Abstract
This study aimed to compare adherence to dietary guidelines between elderly and non-elderly individuals with type 2 diabetes mellitus (T2DM) in Korea. Data of 4,577 participants with T2DM were collected from the 1998-2015 Korea National Health and Nutrition Examination Surveys. The participants were classified into two groups based on age: non-elderly T2DM group comprising participants aged 30–64 years and elderly T2DM group comprising participants aged ≥ 65 years. Adherence to dietary guidelines was assessed using the Korean Diabetes Association-Korean Ministry of Health and Welfare (KDA-KMHW) index, comprising six components of dietary guidelines for T2DM patients. Multivariable generalized linear regression analysis was performed to analyze the KDA-KMHW index scores. The adherence levels to the individual components of the KDA-KMHW index were mostly lower in non-elderly group (p < 0.001) than elderly group, except for moderate carbohydrate consumption. The total KDA-KMHW index score was significantly lower in non-elderly T2DM group than in the elderly T2DM group (p < 0.001). The study results suggest the need for developing patient-specific education programs that focus on adherence to dietary guidelines, particularly for non-elderly patients, to adequately intervene with the difficulties experienced in T2DM dietary management.
Keywords: Guideline adherence, Dietary guidelines, Diabetes mellitus, Elderly
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease recognized as a worldwide public health issue [1]. The prevalence of diabetes in South Korean adults (≥ 30 years) has been steadily increasing from 7.6% in women and 10.5% in men in 2005 to 9.5% in women and 14.0% in men in 2019 [2]. However, less than a third of patients with T2DM have maintained self-management of their diet and lifestyle to prevent diabetes complications [2].
Appropriate self-management of T2DM patients can considerably reduce the risks of diabetes complications including cerebrovascular diseases and diabetic nephropathy [3,4]. By contrast, a lack of self-management for T2DM can not only induce complications, but also increase medical costs, prolong hospitalization, and increase the risk of premature mortality [5,6]. Dietary management is particularly important in a T2DM patient's self-management [7,8]. Previous studies that assessed the effects of dietary interventions such as the Dietary Approaches to Stop Hypertension diet or the Mediterranean diet have demonstrated beneficial effects on the management of serum HbA1c, cholesterol, and triglyceride levels [9]. Moreover, appropriate energy intake and reduced carbohydrate intake [10], moderate alcohol consumption [11], adequate consumption of seaweed and dietary fibers [12,13], and limiting sodium consumption [14] have been reported to have a direct impact on improving blood glucose level. Therefore, dietary management for patients with T2DM is essential for the prevention of potential complications.
Recognition of the importance of self-management can vary between different age groups [15,16,17]. In general, older patients have higher risks of diabetic complications and hence the importance of management for these patients has been highly emphasized [18]. Meanwhile, younger patients with T2DM have a relatively longer remaining life expectancy, and therefore exhibit a prolonged risk period for potential complications since they have a longer duration of T2DM [18,19]. Thus, the management of T2DM is essential not only for older patients but also for younger patients. Many studies have evaluated drug compliance in patients with T2DM across different age groups [15,16,17], but limited studies have evaluated adherence levels to dietary guidelines by age.
Accordingly, the purpose of this study was to compare the adherence level to dietary guidelines between non-elderly (30–64 years) and elderly (≥ 65 years) participants with T2DM in Korea to determine the gaps and necessary interventions for improving the overall compliance to dietary guidelines for T2DM. Adherence level to dietary guideline for T2DM was estimated using the Korean Diabetes Association- Korean Ministry of Health and Welfare (KDA-KMHW) index [20], consisting of 6 components of dietary guidelines (meal patterns and intake levels of total energy, carbohydrates, vegetable/seaweed, sodium, and alcohol).
MATERIALS AND METHODS
Participants
Korea National Health and Nutrition Examination Survey (KNHANES) is a large-scale cross-sectional survey, which carried out to assess the health and nutritional status and health-related awareness or behavior of the civilian population of Korea [21]. The initial KNHANES were conducted every 3–4 years (1998, 2001, and 2005), and KNHANES IV (2007–2009) began using an annual survey with a rolling sample system [22]. This study used data from the 1st (1998) to the 6th (2013–2015) surveys. This study only included participants who aged 30 or older, were fully aware of their diabetes, and provided positive responses to the questions regarding clinician diagnoses, use of oral hypoglycemic agents, or insulin injections.
