Abstract
AIMS
Examine associations of dietary strategies used to manage diabetes over time with hemoglobin A1c in youth-onset type 1 or type 2 diabetes.
METHODS
The SEARCH for Diabetes in Youth observational study assessed dietary strategies used by 1,814 participants with diabetes (n=1,558 type 1, n=256 type 2) at 2–3 research visits over 5.5 years (range 1.7–12.2). Participants reported often, sometimes, or never using 10 different dietary strategies, and use over time was categorized into 5 mutually exclusive groups: often using across visits; started using at later visits; sometimes using across visits; stopped using at later visits; or never using across visits. General multivariable linear models evaluated most recent A1c by use category for each strategy.
RESULTS
In type 1 diabetes, A1c was lower among those who starting tracking calories (−0.4%, Tukey p<0.05), often counted carbs (−0.8%, Tukey p<0.001), or sometimes chose low glycemic index foods (−0.5%, Tukey p=0.02) versus those with less use, while participants who never drank more milk had the lowest A1c (−0.5%, Tukey p=0.04). In type 2 diabetes, A1c was lower among those who often limited high fat foods (−2.0%, Tukey p=0.02) or started counting carbohydrates (−1.7%, Tukey p=0.07) than those who did so less.
CONCLUSIONS
For several dietary strategies, more frequent use over time was related to lower A1c in youth-onset type 1 and type 2 diabetes, suggesting these strategies can likely support diabetes management for this population. Investigation into factors predicting receipt of advice for specific strategies and corresponding impact on intake might be considered.
INTRODUCTION
Dietary behaviors play a key role in diabetes management (1). To support optimal behaviors in youth-onset diabetes, formal medical nutrition therapy delivered by a registered dietitian nutritionist is recommended at diagnosis and regularly thereafter, with a particular emphasis on monitoring carbohydrate intake in those with type 1 diabetes and adopting healthy eating patterns in those with type 2 diabetes (2). Individuals with diabetes may also receive less formal nutrition education or nutrition counseling from providers, and are exposed to alternative dietary strategies to manage diabetes via the lay press and peers with diabetes (3). There is moderate strength evidence to support the dietary strategy of carbohydrate counting, for which >97% of individuals with type 1 diabetes receive guidance from providers (4). Two clinical trials reported reductions of ~0.6% in pediatric type 1 diabetes patients following a carbohydrate counting intervention (5,6), and the SEARCH for Diabetes in Youth study previously reported that mean A1c was 1.1% lower among those who reported often using this dietary strategy versus those who sometimes/never did (8.3% versus 9.4%) (4). However, use of other food-based or nutrient-based dietary strategies by these individuals, as well as relationship with glycemic control, is largely unknown. Given the consistently high A1c levels in youth-onset type 1 and type 2 diabetes (7,8), further approaches to support improved glycemic control are needed. Identification of dietary strategies with potential for improving glycemic control when used over time can help guide dietary support services for this population.
Thus, the goal of this analysis was to examine associations between self-reported utilization of dietary strategies to manage diabetes over ~5 years and A1c levels in individuals with youth-onset type 1 or type 2 diabetes. We hypothesized that frequent use of any dietary strategy over time would be associated with lower A1c levels compared to less frequent use or non-use, for both type 1 and type 2 diabetes, independent of diabetes medication regimen.
METHODS
Participants
The SEARCH for Diabetes in Youth Study uses a population-based registry network at five sites in the United States to identify individuals diagnosed with any type of diabetes before twenty years of age (9). The clinical sites include the state of South Carolina; Cincinnati, Ohio and surrounding counties; the state of Colorado with southwestern US American Indian sites; Seattle, Washington, and surrounding counties; and Kaiser Permanente Southern California membership in seven counties, resulting in a catchment population of over 5.5 million children aged <20 years (10). Annual incidence of youth-onset diabetes in this population has been continuously ascertained since 2002 (11). Individuals diagnosed with type 1 or type 2 diabetes in 2002–2006 or 2008 were invited to participate in an observational cohort research study on the natural history of youth-onset diabetes by completing baseline visits shortly after diagnosis (mean 9.6 [SD 6.4] months post-diagnosis). In 2011–2015 and 2015–2019, two follow-up visits were conducted among those with ≥5 years diabetes duration for assessment of health care quality, diabetes-related early complications, quality of life, and related characteristics. The study was approved by the institutional review boards with jurisdiction in each study location. All participants provided consent or assent as age-appropriate, and parents also provided consent for those aged <18 years.
