Abstract
Background and Objectives
This study investigated the relative incidence of contrast induced nephropathy (CIN) and long-term outcomes between iso-osmolar contrast media (IOCM) and low-osmolar contrast media (LOCM) undergoing elective percutaneous coronary intervention (PCI).
Methods
A total of 9,431 patients receiving elective PCI were enrolled in the cohort. The patients were divided into IOCM group and LOCM group. Propensity score matching (PSM) was applied to minimize the selection bias between groups.
Results
The multivariate analysis showed that the use of IOCM compared with LOCM did not affect the CIN incidence (odds ratio [OR], 0.912; 95% confidence interval [CI], 0.576–1.446; p=0.696). After PSM, the incidence of CIN was 1.5% and 4.0% in IOCM group (n=979) and LOCM group (n=979), respectively, p=0.001. IOCM significantly reduced the incidence of CIN compared with LOCM (OR, 0.393; 95% CI, 0.214–0.722; p=0.003). After 2 years of follow-up, the all-cause mortality was higher in IOCM group than LOCM group (2.1% vs. 0.9%, p<0.001). Cox regression analysis showed IOCM was not independent risk factor of 2-years all-cause mortality (OR, 0.849; 95% CI, 0.510–1.412; p=0.528). After PSM, the difference of all-cause death between groups disappeared (1.7% vs. 1.9%, p=0.739). Cox regression analysis showed that the use of IOCM compared with LOCM did not affect the incidence of 2-year all-cause mortality (OR, 1.037; 95% CI, 0.534–2.014; p=0.915).
Conclusions
Compared with LOCM, IOCM significantly reduced the incidence of CIN after elective PCI, but had no significant effect on 2-year all-cause mortality.
Keywords: Contrast media, Percutaneous coronary intervention, Coronary artery disease
INTRODUCTION
Contrast-induced nephropathy (CIN) is one of the common complications of coronary interventional therapy, which accounts for the increase in morbidity, mortality, length of stay and hospitalization cost.1),2) The use of low-osmolar contrast media (LOCM) and iso-osmolar contrast media (IOCM) significantly reduces the incidence of CIN compared with high-osmolar contrast media. At first, many studies found that IOCM can reduce the incidence of CIN.3) However, in recent years, some of studies have reached different conclusions.4),5),6) Some studies did not observe any difference between IOCM and LOCM. This study compared the correlation of CIN and 2-year all-cause mortality between usage of IOCM agents and LOCM agents in patients who underwent elective percutaneous coronary intervention (PCI) using a large retrospective cohort.
METHODS
Ethical approval
As a retrospective study, data analysis was performed anonymously. This study was exempt from the ethical approval and informed consent from patients.
Patient population
For this retrospective observational study, we identified a consecutive group of 10,724 patients who had received PCI in Fuwai hospital, Beijing, China from January 1st 2013 to December 31th, 2013. The 9,431 patients with elective PCI were eventually enrolled and divided into IOCM group (n=1,665) and LOCM group (n=7,766) according to the contrast agent used.
Procedural and data collection
All patients underwent elective PCI at the clinician's discretion according to the condition of coronary artery disease (CAD). Stents were placed according to conventional methods. Perioperative and intraoperative antiplatelet and anticoagulant therapy were performed according to relevant guidelines. The IOCM that the agent used was iodixanol (Visipaque 320; General Electric Pharmaceutical, Carrigtohill, Ireland). Four LOCM agents included iohexol (Shuangbei 350; Beijing Shuangbei Pharmaceutical, Beijing, China), ioversl (Optiray 350; Liebel-Flarsheim Canada Inc., Quebec, Canada) iopamidol (Iopamiro 370; Patheon Italia S.P.A., Monza, Italy) and iopromide (Ultravist 370; Bayer Pharmaceutical, Shanghai, China). The choice of contrast media agent was determined by the interventional physician. The patients with renal insufficiency were hydrated from 12–24 hours before operation to 12–24 hours after operation, and the hydration rate was 0.5–1 mL/(kg·min). All patients received a continuous intravenous slow drip of at least 1,000 mL of 0.9% sodium chloride after contrast exposure except where there was contraindication for volume expansion such as congestive heart failure. After intervention therapy, both groups of patients with CAD were treated with dual antiplatelet therapy of aspirin (100 mg, once a day) and clopidogrel (75 mg, once a day) or ticagrelor (90 mg, twice a day) for at least 1 year. Data were obtained from interventional catheterization laboratory and information center of Fuwai hospital. General clinical data, laboratory findings and interventional treatment data were collected from inpatient medical records and interventional treatment records.