The following responses were excluded from the analysis: missing values on sampling weights or those without T2DM (n = 107,763); responses from the participants who were pregnant or breastfeeding at the time of the survey (n = 590); and responses from the participants who had a daily energy intake below 500 kcal or exceeding 5,000 kcal (n = 110). Finally, 4,577 participants were included from the 1st–6th KNHANES (1st n = 248; 2nd n = 247; 3rd n = 295; 4th n = 1,169; 5th n = 1,346; 6th n = 1,272).
Measurements
Age, sex, education level, smoking, alcohol consumption, and stress status were assessed through self-administered questionnaire. Information regarding household income and diabetes care (oral hypoglycemic agents or insulin injections) was collected at the interview. The education level was classified as below high school graduate or high school graduate and above, and smoking habits were categorized as non-smoker, former smoker, or current smoker. The household income levels were evaluated in terms of sex and age in accordance with the monthly household equivalence income, and categorized into quartiles: low, mid-low, mid-high, and high. Each participant's overall alcohol consumption was calculated by multiplying the frequency by the amount of alcohol consumed. Alcohol consumption was classified as non-drinkers, moderate drinkers (1–2 drinks a day), and heavy drinkers (more than 2 drinks a day). For stress status, the participants were asked regarding the level of stress they experience in their daily lives, and possible response options included the following: rarely, sometimes, most of the time, and always. Lastly, the duration of T2DM was calculated by subtracting the year of diagnosis from the age. Disease duration was categorized as follows: < 1, 1–4, 5–9, and ≥ 10 years. Comorbidity was defined as a condition in which participants with T2DM had chronic diseases other than diabetes (hypertension, dyslipidemia, stroke, myocardial infarction/angina, renal failure, cancer). We categorized into 1, 2, and 3 or more according to the number of comorbidity.
Height and weight were assessed through health examination. Body mass index (BMI) was calculated by dividing the weight (kg) by the square of height (m2). Using the standards of the Asian-Pacific region suggested by the World Health Organization (WHO), which considers the physical characteristics of the Asian population, the participants with a BMI < 23 kg/m2 were considered underweight/normal, while participants with a BMI ≥ 23 kg/m2 were considered overweight/obese [23].
Dietary intake levels were assessed using a single 24-hour recall data. Trained interviewers assessed the type, amount, and composition of food that the participants consumed one day before the interview. To improve the accuracy of the assessments, auxiliary tools including food models or shapes, measuring cups, spoons, and tape measures were used [24].
Dietary guideline adherence
Adherence to dietary guidelines was evaluated using the KDA-KMHW index. A detailed explanation regarding the KDA-KMHW index is provided in previous study [20]. Briefly, the index is comprised of six components based on the “Treatment guidelines for diabetes” developed by the Korean Diabetes Association and “Dietary guidelines for disease management” published by the Korean Ministry of Health and Welfare [25,26,27,28]. These components are 1) moderate calorie consumption (± 10% of the recommended energy intake); 2) moderate carbohydrate consumption (50%–60% of the total energy intake); 3) maintaining regular meal patterns (all 3 meals including breakfast, lunch, and dinner); 4) sufficient vegetable/seaweed consumption (one serving of vegetables/seaweeds excluding kimchi and pickled vegetables; men: ≥ 8 servings at all ages per day, women: ≥ 8 servings per day for participants aged between 30 and 64 years and ≥ 6 servings per day for participants aged ≥ 65 years); 5) limited sodium intake (< 2,000 mg of sodium per day); and 6) moderate alcohol consumption (≤ 2 glasses per day for men and ≤ 1 glass per day for women). Participants who were following the above guidelines were given one point per category. The total score of the KDA-KMHW index ranges from 0 to 6, with a higher score indicating higher adherence.
