manuscript. Chunlu Zhang contributed to the acquisition of the data. Peng Chen contributed to the study concept and design and study supervision. All authors have read and approved the manuscript, and ensure that this is the case.
Data curation: Zichen Song, Chunlu Zhang.
Funding acquisition: Peng Chen.
Writing – original draft: Danyang Wang.
Glossary
Abbreviations: BIS = bispectral index, CI = confidence interval, EEG = electroencephalogram, MD = mean difference, POCD = postoperative cognitive dysfunction, RCT = randomized controlled trial, SD = standard deviation, TCI = target-controlled infusion, TIVA = total intravenous anesthesia.
References
- [1].Liu YH, Qiu DJ, Jia L, et al. Depth of anesthesia measured by bispectral index and postoperative mortality: a meta-analysis of observational studies. Clin Anesth 2019;56:119–25. [DOI] [PubMed] [Google Scholar]
- [2].Zorrilla-Vaca A, Healy RJ, Wu CL, et al. Relation between bispectral index measurements of anesthetic depth and postoperative mortality: a meta-analysis of observational studies. Can J Anaesth 2017;64:597–607. [DOI] [PubMed] [Google Scholar]
- [3].Short TG, Campbell D, Frampton C, et al. Anaesthetic depth and complications after major surgery: an international, randomised controlled trial. Lancet 2019;20:315–23. [DOI] [PubMed] [Google Scholar]
- [4].Reshef ER, Schiff ND, Brown EN. A neurologic examination for anesthesiologists assessing arousal level during induction, maintenance, and emergence. Anesthesiology 2019;130:462–71. [DOI] [PubMed] [Google Scholar]
- [5].Nimmo AF, Absalom AR, Bagshaw O, et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA): Joint Guidelines fromthe Association of Anaesthetists and the Society for Intravenous Anaesthesia. Anaesthesia 2018;20:128–34. [DOI] [PubMed] [Google Scholar]
- [6].Hyung C, Geol R, Chun EJ, et al. Prediction of Bispectral Index during Target-controlled Infusion of Propofol and Remifentanil. Anesthesiology 2018;128:492–501. [DOI] [PubMed] [Google Scholar]
- [7].Schuller PJ, Newell S, Strickland PA, et al. Response of bispectral index to neuromuscular block in awake volunteers. Br J Anaesth 2015;115:95–103. [DOI] [PubMed] [Google Scholar]
- [8].Pasin L, Nardelli P, Pintaudi M, et al. Closed-loop delivery systems versus manually controlled administration of total IV anesthesia: a meta-analysis of randomized clinical trials. Anesth Analg 2017;124:456–64. [DOI] [PubMed] [Google Scholar]
- [9].Brogi E, Shantale C, Kazan R, et al. Clinical performance and safety of closed-loop systems: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg 2017;124:446–55. [DOI] [PubMed] [Google Scholar]
- [10].Park SW, Lee H, Ahn H, et al. Bispectral index versus standard monitoring in sedation for endoscopic procedures: a systematic review and meta-analysis. Dig Dis Sci 2016;61:814–24. [DOI] [PubMed] [Google Scholar]
- [11].Cao YH, Chi P, Zhao YX, et al. Effect of bispectral index-guided anesthesia on consumption of anesthetics and early postoperative cognitive dysfunction after liver transplantation: an observational study. Medicine 2017;96:66–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Joosten A, Rinehart J, Bardaji A, et al. Anesthetic management using multiple closed-loop systems and delayed neurocognitive recovery: a randomized controlled trial. Anesthesiology 2019;7:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Louvet N, Rigouzzo A, Sabourdin N, et al. Bispectral index under propofol anesthesia in children: a comparative randomized study between TIVA and TCI. Paediatr Anaesth 2016;26:899–908. [DOI] [PubMed] [Google Scholar]
- [14].Mahajan V, Samra T, Puri GD, et al. Anaesthetic depth control using closed loop anaesthesia delivery system vs target controlled infusion in patients with moderate to severe left ventricular systolic dysfunction. J Clin Anesth 2017;42:106–13. [DOI] [PubMed] [Google Scholar]
- [15].Puri GD, Mathew PJ, Biswas I, et al. A multicenter evaluation of a closed-loop anesthesia delivery system: a randomized controlled trial. Anesth Analg 2016;122:106–14. [DOI] [PubMed] [Google Scholar]