Definitions and follow-up
CIN was defined using the criteria in the clinical guidelines issued by the Kidney Disease Improving Global Outcomes (KDIGO) in 2012, serum creatinine (SCr) increased by >0.3 mg/dL (26.5 µmol/L) or >50% from baseline within 48 hours after exposure.7) Estimated glomerular filtration rate (eGFR) was calculated using the modified of diet in renal disease formula, eGFR (mL/min/1.73 m2) = 186 × Scr − 1.154 × age − 0.203 (female × 0.742).8) Three vessel lesion was defined as angiographically confirmed stenosis of ≥50% in all 3 main coronary arteries, including left anterior descending artery, left circumflex artery and right coronary artery, with or without left main coronary artery involved. Follow-up methods: The patients were visited after 1 month, 6 months, 1 year and 2 years after elective PCI. Information of in-hospital outcome was obtained through review of medical records, and the long-term clinical outcome was collected from survey completed by telephone follow-up, follow-up letter or visit.
Statistical analysis
SPSS version 24.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Independent t-tests were used to compare continuous variables fitting normal distribution while χ2 tests were applied to compare categorical variables between the 2 groups. Propensity score matching (PSM) using closest match with a 1:1 ratio was applied to control for baseline differences, and the caliper was set as 0.01. PSM was calculated based on 18 variables (age, gender, diabetes mellitus, hyperlipidemia, hypertension, smoking, old myocardial infarction, previous PCI, previous coronary artery bypass grafting, ST elevated myocardial infarction, stable coronary disease, left ventricular ejection fraction (LVEF), eGFR before PCI, SCr before PCI, Triple vessel, Syntax sore, contrast volume, intra-aotic balloon pump (IABP) support (Table 1). Multivariate regression analysis was used to analyze the correlation between contrast agents and CIN. Kaplan-Meier survival analysis was used to evaluate 2-year all-cause mortality after elective PCI with different contrast agents, and log-rank test was used to compare all-cause mortality between 2 groups. Univariate analysis was used to analyze the predictors of 2-year all-cause mortality. Variables with p<0.10 in univariate analysis and clinically significant variables were analyzed by multivariate Cox regression. The p<0.05 was considered statistically significant.
Table 1. Patient demographics and clinical characteristics before and after PSM.
| Characteristics | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| IOCM (n=1,665) | LOCM (n=7,766) | p value | IOCM (n=979) | LOCM (n=979) | p value | |
| Age (years) | 67.5±10.8 | 56.3±8.9 | <0.001 | 62.7±11.0 | 62.5.3±10.5 | 0.783 |
| Male | 1,148 (68.9) | 6,127 (78.9) | <0.001 | 716 (73.1) | 755 (71.1) | 0.045 |
| Diabetes mellitus | 514 (30.9) | 2,301 (29.6) | 0.315 | 309 (31.6) | 300 (30.6) | 0.649 |
| Hyperlipidemia | 1,091 (65.5) | 5,289 (68.1) | 0.041 | 650 (66.4) | 652 (66.6) | 0.949 |
| Hypertension | 1,151 (69.1) | 4,935 (63.5) | <0.001 | 663 (67.7) | 685 (70.0) | 0.298 |
| Smoking | 829 (49.8) | 4,652 (59.9) | <0.001 | 526 (53.7) | 552 (56.4) | 0.247 |