Statistical analyses
All statistical analyses were performed considering the complex survey design. To comprehensively analyze the data collected from the 1st–6th KNHANES, different assessment categories for different years were also considered for appropriate weighting. For the analysis, the participants were divided into two groups according to age: elderly T2DM group (≥ 65 years) and non-elderly T2DM group (< 65 years). The distribution of the general characteristics of the participants in the non-elderly T2DM group and the elderly T2DM group was evaluated using frequency (%). Differences between the two groups were analyzed using a χ2 test for categorical variables and a t-test or regression analysis for continuous variables. The KDA-KMHW index scores in non-elderly T2DM group and the elderly T2DM group were analyzed using multivariable regression analysis (SAS PROC SURVEYREG), and the mean value was calculated after adjusting for sex, education level, smoking habits, household income, alcohol consumption, diabetes care (oral hypoglycemic agents or insulin injection), diabetes duration, number of comorbidities, and BMI. All statistical analyses in this study were performed using SAS (Statistical Analysis System version 9.4; SAS Institute, Cary, NC, USA). p value was assessed with a 2-tailed test and significance of α = 0.05.
RESULTS
Demographic and lifestyle characteristics of participants according to age group
Compared to the elderly participants with T2DM, non-elderly participants with T2DM were more likely to be men (p < 0.001) and have a higher education level (p < 0.001) and skip breakfast (p < 0.001). In addition, the proportion of participants who smoked (p < 0.001) and were overweight/obese (p < 0.001) was significantly higher in non-elderly T2DM group. Meanwhile, the proportion of participants who never consumed alcohol (p < 0.001), had a higher household income (p < 0.001), showed strict management of diabetes care (p < 0.001), and more than 10 years duration of diabetes (p < 0.001) was significantly higher in the elderly T2DM group (Table 1).
Table 1. Demographic and lifestyle characteristics of the participants with diabetes mellitus according to age group, KNHANES 1998–2015.
| Characteristics | < 65 years | ≥ 65 years | p value* | |
|---|---|---|---|---|
| No. participants | 2,181 | 2,396 | ||
| Median and range of age (yr) | 54 (30–64) | 72 (65–93) | ||
| Sex | < 0.001 | |||
| Male | 1,153 (52.9) | 1,000 (41.7) | ||
| Female | 1,028 (47.1) | 1,396 (58.3) | ||
| Education level | < 0.001 | |||
| Middle school or lower | 1,199 (54.7) | 1,890 (78.7) | ||
| High school or higher | 982 (45.3) | 506 (21.3) | ||
| Smoking status | < 0.001 | |||
| Non-smoker | 1,118 (51.5) | 1,384 (58.4) | ||
| Former smoker | 497 (22.9) | 665 (28.1) | ||
| Current smoker | 556 (25.6) | 320 (13.5) | ||
| Alcohol consumption | < 0.001 | |||
| Non-drinker | 849 (39.2) | 1,418 (59.9) | ||
| Moderate alcohol drinker | 992 (45.8) | 796 (33.6) | ||
| Heavy drinker | 327 (15.1) | 155 (6.5) | ||
| Household income | < 0.001 | |||
| Low | 660 (30.6) | 570 (24.2) | ||
| Mid-low | 575 (26.7) | 597 (25.4) | ||
| Mid-high | 458 (21.3) | 594 (25.2) | ||
| High | 462 (21.4) | 592 (25.2) | ||
| Stress status | < 0.001 | |||
| Rarely | 397 (18.3) | 811 (34.2) | ||
| Sometimes | 1,115 (51.4) | 1,011 (42.7) | ||
| Most of the time | 512 (23.6) | 426 (18.0) | ||
| Always | 146 (6.7) | 121 (5.1) | ||
| Oral hypoglycemic agents or insulin use | 1,762 (80.8) | 2,102 (87.7) | < 0.001 | |
| Diabetes duration | < 0.001 | |||
| < 1 year | 189 (8.8) | 133 (5.6) | ||
| 1–4 years | 829 (38.6) | 653 (27.5) | ||
| 5–9 years | 503 (23.4) | 553 (23.3) | ||
| ≥ 10 years | 629 (29.3) | 1032 (43.5) | ||
| No. of comorbidities | < 0.001 | |||
| 0 | 719 (33.0) | 480 (20.0) | ||
| 1 | 989 (45.4) | 1,243 (51.9) | ||
| 2 | 399 (18.3) | 561 (23.4) | ||
| ≥ 3 | 74 (3.4) | 112 (4.7) | ||
| Overweight or obesity† | 1,575 (72.5) | 1,599 (67.1) | < 0.001 | |
Values are presented as number (%), except for age.
KNHANES, Korea National Health and Nutrition Examination Survey.