The first follow-up visit was completed by 2,777 participants at a mean age of 17.9 years (SD 4.8) and mean diabetes duration of 8.0 years (SD 2.0). The distribution of demographic, metabolic, and socioeconomic characteristics of participants who completed the first follow-up visit were similar to those of the larger SEARCH registry population (12). The second follow-up visit was completed by 2,668 participants at a mean age of 21.5 years (SD 5.1) and a mean diabetes duration of 11.2 years (SD 3.3). By design, approximately half of participants with type 1 diabetes who were non-Hispanic white were invited to complete in-person research visits (target n~700), with the rest invited to complete only web-based questionnaires, as it was determined a priori that the statistical power gained by conducting in-person research visits on all non-Hispanic white type 1 participants was incremental relative to the resources required to do so. Thus, participant characteristics for the second follow-up visit intentionally differed from that of the larger SEARCH registry population in terms of enriched representation of participants with type 1 diabetes who were non-white and participants with type 2 diabetes (all races/ethnicities). Additionally, participants who declined an in-person research visit were invited to complete web-based questionnaires only. Altogether, this resulted in a total of 995 individuals (37% of 2,668) who completed only questionnaires at the second follow-up visit.
Data collection
Trained research staff conducted the in-person baseline and follow-up research visits. Participants (and/or parents, for younger participants) self-reported date of birth, sex, race, ethnicity, highest parental education, annual household income, type of health insurance, and diabetes treatment regimen. Date of diagnosis had been obtained previously from medical records during case ascertainment, and was used to calculate age of diagnosis and diabetes duration at each research visit. Participants were instructed to fast overnight for ≥8 hours and abstain from medications (including short-acting insulin) on the morning of the visit. Blood samples were obtained and analyzed for hemoglobin A1c at the central laboratory (Northwest Lipid Metabolism and Diabetes Research, Seattle, WA). Questionnaires were used to assess ten dietary strategies to manage diabetes: 1) keep track of calories, 2) count carbohydrates, 3) choose low glycemic index foods, 4) use dietary exchanges, 5) keep track of fat grams, 6) limit sweets, 7) limit high fat foods, 8) drink more milk, 9) eat more fruits and vegetables, and 10) eat more fiber and whole grains. For each strategy, participants were asked if they had ever received advice on that strategy from a provider (yes, no, don’t know), and how often they used each strategy (often, sometimes, never).
Statistical analyses
This analysis included participants with a) a provider diagnosis of type 1 or type 2 diabetes, b) data on dietary strategies from ≥2 visits, and c) an A1c result from the most recent visit with dietary strategy data. We classified use over time for each of the 10 dietary strategies with five categories: often using (often using at every visit, or sometimes using at earlier visits with often using at the most recent visit), started using (never using at earlier visits with sometimes/often using at later visits), sometimes using (sometimes using at every visit, or often using at earlier visits with sometimes using at the most recent visit), stopped using (sometimes or often using at earlier visits with never using at later visits), and never using (not using at any visit). For most strategies, 5% or fewer participants reported inconsistent/intermittent use (never using at the first and last visit but sometimes/often using in the middle, or vice versa), which did not align with any of the previously described categories, and were excluded from the analysis due to the small cell size that would impede interpretation.
We used general linear regression, stratified by diabetes type, to evaluate the relationship between categorized use of each dietary strategy and current A1c. We fit separate models for each strategy, resulting in 20 models total. When the overall p-value for the dietary strategy use variable was <0.05, we examined Tukey-adjusted pairwise comparisons for each pair of categories. Models were adjusted for age at diagnosis (years), sex (male, female), race/ethnicity (non-Hispanic white, all others), baseline parental education (did not graduate high school, graduated high school), health insurance status at the most recent visit (private, all others), SEARCH study site (California, Colorado, Ohio, South Carolina, Washington), diabetes duration at the most recent visit (years), and treatment regimen at the most recent visit (type 1: insulin pump, all others; type 2: insulin pump, other insulin, non-insulin, no medication), and self-reported receipt of provider guidance for using that strategy (ever, never, don’t know). The adjustment for having been advised on the use of a particular strategy was excluded if >90% of observations reported receiving the advice. Analyses were conducted in SAS v9.4 (Cary, NC) with two-sided alpha for statistical significance set at 0.05.