| OMI | 308 (18.5) | 1,517 (19.5) | 0.332 | 180 (18.4) | 208 (21.2) | 0.115 |
| Previous PCI | 408 (24.5) | 1,707 (21.9) | 0.025 | 234 (23.9) | 269 (27.5) | 0.072 |
| Previous CABG | 77 (4.6) | 183 (2.4) | <0.001 | 40 (4.1) | 38 (3.9) | 0.814 |
| STEMI | 137 (8.2) | 922 (11.9) | <0.001 | 93 (9.5) | 113 (11.5) | 0.143 |
| Stable CAD | 685 (41.1) | 3,176 (40.9) | 0.854 | 419 (42.8) | 408 (41.7) | 0.601 |
| LVEF | 62.6±7.7 | 63.3±6.9 | 0.001 | 63.2±7.6 | 62.4±7.6 | 0.022 |
| eGFR before PCI (mL/min/1.73 m2) | 87.7±20.6 | 97.8±18.9 | <0.001 | 92.5±20.1 | 91.2±20.5 | 0.169 |
| SCr before PCI (µmol/L) | 78.7±18.8 | 74.6±14.6 | <0.001 | 76.5±16.8 | 78.4±17.7 | 0.016 |
| Triple vessel lesion | 768 (46.1) | 3,117 (40.1) | <0.001 | 414 (42.3) | 3,429 (43.8) | 0.506 |
| Syntax score | 12.0±8.5 | 11.1±7.6 | <0.001 | 11.3±8.0 | 11.4±8.3 | 0.745 |
| Contrast volume (mL) | 176.2±86.0 | 167.7±83.6 | <0.001 | 170.2±83.0 | 170.4±89.3 | 0.973 |
| IABP support | 21 (1.3) | 43 (0.6) | 0.001 | 8 (0.8) | 14 (1.4) | 0.199 |
| SCr after PCI (µmol/L) | 81.3±19.4 | 80.5±15.8 | 0.088 | 78.5±17.7 | 85.0±17.9 | <0.001 |
| CIN | 28 (1.7) | 131 (1.7) | 0.988 | 15 (1.5) | 39 (4.0) | 0.001 |
Data were shown as means±standard deviation or number (%).
CABG = coronary artery bypass grafting; CAD = coronary artery disease; CIN = contrast induced nephropathy; eGFR = estimated glomerular filtration rate; IABP = intra-aortic balloon pump; IOCM = iso-osmolality contrast media; LOCM = low-osmolar contrast media; LVEF = left ventricular ejection fraction; OMI = old myocardial infarction; PCI = percutaneous coronary intervention; PSM = propensity score matching; SCr = serum creatinine; STEMI = ST elevated myocardial infarction.
RESULTS
A total of 9,431 patients (1,665 in IOCM group and 7,766 in LOCM group) were enrolled (Table 1). In LOCM group, 1,160 cases were treated with iohexol, 1,584 cases with ioversl, 1,905 cases with iopamidol and 3,117 cases with iopromide. After PSM 1,958 patients (979 in IOCM group and 979 in LOCM group) were analyzed. In LOCM group, 522 cases were treated with iohexol, 118 cases with ioversl, 113 cases with iopamidol and 226 cases with iopromide. Before PSM, compared with the LOCM group, the IOCM group were elder (p<0.001), prone to have more co-morbidities and worse basal renal and cardiac function. During procedure, IOCM group were more likely to have complex and severe coronary lesions and used IABP more frequently and used larger volume of contrast. After PSM, only male proportion, LVEF and SCr were slightly lower in IOCM group than in LOCM group.
Before PSM, according to the SCr level after PCI, the CIN were observed in 28 patients (1.7%) in IOCM group and 131 patients (1.7%) in LOCM group. Multivariate analysis showed that IOCM compared with LOCM did not significantly alter rates of CIN (odds ratio [OR], 0.912; 95% confidence interval [CI], 0.576–1.446; p=0.696). After PSM, the CIN were observed in 15 patients (1.5%) in the IOCM group and 39 patients (4.0%) in LOCM group. Multivariate analysis showed that IOCM compared with LOCM was an independent protective factor of CIN (OR, 0.393; 95% CI, 0.214–0.722; p=0.003).