*p values were derived from a χ2 test; †Body mass index (kg/m2) ≥ 23
Adherence levels to dietary guidelines according to age group
Table 2 presents a comparison of the adjusted score levels of the KDA-KMHW index and its 6 components between the non-elderly and elderly groups of participants with T2DM, controlling for sex, education, smoking status, alcohol status, household income, diabetes care, diabetes duration, number of comorbidities, and BMI. The adherence level to moderate carbohydrate consumption was significantly higher in the non-elderly T2DM group than in the elderly T2DM group (p = 0.020). However, the adherence level to maintaining regular meal patterns (p = 0.003), limited sodium intake (p < 0.001), and moderate alcohol consumption (p < 0.001) was higher in the elderly T2DM group. The total KDA-KMHW index score was significantly higher in the elderly T2DM group than in the non-elderly T2DM group (p < 0.001).
Table 2. Average adherence score for the dietary guidelines for participants with diabetes mellitus according to age group, KNHANES 1998–2015.
| Component of the KDA-KMHW index§ | < 65 years | ≥ 65 years | p value‡ |
|---|---|---|---|
| Moderate calorie consumption* | 0.21 ± 0.02 | 0.21 ± 0.02 | 0.900 |
| Moderate carbohydrate consumption* | 0.11 ± 0.01 | 0.08 ± 0.01 | 0.020 |
| Maintaining regular meal patterns* | 0.74 ± 0.02 | 0.79 ± 0.02 | 0.003 |
| Sufficient vegetable/seaweed consumption* | 0.06 ± 0.01 | 0.07 ± 0.01 | 0.400 |
| Limited sodium intake* | 0.18 ± 0.02 | 0.30 ± 0.02 | < 0.001 |
| Moderate alcohol consumption† | 0.83 ± 0.01 | 0.90 ± 0.01 | < 0.001 |
| Total score of the KDA-KMHW index†,∥ | 2.14 ± 0.03 | 2.36 ± 0.03 | < 0.001 |
Values are presented as mean ± standard deviation.
KNHANES, Korea National Health and Nutrition Examination Survey; KDA-KMHW, Korean Diabetes Association- Korean Ministry of Health and Welfare.
*Values are adjusted for sex, education, smoking status, household income, diabetes care, diabetes duration, number of comorbidities, body mass index, and alcohol consumption; †Values are adjusted for sex, education, smoking status, household income, diabetes care, diabetes duration, number of comorbidities and body mass index; ‡p values were derived from general linear regression analyses; §The score of each component of KDA-KMHW index ranges from 0 (worst) to 1 (best); llTotal score of KDA-KMHW index ranges from 0 (worst) to 6 (best).
Trends in the KDA-KMHW index score by age group and survey year
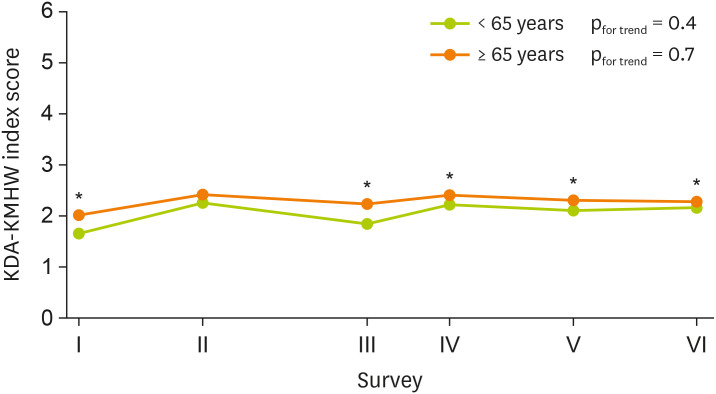
A comparison of KDA-KMHW index scores between the two groups across the 1st to 6th surveys (1998-2015) (Figure 1) showed no change in the adherence trend for both groups (non-elderly T2DM group, pfor trend = 0.4; elderly T2DM group, pfor trend = 0.7). However, the elderly T2DM group showed significantly higher adherence levels than the non-elderly T2DM group for all survey sessions except the 2nd survey (2001).
Figure 1. Trends in adherence to dietary guidelines by age group as assessed using the KDA-KMHW index. Multivariable general linear model was used to test for differences in adherence to the KDA-KMHW index between non-elderly and elderly groups for all survey years. Values were adjusted for sex, education, smoking status, household income, diabetes care, diabetes duration, number of comorbidities, and body mass index.
