Fig 3.
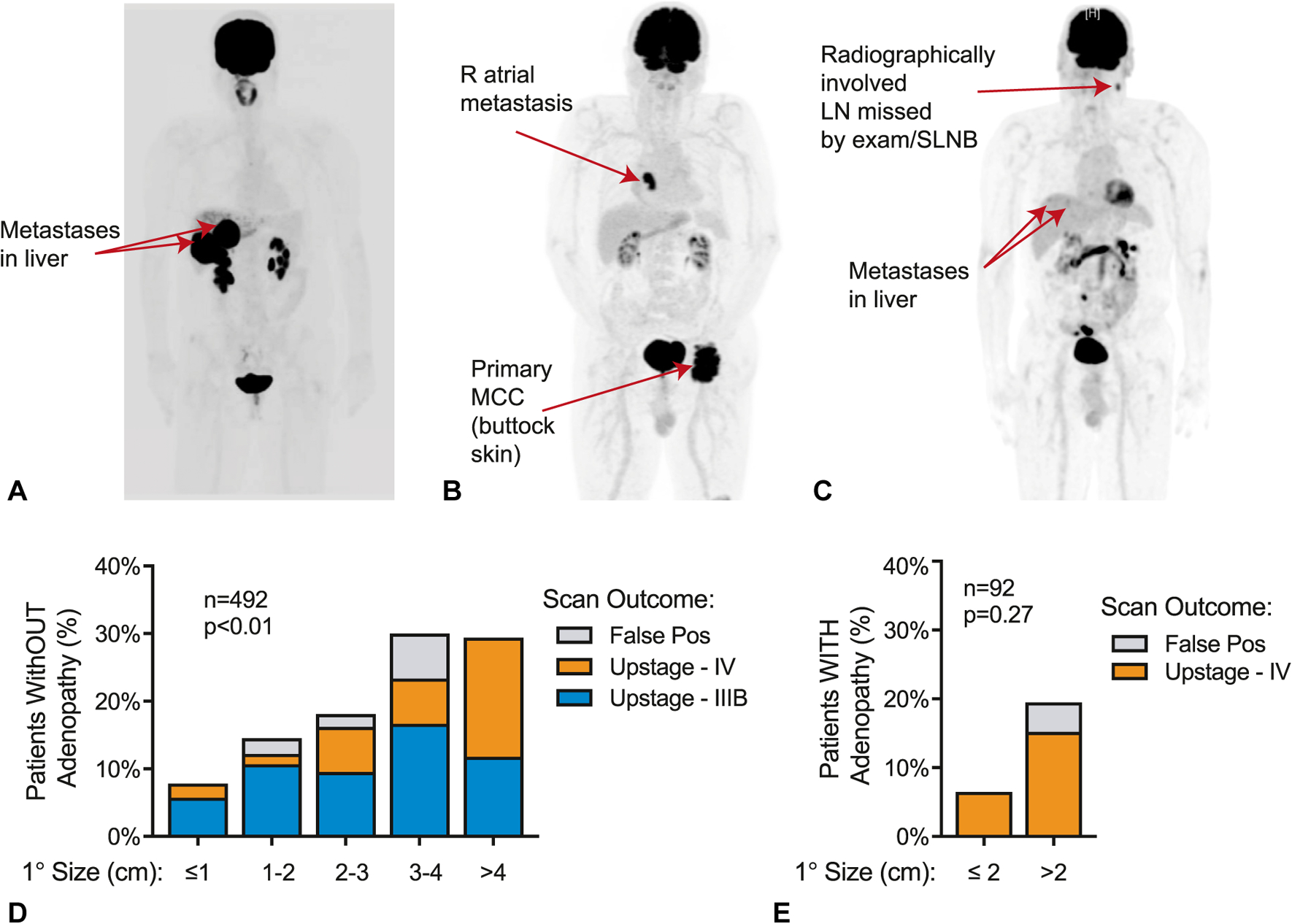
The clinical utility of baseline imaging in MCC. A–C, Three representative patients for whom baseline imaging revealed asymptomatic distant metastatic disease that was not appreciated on medical history or physical examination. Metastases were subsequently biopsy proven. A, A 55-year-old woman who presented with a 1-cm MCC primary tumor on the left medial aspect of the chest (resected before imaging); PET-CT revealed multiple hepatic metastases. B, A 85-year-old man presenting with a 10-cm primary tumor on the left buttock found to have a right atrial metastasis. C, A 74-year-old man who presented with a 1-cm primary tumor on the left temple and underwent SLNB with involvement of sentinel nodes. Subsequent PET-CT revealed additional involved regional lymph nodes (not sampled in the SLNB procedure) and distant hepatic metastases. D, Utility of baseline imaging in patients with MCC presenting without adenopathy on physical examination. Overall, 65 of 492 patients (13.2%) were found to have previously unappreciated nodal or distant metastatic spread on baseline imaging, and 7 of 492 patients (1.4%) had false positive imaging. P = .0013 for trend by primary (1°) tumor size. E, Utility of baseline imaging in patients with MCC presenting with adenopathy on physical examination. Overall, 10 of 92 patients (10.8%) were found to have previously unappreciated distant metastatic disease, and 2 of 92 (2.2%) patients had false positive imaging. P = .27 (not significant) for trend by primary tumor size. LN, Lymph node; MCC, Merkel cell carcinoma; PET-CT, positron emission tomography–computed tomography; Pos, positive; SLNB, sentinel lymph node biopsy.