Subgroup analysis was performed. Before PSM, Patients were divided into 2 groups according to LVEF, 409 patients with EF <50% and 8,763 patients with LVEF ≥50%. According to eGFR, patients were divided into 2 groups, 288 patients with eGFR <60 mL/min/1.73 m2 and 9,143 patients with eGFR ≥60 mL/min/1.73 m2 before PCI. The CIN incidence of subgroups were shown in Table 2. After PSM, we found that the CIN incidence was higher using LOCM than IOCM in LVEF ≥50% group and eGFR ≥60 mL/min/1.73 m2 group. While in other subgroups, there was no significant difference in the incidence of CIN between IOCM and LOCM.
Table 2. CIN incidence of subgroups.
| Characteristics | Before PSM | After PSM | ||||
|---|---|---|---|---|---|---|
| IOCM | LOCM | p value | IOCM | LOCM | p value | |
| LVEF <50% | 7/93 (7.5%) | 14/316 (4.4%) | 0.234 | 2/45 (4.4%) | 6/60 (10%) | 0.249 |
| LVEF ≥50% | 21/1,528 (1.4%) | 115/7,235 (1.6%) | 0.536 | 13/934 (1.4%) | 33/919 (3.6%) | 0.002 |
| eGFR <60 mL/min/1.73 m2 | 3/143 (2.1%) | 4/145 (2.8%) | 0.508 | 2/54 (3.7%) | 3/59 (5.1%) | 0.542 |
| eGFR ≥60 mL/min/1.73 m2 | 25/1,522 (2.6%) | 127/7,621 (1.7%) | 0.527 | 13/925 (1.4%) | 36/920 (3.9%) | 0.001 |
CIN = contrast induced nephropathy; eGFR = estimated glomerular filtration rate; IOCM = iso-osmolality contrast media; LOCM = low-osmolar contrast media; LVEF = left ventricular ejection fraction; PSM =propensity score matching.
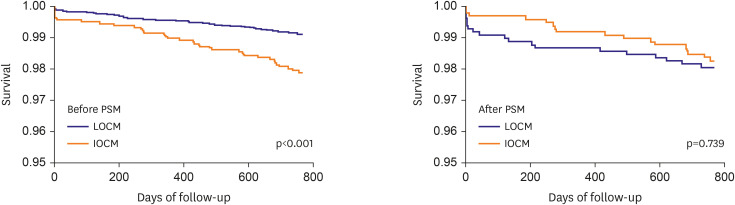
The follow-up time was 753±57 days. Before PSM, 2-year all-cause death happened in 35 patients (2.1%) in IOCM group and 69 patients (0.9%) in LOCM group, respectively. Log-rank analysis showed that all-cause mortality was significantly higher in IOCM group than LOCM group (p<0.001), Kaplan-Meier survival analysis was shown in Figure 1. Adjusted multivariate COX regression analysis showed that IOCM did not affect 2-year all-cause mortality compared with LOCM (hazard ratio [HR], 0.849; 95% CI, 0.510–1.412; p=0.528). Age, baseline SCr, LVEF and IABP support were independent predictors of 2-year all-cause death after elective PCI. After PSM, 2-year all-cause death happened in 17 patients (1.7%) in IOCM group and 19 patients (1.9%) in LOCM group, respectively. Log-rank analysis showed that all-cause mortality was not significantly different between IOCM group and LOCM group (p=0.739). Kaplan-Meier survival analysis was shown in Figure 1. Adjusted multivariate COX regression analysis showed that IOCM did not affect 2-year all-cause mortality compared with LOCM (HR, 1.037; 95% CI, 0.534–2.014; p=0.915), either. Age, baseline SCr and IABP support were independent predictors of 2-year all-cause death after elective PCI (Tables 3 and 4).
Figure 1.
Survival curves (Kaplan-Meier analysis) for all-cause mortality at 2 years.
IOCM = iso-osmolar contrast media; LOCM = low-osmolar contrast media; PSM = propensity score matching.