KDA-KMHW, Korean Diabetes Association- Korean Ministry of Health and Welfare.
*p < 0.05.
DISCUSSION
Appropriate self-management in T2DM patients can reduce the risks of complications. However, the adherence to dietary guidelines for T2DM self-management varies according to age. In this study, the non-elderly participants with T2DM showed lower adherence levels than the elderly group, particularly for maintaining a regular meal pattern, limited sodium intake, and moderate alcohol consumption. The total KDA-KMHW index scores for all survey years between 1998 and 2015 were significantly lower in the non-elderly participants with T2DM than in the elderly participants with T2DM, except the 2nd survey II (2001).
Maintaining regular meal patterns has been suggested as an important factor in preventing the risk of hyperglycemia [29]. More specifically, skipping breakfast can damage insulin responses and reduce the level of glucagon-like peptide-1 that increases insulin secretion, consequently increasing the risk of post-meal hyperglycemia. Therefore, the importance of a regular meal pattern for individuals with T2DM has been emphasized continuously [30]. In this study, the non-elderly T2DM group exhibited a lower adherence level to maintaining regular meal patterns than the elderly T2DM group, and approximately 50% of participants who did not have regular meal patterns responded that they were skipping breakfast (data not shown). The key reason for skipping meals was a lack of time [31], demonstrating that the busy schedules of non-elderly individuals may have affected their ability to maintain regular meal patterns.
Although elderly participants may consume more salt due to an increased threshold for salty tastes [32], the adherence level for “limited sodium intake” was higher in the elderly group. Limited sodium intake can reduce blood pressure and help prevent hypertension, which is a key risk factor of cardiovascular disease [8]. Nevertheless, the average sodium intake of Koreans was 3,668.9mg/day, above daily recommended sodium intake of 2,000 mg [33]. More specifically, young adults have a high level of sodium intake, at 310% and 245% of the recommended daily requirements for men and women, respectively [34]. A higher frequency of dining out in the non-elderly population compared to the elderly population may have affected the adherence level of non-elderly participants with T2DM, as the sodium intake levels from eating-out was over 5,000 mg per day among Korean adults [35,36].
In this study, the non-elderly T2DM group showed a low adherence level to “moderate alcohol consumption” compared to the elderly as well. Moderate to low alcohol consumption can significantly reduce the occurrence of cardiovascular diseases in participants with T2DM [11], while excessive amounts can induce hypertension [37]. A study on alcohol consumption in the Korean population showed that the proportion of individuals with excessive alcohol consumption is substantially higher in the younger population than in the elderly [38], which is in line with the findings of the current study. Alcohol consumption can reduce the level of growth hormones overnight and induce hypoglycemia the next day [39]. Therefore, more attention and interventions are required for non-elderly Korean patients with T2DM who exhibit irregular meal patterns and low adherence to appropriate alcohol consumption.
Adherence levels to most dietary guidelines including regular meal patterns, moderate alcohol consumption, and limited sodium intake were higher in the elderly participants with T2DM than in the non-elderly participants. However, adherence to “moderate carbohydrate consumption” was remarkably lower in the elderly group. Traditionally, the Korean population has been dependent on white rice as a main nutritional source [40], and elderly individuals, especially, tend to maintain a higher dependency on dietary habits consuming white rice [41,42]. Refined carbohydrate consumption rapidly increases the blood glucose and has negative effects on the management of fasting blood glucose level, HbA1c, and triglycerides [43,44]. This suggests that the need for different educational strategies for carbohydrate consumption among the different age groups.
In this study, the overall adherence level to dietary guidelines was lower in the non-elderly participants with T2DM than in the elderly participants. Similarly, previous studies reported that non-elderly individuals with T2DM showed lower treatment compliance (antidiabetic drug intake and blood glucose management) than the elderly [15,16]. There are a few possible explanations for the higher adherence level observed in the elderly individuals with T2DM. First, elderly individuals have higher and more frequent exposure to medical services [45], and the interaction between patient, physician, and clinical nutritionist may have had a positive effect on the elderly's adherence levels. Second, elderly individuals are reportedly more concerned about their health compared to non-elderly individuals because of their relatively shorter remaining life expectancy [46]. Third, elderly individuals with T2DM experience physical symptoms such as acute pain, neurological disorders, or shortness of breath, while younger individuals experience psychosocial symptoms such as fatigue and depression [47]. A lack of physical symptoms in younger individuals may cause them to be unaware of their medical condition [48], and thus non-elderly individuals with T2DM find it more difficult to comply with dietary guidelines. Therefore, it is necessary to develop age-specific nutrition education program that can achieve the education goal for non-elderly T2DM group who have experienced difficulties in T2DM dietary management.