- [16].Rusch D, Arndt C, Eberhar L, et al. Bispectral index to guide induction of anesthesia: a randomized controlled study. BMC Anesthesiol 2018;18:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yong FF, Jia HQ, Du SJ. Comparison of the cost and effect of closed loop and open loop controlled infusion of propofol under the guidance of BIS in elderly patients undergoing abdominal surgery. Chin J anesthesiology 2017;7:852–5. [Google Scholar]
- [18].Zhou Y, Li Y, Wang K. Bispectral index monitoring during anesthesia promotes early postoperative recovery of cognitive function and reduces acute delirium in elderly patients with colon carcinoma: a prospective controlled study using the attention network test. Med Sci Monit 2018;24:7785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Crowther M, Vader K, Roodt F, et al. Therelationship between pre-operative hypertension and intra-operativehaemodynamic changes known to be associated with postoperative morbidity. Anaesthesia 2018;73:812–8. [DOI] [PubMed] [Google Scholar]
- [20].Hajat Z, Ahmad N, Andrzejowski J. The role and limitations of EEG-based depth of anaesthesia monitoring in theatres and intensive care. Anaesthesia 2017;72:38–47. [DOI] [PubMed] [Google Scholar]
- [21].Dutta A, Sethi N, Sood J, et al. The effect of dexmedetomidine on propofol requirements during anesthesia administered bybispectral index-guided closed-loop anesthesia delivery system: a randomizedcontrolled study. Anesth Analg 2019;129:77–83. [DOI] [PubMed] [Google Scholar]
- [22].Mu J, Jiang T, Xu XB, et al. Comparison of target-controlled infusion and manual infusion for propofol anaesthesia in children. Bri J Anaesth 2018;120:41–9. [DOI] [PubMed] [Google Scholar]
- [23].Sabourdin N, Peretout JB, Khalil E, et al. Influence of depth of hypnosis on pupillary reactivity to a standardized tetanic stimulus in patients under propofol-remifentanil target-controlled infusion: a crossover randomized pilot study. Anesth Analg 2017;9:88–94. [DOI] [PubMed] [Google Scholar]
- [24].Petersen CL, Gorges M, Massey RB, et al. A procedural electroencephalogram simulator for evaluation of anesthesia monitors. Anesth Analg 2016;123:1136–40. [DOI] [PubMed] [Google Scholar]
- [25].Yuen MC, Gail PS, Robert JS, et al. Monitoring depth of hypnosis: mid-latency auditory evoked potentials derived aepEX in children receiving desflurane-remifentanil anesthesia. Anesth Analg 2018;11:707–14. [DOI] [PubMed] [Google Scholar]
- [26].Wang ZH, Chen H, Yang YL, et al. Bispectral index can reliably detect deep sedation in mechanically ventilated patients: a prospective multicenter validation study. Anesth Analg 2017;125:176–83. [DOI] [PubMed] [Google Scholar]
- [27].Evered LA, Silbert BS. Postoperative cognitivedysfunction and noncardiac surgery. Anesth Analg 2018;127:890–5. [DOI] [PubMed] [Google Scholar]
- [28].Lewis SR, Pritchard MW, Fawcett LJ, et al. Bispectral index for improving intraoperative awareness and early postoperative recovery in adults. Cochrane Database Syst Rev 2019;9:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zhang D, Nie A. Assessment of different anesthesia depth under total intravenous anesthesia on postoperative cognitive function in laparoscopic patients. J Res Med Sci 2016;27:26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cotoia A, Mirabella L, Beck R, et al. Effects of closed-loop intravenous anesthesia guided by bispectral index in adult patients on emergence delirium: a randomized controlled study. Minerva Anestesiol 2018;84:437–46. [DOI] [PubMed] [Google Scholar]
- [31].Sudhakaran R, Makkar JK, Jain D, et al. Comparison of bispectral index and end-tidal anaesthetic concentration monitoring on recovery profile of desflurane in patients undergoing lumbar spine surgery. Indian J Anaesth 2018;62:516–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Mccormick PJ, Levin MA, Lin HM, et al. Effectiveness of an electronic alert for hypotension and low bispectral index on 90-day postoperative mortality: a prospective, randomized trial. Anesthesiology 2016;125:1113–20. [DOI] [PubMed] [Google Scholar]
- [33].Maheshwar I, Mccormick PJ, Sessler DI, et al. Prolonged concurrent hypotension and low bispectral index (‘double low’) are associated with mortality, serious complications, and prolonged hospitalization after cardiac surgery. Br J Anaesth 2017;119:40–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wan X, Wang W, Liu J. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