Table 3. Cox regression of 2-year all-cause death before PSM.
| Characteristics | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | |
| Age | 1.079 (1.057–1.101) | <0.001 | 1.069 (1.043–1.096) | <0.001 |
| Previous CABG | 2.168 (0.951–4.943) | 0.066 | 0.970 (0.388–2.420) | 0.947 |
| Previous PCI | 1.686 (1.119–2.540) | 0.012 | 1.440 (0.924–2.243) | 0.107 |
| OMI | 1.859 (1.226–2.819) | 0.004 | 1.122 (0.691–1.822) | 0.642 |
| SCr before PCI | 1.024 (1.015–1.033) | <0.001 | 1.011 (1.002–1.022) | 0.024 |
| LVEF | 0.939 (0.920–0.958) | <0.001 | 0.954 (0.932–0.977) | <0.001 |
| IABP support | 1.573 (1.334–1.855) | <0.001 | 1.315 (1.107–1.561) | 0.002 |
| IOCM vs. LOCM | 2.377 (1.583–3.570) | <0.001 | 0.849 (0.510–1.412) | 0.528 |
CABG = coronary artery bypass grafting; CI = confidence interval; HR = hazard ratio; IABP = intra-aortic balloon pump; IOCM = iso-osmolality contrast media; LOCM = low-osmolar contrast media; LVEF = left ventricular ejection fraction; OMI = old myocardial infarction; PCI = percutaneous coronary intervention; PSM = propensity score matching; SCr = serum creatinine.
Table 4. Cox regression of 2-year all-cause death after PSM.
| Characteristics | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | |
| Age | 1.045 (1.008–1.083) | 0.016 | 1.037 (1.001–1.074) | 0.042 |
| SCr before | 1.025 (1.012–1.039) | <0.001 | 1.016 (1.002–1.030) | 0.024 |
| LVEF | 0.954 (0.923–0.985) | 0.005 | 0.978 (0.941–1.016) | 0.247 |
| IABP support | 1.853 (1.555–2.708) | <0.001 | 1.662 (1.363–2.026) | <0.001 |
| IOCM vs. LOCM | 0.890 (0.463–1.713) | 0.728 | 1.037 (0.534–2.014) | 0.915 |
CI = confidence interval; HR = hazard ratio; IABP = intra-aortic balloon pump; IOCM = iso-osmolality contrast media; LOCM = low-osmolar contrast media; LVEF = left ventricular ejection fraction; PSM = propensity score matching; SCr = serum creatinine.
DISCUSSION
Both IOCM and LOCM were recommended according to the international guidelines from both European Society of Urogenital Radiology and KDIGO.7),9) However, there are still uncertainties on whether there are any significant difference in renal safety between IOCM and LOCM. This is a large retrospective cohort study comparing the CIN rate and long-term outcomes between IOCM and LOCM in Chinese patients in real world clinical practice. The patients of IOCM group were more likely to have high risk characteristics of CIN and mortality (older age, worse baseline renal and cardiac function, greater contrast volume and IABP support, et al.). Obviously, the physicians tended to choose IOCM rather than LOCM for high risk patients in clinical practice. Therefore, PSM was applied to compensate for imbalance between groups in this study. After PSM, the baseline variables were much better balanced.
In the present study, CIN incidence of IOCM and LOCM were similar before PSM. We presume that this was related to the known selection biases in IOCM group as mentioned above (older age, worse baseline renal and cardiac function, greater contrast volume and IABP support, et al.). After PSM, CIN incidence of IOCM was lower than LOCM in the cohort. This was in consistent with previous studies comparing IOCM and LOCM.3),10),11) Iodixanol is the only iodinated contrast agent that is not hyperosmolar to blood.12),13),14),15) While the osmotic diuresis of LOCM can reduce blood volume, activate renin-angiotensin system and lead to vasoconstriction. On the other hand, the decrease of blood volume will affect the renal perfusion and eventually lead to renal function damage. However, some of studies found on difference in the CIN rate between IOCM and LOCM. A meta-analysis including 36 randomized controlled trials by From et al.,5) found that there was no advantage of IOCM in comparison with LOCM in CIN.