There are several limitations in this study. One-day recall data were used to assess the adherence to dietary guidelines; thus, the study results may have been influenced by some degree of measurement errors. In addition, there may be potential misclassification regarding the identification of diabetes because we used self-reported information for diabetes medical history. Despite these limitations, this study is a national-level study that can represent the entire population of Korean individuals with diabetes, and therefore the findings can be generalized to adults with T2DM in Korea. Furthermore, with very limited previous studies that assessed the adherence of individuals with T2DM to dietary guidelines by age, this study can provide scientific evidence to guide disease management strategies in Korean individuals with diabetes.
CONCLUSION
Non-elderly participants with T2DM in Korea have relatively lower adherence to dietary guidelines compared to elderly participants. In addition, the adherence levels to dietary guidelines for each components were different by age groups, raising the need for development of detailed patient-specific nutrition education programs that manage vulnerable points. These findings suggest the need for the development of an active educational program to raise awareness on the importance of disease self-management, as well as the need for improvement of dietary habits in non-elderly individuals with T2DM. In addition, continuous systematic management should be provided to further prevent disease progression and associated complications.
Footnotes
Funding: This research was supported by the 2019 Yeungnam University research grant and by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (grant number: NRF-2017R1A1A3A04069759). The funding sponsor had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Conflict of Interest: The authors declare that they have no competing interests.
References
- 1.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Heath and Welfare; Korea Centers for Disease Control and Prevention. Korea health statistics 2019: Korea National Health and Nutrition Examination Survey (KNHANES) [Internet] 2020. [cited 2021 January 6]. Available from https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.
- 3.Kim HS, Oh JA. Adherence to diabetes control recommendations: impact of nurse telephone calls. J Adv Nurs. 2003;44:256–261. doi: 10.1046/j.1365-2648.2003.02800.x. [DOI] [PubMed] [Google Scholar]
- 4.Curtis SE, Boye KS, Lage MJ, Garcia-Perez LE. Medication adherence and improved outcomes among patients with type 2 diabetes. Am J Manag Care. 2017;23:e208–14. [PubMed] [Google Scholar]
- 5.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 6.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 7.Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, Neumiller JJ, Nwankwo R, Verdi CL, Urbanski P, Yancy WS., Jr Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2014;37(Suppl 1):S120–43. doi: 10.2337/dc14-S120. [DOI] [PubMed] [Google Scholar]
- 8.International Diabetes Federation. Managing type 2 diabetes in primary care [Internet] 2017. [cited 2018 March 22]. Available from https://www.idf.org/managing-type2-diabetes.
- 9.Azadbakht L, Fard NR, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, Esmaillzadeh A, Willett WC. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care. 2011;34:55–57. doi: 10.2337/dc10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Westman EC, Feinman RD, Mavropoulos JC, Vernon MC, Volek JS, Wortman JA, Yancy WS, Phinney SD. Low-carbohydrate nutrition and metabolism. Am J Clin Nutr. 2007;86:276–284. doi: 10.1093/ajcn/86.2.276. [DOI] [PubMed] [Google Scholar]