RESULTS
Of the 2,777 participants who completed the first and/or second follow-up visit, we excluded 24 who did not have a provider diagnosis of type 1 or type 2 diabetes (i.e., had a provider diagnosis of other/unknown diabetes), 441 who did not have sufficient dietary strategy data, and 498 who did not have A1c data, resulting in an analytic sample of 1,814 participants (1,558 type 1 and 256 type 2). Of these, 1,219 (67%) contributed data from two visits and 595 (33%) contributed data from three visits. Participant characteristics at the baseline and most recent follow-up visits are presented in Table 1, stratified by diabetes type. On average, the first research visit from which dietary strategy data is available occurred approximately 5.8 years after diagnosis, and the most recent visit occurred approximately 5.5 years later.
Table 1.
Characteristics of SEARCH participants that completed 2–3 questionnaires on use of dietary strategies to manage diabetes over (mean) 5.5 years and provided a blood sample for analysis of hemoglobin A1c at the last follow-up visit (n=1,814).
| Type 1 diabetes |
Type 2 diabetes |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline visit |
Last follow-up visit |
Baseline visit |
Last follow-up visit |
|||||
| N | Mean (SD) or count (%) | N | Mean (SD) or count (%) | N | Mean (SD) or count (%) | N | Mean (SD) or count (%) | |
| Female (n) | 1558 | 820 (52.6) | 256 | 166 (64.8) | ||||
| Non-Hispanic white (n) | 1557 | 1106 (71.0) | 256 | 60 (23.4) | ||||
| Age at diagnosis (years) | 1558 | 9.1 (4.4) | 256 | 14.2 (2.7) | ||||
| Age at visit (years) | 1558 | 10.0 (4.4) | 1558 | 20.4 (5.0) | 256 | 15.1 (2.7) | 256 | 26.3 (3.6) |
| Diabetes duration (years) | 1558 | 0.8 (0.5) | 1558 | 11.2 (2.6) | 256 | 0.9 (0.6) | 256 | 12.1 (2.3) |
| Parental education (n) | 1539 | 1514 | 247 | 236 | ||||
| <High school graduate | 53 (3.4) | 56 (3.7) | 44 (17.8) | 25 (10.6) | ||||
| High school graduate or higher | 1486 (96.6) | 1458 (96.3) | 203 (82.2) | 211 (89.4) | ||||
| Annual household income (n) | 1541 | 1551 | 252 | 255 | ||||
| <$25,000 | 212 (13.8) | 218 (14.1) | 106 (42.1) | 87 (34.1) | ||||
| $25,000 – $49,999 | 312 (20.2) | 249 (16.1) | 60 (23.8) | 54 (21.2) | ||||
| $50,000 – $74,999 | 319 (20.7) | 212 (13.7) | 30 (11.9) | 14 (5.5) | ||||
| ≥$75,000 | 584 (37.9) | 525 (33.8) | 17 (6.7) | 15 (5.9) | ||||
| Do not know/refused | 114 (7.4) | 347 (22.4) | 39 (15.5) | 85 (33.3) | ||||
| Health insurance (n) | 1542 | 1543 | 253 | 245 | ||||
| Private | 1219 (79.1) | 1167 (75.6) | 122 (48.2) | 111 (45.3) | ||||
| Medicare/Medicaid | 270 (17.5) | 232 (15.0) | 108 (42.7) | 68 (27.8) | ||||
| Other | 31 (2.0) | 85 (5.5) | 12 (4.7) | 24 (9.8) | ||||
| None | 22 (1.4) | 59 (3.8) | 11 (4.3) | 42 (17.1) | ||||
| Diabetes treatment (n)† | 1180 | 1546 | 169 | 237 | ||||
| Pump | 88 (7.5) | 890 (57.6) | 1 (0.6) | 12 (5.1) | ||||
| Other Insulin | 1077 (91.3) | 638 (41.3) | 58 (34.3) | 121 (51.1) | ||||
| Non-Insulin only | 11 (0.9) | 6 (0.4) | 92 (54.4) | 43 (18.1) | ||||
| None | 4 (0.3) | 12 (0.8) | 18 (10.7) | 61 (25.7) | ||||
| Hemoglobin A1c (%) | 1347 | 7.7 (1.5) | 1558 | 9.0 (1.9) | 237 | 7.1 (2.1) | 256 | 9.5 (3.0) |
| Hemoglobin A1c (mmol/mol) | 1347 | 60.5 (16.4) | 1558 | 75.1 (21.2) | 237 | 54.5 (22.7) | 256 | 80.1 (32.3) |
Insulin regimen not available at baseline for phase 2 participants - baseline treatment category reported for phase 1 participants only
The proportions of participants often, sometimes, or never using each strategy at the first and most recent visits are presented in Supplemental Figures 1 (type 1 diabetes) and 2 (type 2 diabetes). For type 1 diabetes, the proportion of participants often using each strategy declined by 3–15% % from the first visit (mean 5.8 years diabetes duration) to the most recent visit (mean 11.2 years diabetes duration), reflecting a slight but consistent decrease in use of these dietary strategies to manage diabetes over ~5 years in the overall sample. Only the strategies of counting carbohydrates and eating more fruits/vegetables were consistently used by ≥50% or more of participants at each visit. For type 2 diabetes, the proportion of participants often using each strategy at the first visit (mean 6.2 years diabetes duration) remained stable (±1%) to the most recent visit (mean 12.1 years diabetes duration) for three strategies, increased by 6–9% for five strategies, and decreased by 6% for two strategies, reflecting a slight variability in the use of these dietary strategies to manage diabetes over ~5 years in the overall sample. Only the strategies of limiting sweets and eating more fruits/vegetables were used by ≥40% or more of participants at each visit.