Many studies failed to find a lower CIN incidence in IOCM compared with LOCM. There may be several reasons. First, the definitions of CIN used in different studies were not the same. Zhao et al.16) found that, the difference between IOCM and LOCM was found when CIN was defined as an absolute SCr increase (≥0.5 mg/dL) rather than a relative SCr increase (≥25%) in a meta-analysis including 2,190 patients. In addition, Newhouse reported the slight SCr fluctuation (≥25%) were observed in patients who were not exposed to contrast.17) That means some CIN definition such as an SCr increase of ≥25% was inappropriate, which has overestimated CIN. Second, the agents of LOCM used in studies were different. Specific LOCM may have different, nephrotoxicity, viscosity and pharmacokinetics. Bartosz6) in his meta-analysis found when compared with iohexol alone, iodixanol had advantages in almost all trials. In Reed et al.,18) some specific LOCM such as iomeprol was found with lower CIN incidence than IOCM, which hints nephrotoxicity, viscosity and pharmacokinetics of specific LOCM may also play a role in the happening of CIN.19),20)
As for the long-term outcomes, we found a higher mortality in IOCM group compared with LOCM reversed after PSM. Though the trend of higher survival rate of IOCM was observed in the Kaplan-Meier curve, multivariate Cox analysis showed that IOCM did not affect the 2-year all-cause mortality. In Wang et al.,21) the lower survival of IOCM compared with LOCM was also found before adjusted, then no difference between IOCM and LOCM was found after inverse probability weighing in patients receiving coronary angiography. While in our study, the overall population is of low-risk and the all-cause death rate is relatively low, so it may need longer follow-up to verify whether the lower mortality of IOCM will sustain.
There are still some limitations in this study. First of all, this study is a retrospective study in a single institution, and there may be some bias in the selection of contrast agents, which needs to be verified by a large randomized controlled study. Second, there are 4 types of LOCM with different viscosity, pharmacokinetics and nephrotoxicity, which may bring confounding factors to the result. Third, we did not monitor the SCr elevation ≥48 hours after PCI, which may have underestimated the incidence of CIN. Moreover, the study did not exclude those cases who are exposed to contrast agents repeatedly during perioperative period. And this may resulted an overestimation of CIN incidence.
In conclusion, in this retrospective study with selection bias eliminated by using PSM, we found that IOCM, compared with LOCM, significantly reduced the incidence of CIN after elective PCI, but had no significant effect on 2-year all-cause mortality.
Footnotes
Funding: This work was funded by the National Key Research and Development Program of China (2016YFC1031301).
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Du M.
- Data curation: Jiang L.
- Formal analysis: Du M.
- Funding acquisition: Yuan J.
- Investigation: Du M.
- Methodology: Du M.
- Project administration: Tang X.
- Resources: Gao Z.
- Software: Du M.
- Supervision: Xu B.
- Validation: Yuan J.
- Visualization: Du M.
- Writing - original draft: Du M.
- Writing - review & editing: Du M.
References
- 1.Seeliger E, Sendeski M, Rihal CS, Persson PB. Contrast-induced kidney injury: mechanisms, risk factors, and prevention. Eur Heart J. 2012;33:2007–2015. doi: 10.1093/eurheartj/ehr494. [DOI] [PubMed] [Google Scholar]
- 2.Mehran R, Nikolsky E. Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int Suppl. 2006:S11–S15. doi: 10.1038/sj.ki.5000368. [DOI] [PubMed] [Google Scholar]
- 3.Aspelin P, Aubry P, Fransson SG, et al. Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med. 2003;348:491–499. doi: 10.1056/NEJMoa021833. [DOI] [PubMed] [Google Scholar]
- 4.Azzalini L, Vilca LM, Lombardo F, et al. Incidence of contrast-induced acute kidney injury in a large cohort of all-comers undergoing percutaneous coronary intervention: comparison of five contrast media. Int J Cardiol. 2018;273:69–73. doi: 10.1016/j.ijcard.2018.08.097. [DOI] [PubMed] [Google Scholar]