- 11.Howard AA, Arnsten JH, Gourevitch MN. Effect of alcohol consumption on diabetes mellitus: a systematic review. Ann Intern Med. 2004;140:211–219. doi: 10.7326/0003-4819-140-6-200403160-00011. [DOI] [PubMed] [Google Scholar]
- 12.Lee HJ, Kim HC, Vitek L, Nam CM. Algae consumption and risk of type 2 diabetes: Korean National Health and Nutrition Examination Survey in 2005. J Nutr Sci Vitaminol (Tokyo) 2010;56:13–18. doi: 10.3177/jnsv.56.13. [DOI] [PubMed] [Google Scholar]
- 13.Yang L, Shu L, Jiang J, Qiu H, Zhao G, Zhou Y, Jiang Q, Sun Q, Qin G, Wu H, Yang L, Ruan X, Xu WH. Long-term effect of dietary fibre intake on glycosylated haemoglobin A1c level and glycaemic control status among Chinese patients with type 2 diabetes mellitus. Public Health Nutr. 2014;17:1858–1864. doi: 10.1017/S1368980013002000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ekinci EI, Clarke S, Thomas MC, Moran JL, Cheong K, MacIsaac RJ, Jerums G. Dietary salt intake and mortality in patients with type 2 diabetes. Diabetes Care. 2011;34:703–709. doi: 10.2337/dc10-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Casagrande S, Cowie CC, Fradkin JE. Intensive glycemic control in younger and older U.S. adults with type 2 diabetes. J Diabetes Complications. 2017;31:1299–1304. doi: 10.1016/j.jdiacomp.2017.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Shea MP, Teeling M, Bennett K. An observational study examining the effect of comorbidity on the rates of persistence and adherence to newly initiated oral anti-hyperglycaemic agents. Pharmacoepidemiol Drug Saf. 2013;22:1336–1344. doi: 10.1002/pds.3535. [DOI] [PubMed] [Google Scholar]
- 17.Yang Y, Thumula V, Pace PF, Banahan BF, 3rd, Wilkin NE, Lobb WB. Predictors of medication nonadherence among patients with diabetes in Medicare Part D programs: a retrospective cohort study. Clin Ther. 2009;31:2178–2188. doi: 10.1016/j.clinthera.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, Heller S, Marre M, Patel A, Poulter N, Williams B, Chalmers J ADVANCE Collaborative Group. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57:2465–2474. doi: 10.1007/s00125-014-3369-7. [DOI] [PubMed] [Google Scholar]
- 19.Price HC, Clarke PM, Gray AM, Holman RR. Life expectancy in individuals with type 2 diabetes: implications for annuities. Med Decis Making. 2010;30:409–414. doi: 10.1177/0272989X09349960. [DOI] [PubMed] [Google Scholar]
- 20.Park K. Trends in adherence to dietary recommendations among Korean type 2 diabetes mellitus patients. Nutr Res Pract. 2015;9:658–666. doi: 10.4162/nrp.2015.9.6.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korea Centers for Disease Control and Prevention. Implementation state of National Health and Nutrition Survey [Internet] 2019. [cited 2020 February 20]. Available from https://knhanes.cdc.go.kr/knhanes/sub02/sub02_01.do.
- 23.World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment [Internet] 2000. [cited 2018 March 1]. Available from https://apps.who.int/iris/handle/10665/206936.
- 24.Korea Centers for Disease Control and Prevention. Guidelines for examination and inspection [Internet] 2018. [cited 2020 February 12]. Available from https://knhanes.cdc.go.kr/knhanes/sub04/sub04_02_02.do?classType=4.
- 25.Korean Diabetes Association. Treatment guideline for diabetes. 2nd ed. Seoul: Korean Diabetes Association; 1995. pp. 25–32. [Google Scholar]
- 26.Korean Diabetes Association. Treatment guideline for diabetes. 3rd ed. Seoul: Korean Diabetes Association; 2007. pp. 49–54. [Google Scholar]
- 27.Korean Diabetes Association. Treatment guideline for diabetes. 4th ed. Seoul: Korean Diabetes Association; 2011. pp. 54–57. [Google Scholar]
- 28.The Ministry of Health and Welfare. Dietary guidelines for disease management [Internet] 2010. [cited 2018 June 2]. Available from http://phi.mw.go.kr:7012/cms/epWeb/resources/jsp/healthinfo/news/healthnews_01/2811927_1748.jsp.
- 29.Kollannoor-Samuel G, Chhabra J, Fernandez ML, Vega-López S, Pérez SS, Damio G, Calle MC, D'Agostino D, Pérez-Escamilla R. Determinants of fasting plasma glucose and glycosylated hemoglobin among low income Latinos with poorly controlled type 2 diabetes. J Immigr Minor Health. 2011;13:809–817. doi: 10.1007/s10903-010-9428-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jakubowicz D, Wainstein J, Ahren B, Landau Z, Bar-Dayan Y, Froy O. Fasting until noon triggers increased postprandial hyperglycemia and impaired insulin response after lunch and dinner in individuals with type 2 diabetes: a randomized clinical trial. Diabetes Care. 2015;38:1820–1826. doi: 10.2337/dc15-0761. [DOI] [PubMed] [Google Scholar]
- 31.Ahn HJ, Han KA, Koo BK, Kim HJ, Kim HJ, Park KS, Min KW. Analysis of meal habits from the viewpoint of regularity in Korean type 2 diabetic patients. Korean Diabetes J. 2008;32:68–76. [Google Scholar]
- 32.Nordin S, Razani LJ, Markison S, Murphy C. Age-associated increases in intensity discrimination for taste. Exp Aging Res. 2003;29:371–381. doi: 10.1080/03610730303719. [DOI] [PubMed] [Google Scholar]
- 33.National Institute of Food and Drug Safety Evaluation. A study on the relation of nutrient intake and disease and intake of nutrients among Korean adults. Cheongju: Ministry of Food and Drug Safety; 2018. [Google Scholar]
- 34.Shim E, Ryu HJ, Hwang J, Kim SY, Chung EJ. Dietary sodium intake in young Korean adults and its relationship with eating frequency and taste preference. Nutr Res Pract. 2013;7:192–198. doi: 10.4162/nrp.2013.7.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ju SY. Changes in eating-out frequency according to sociodemographic characteristics and nutrient intakes among Korean adults. Iran J Public Health. 2020;49:46–55. [PMC free article] [PubMed] [Google Scholar]
- 36.Kim MG, Kim KY, Nam HM, Hong NS, Lee YM. The relationship between lifestyle and sodium intake in Korean middle-aged workers. J Korea Acad Ind Coop Soc. 2014;15:2923–2929. [Google Scholar]
- 37.Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012;14:792–798. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park H. Prevalence and related risk factors of problem drinking in Korean adult population. J Korea Acad Ind Coop Soc. 2018;19:389–397. [Google Scholar]
- 39.Turner BC, Jenkins E, Kerr D, Sherwin RS, Cavan DA. The effect of evening alcohol consumption on next-morning glucose control in type 1 diabetes. Diabetes Care. 2001;24:1888–1893. doi: 10.2337/diacare.24.11.1888. [DOI] [PubMed] [Google Scholar]
- 40.Korea Health Industry Development Institute. Frequent food intake 2018 [Internet] 2018. [cited 2021 January 6]. Available from https://www.khidi.or.kr/kps/dhraStat/result4?menuId=MENU01655&gubun=age1&year=2018.
- 41.Lee MJ, Popkin BM, Kim S. The unique aspects of the nutrition transition in South Korea: the retention of healthful elements in their traditional diet. Public Health Nutr. 2002;5:197–203. doi: 10.1079/PHN2001294. [DOI] [PubMed] [Google Scholar]
- 42.So EJ, Joung H. Socio-economic status is associated with the risk of inadequate energy intake among Korean elderly. J Nutr Health. 2015;48:371–379. [Google Scholar]
- 43.American Diabetes Association. Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, Mooradian AD, Wheeler ML. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(Suppl 1):S61–78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- 44.Kirk JK, Graves DE, Craven TE, Lipkin EW, Austin M, Margolis KL. Restricted-carbohydrate diets in patients with type 2 diabetes: a meta-analysis. J Am Diet Assoc. 2008;108:91–100. doi: 10.1016/j.jada.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 45.Korean Statistical Information Service. Medical service utilization rate [Internet] 2020. [cited 2021 January 10]. Available from https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117099_A001&vw_cd=&list_id=&seqNo=&lang_mode=ko&language=kor&obj_var_id=&itm_id=&conn_path=
- 46.Diefenbach GJ, Stanley MA, Beck JG. Worry content reported by older adults with and without generalized anxiety disorder. Aging Ment Health. 2001;5:269–274. doi: 10.1080/13607860120065069. [DOI] [PubMed] [Google Scholar]
- 47.Sudore RL, Karter AJ, Huang ES, Moffet HH, Laiteerapong N, Schenker Y, Adams A, Whitmer RA, Liu JY, Miao Y, John PM, Schillinger D. Symptom burden of adults with type 2 diabetes across the disease course: diabetes & aging study. J Gen Intern Med. 2012;27:1674–1681. doi: 10.1007/s11606-012-2132-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mosleh SM, Darawad M. Patients' adherence to healthy behavior in coronary heart disease: risk factor management among Jordanian patients. J Cardiovasc Nurs. 2015;30:471–478. doi: 10.1097/JCN.0000000000000189. [DOI] [PubMed] [Google Scholar]