- 5.From AM, Al Badarin FJ, McDonald FS, Bartholmai BJ, Cha SS, Rihal CS. Iodixanol versus low-osmolar contrast media for prevention of contrast induced nephropathy: meta-analysis of randomized, controlled trials. Circ Cardiovasc Interv. 2010;3:351–358. doi: 10.1161/CIRCINTERVENTIONS.109.917070. [DOI] [PubMed] [Google Scholar]
- 6.Mruk B. Renal safety of iodinated contrast media depending on their osmolarity - current outlooks. Pol J Radiol. 2016;81:157–165. doi: 10.12659/PJR.895406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–84. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 8.Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Stacul F, van der Molen AJ, Reimer P, et al. Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines. Eur Radiol. 2011;21:2527–2541. doi: 10.1007/s00330-011-2225-0. [DOI] [PubMed] [Google Scholar]
- 10.Jo SH, Youn TJ, Koo BK, et al. Renal toxicity evaluation and comparison between visipaque (iodixanol) and hexabrix (ioxaglate) in patients with renal insufficiency undergoing coronary angiography: the RECOVER study: a randomized controlled trial. J Am Coll Cardiol. 2006;48:924–930. doi: 10.1016/j.jacc.2006.06.047. [DOI] [PubMed] [Google Scholar]
- 11.McCullough PA, Bertrand ME, Brinker JA, Stacul F. A meta-analysis of the renal safety of isosmolar iodixanol compared with low-osmolar contrast media. J Am Coll Cardiol. 2006;48:692–699. doi: 10.1016/j.jacc.2006.02.073. [DOI] [PubMed] [Google Scholar]
- 12.Hossain MA, Costanzo E, Cosentino J, et al. Contrast-induced nephropathy: pathophysiology, risk factors, and prevention. Saudi J Kidney Dis Transpl. 2018;29:1–9. doi: 10.4103/1319-2442.225199. [DOI] [PubMed] [Google Scholar]
- 13.Fähling M, Seeliger E, Patzak A, Persson PB. Understanding and preventing contrast-induced acute kidney injury. Nat Rev Nephrol. 2017;13:169–180. doi: 10.1038/nrneph.2016.196. [DOI] [PubMed] [Google Scholar]
- 14.Scharnweber T, Alhilali L, Fakhran S. Contrast-induced acute kidney injury: pathophysiology, manifestations, prevention, and management. Magn Reson Imaging Clin N Am. 2017;25:743–753. doi: 10.1016/j.mric.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 15.McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008;51:1419–1428. doi: 10.1016/j.jacc.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Zhao F, Lei R, Yang SK, et al. Comparative effect of iso-osmolar versus low-osmolar contrast media on the incidence of contrast-induced acute kidney injury in diabetic patients: a systematic review and meta-analysis. Cancer Imaging. 2019;19:38. doi: 10.1186/s40644-019-0224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newhouse JH, Kho D, Rao QA, Starren J. Frequency of serum creatinine changes in the absence of iodinated contrast material: implications for studies of contrast nephrotoxicity. AJR Am J Roentgenol. 2008;191:376–382. doi: 10.2214/AJR.07.3280. [DOI] [PubMed] [Google Scholar]
- 18.Reed M, Meier P, Tamhane UU, Welch KB, Moscucci M, Gurm HS. The relative renal safety of iodixanol compared with low-osmolar contrast media: a meta-analysis of randomized controlled trials. JACC Cardiovasc Interv. 2009;2:645–654. doi: 10.1016/j.jcin.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Jost G, Lengsfeld P, Lenhard DC, Pietsch H, Hütter J, Sieber MA. Viscosity of iodinated contrast agents during renal excretion. Eur J Radiol. 2011;80:373–377. doi: 10.1016/j.ejrad.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Bucher AM, De Cecco CN, Schoepf UJ, et al. Is contrast medium osmolality a causal factor for contrast-induced nephropathy? BioMed Res Int. 2014;2014:931413. doi: 10.1155/2014/931413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang YC, Tang A, Chang D, Lu CQ, Zhang SJ, Ju S. Long-term adverse effects of low-osmolar compared with iso-osmolar contrast media after coronary angiography. Am J Cardiol. 2016;118:985–990. doi: 10.1016/j.amjcard.2016.07.017. [DOI] [PubMed] [Google Scholar]