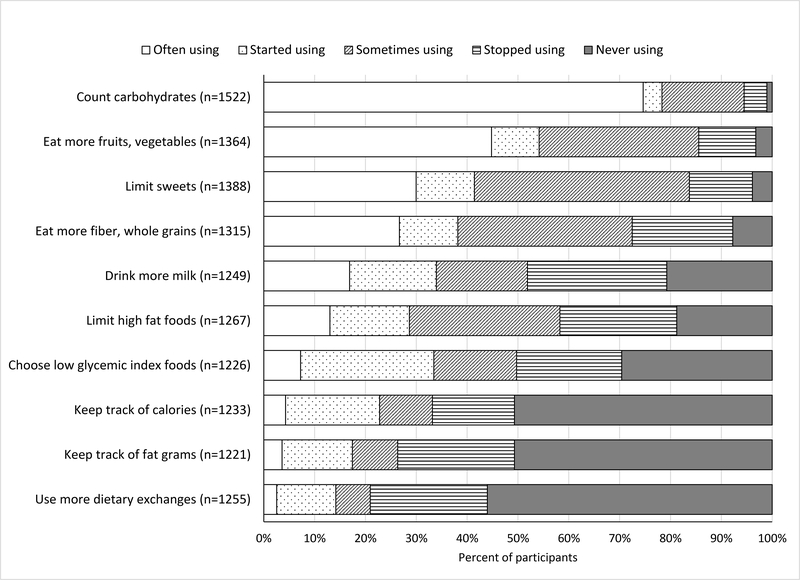
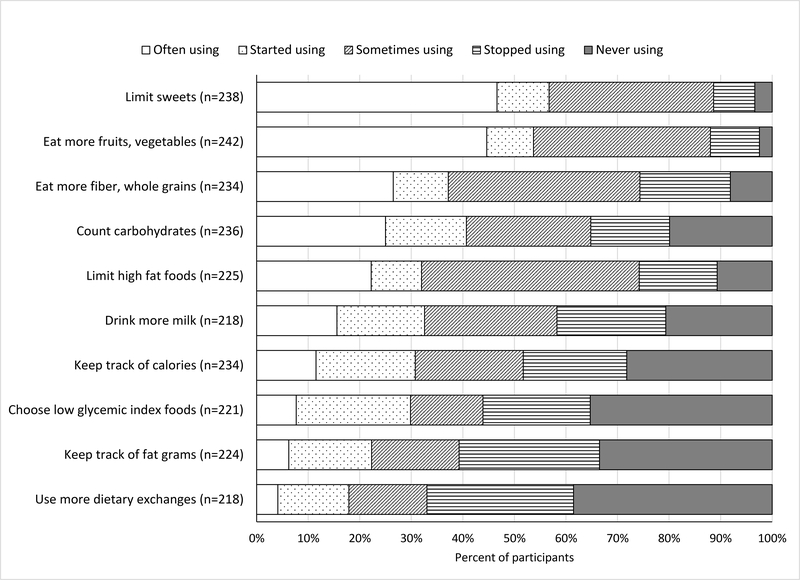
Examination of use over time within individual participants indicated that the dietary strategy used most frequently over time in type 1 diabetes was carbohydrate counting (75% often using), while the strategy used least frequently over time was dietary exchanges (56% never using) (Figure 1). For participants with type 2 diabetes (Figure 2), the dietary strategies used most frequently over time were limiting sweets and eating more fruits and vegetables (47% and 45% often using, respectively), while the strategy used least frequently over time was dietary exchanges (39% never using).
Figure 1.
Participant-reported use of dietary strategies over time to manage Type 1 diabetes
Figure 2.
Participant-reported use of dietary strategies over time to manage Type 2 diabetes
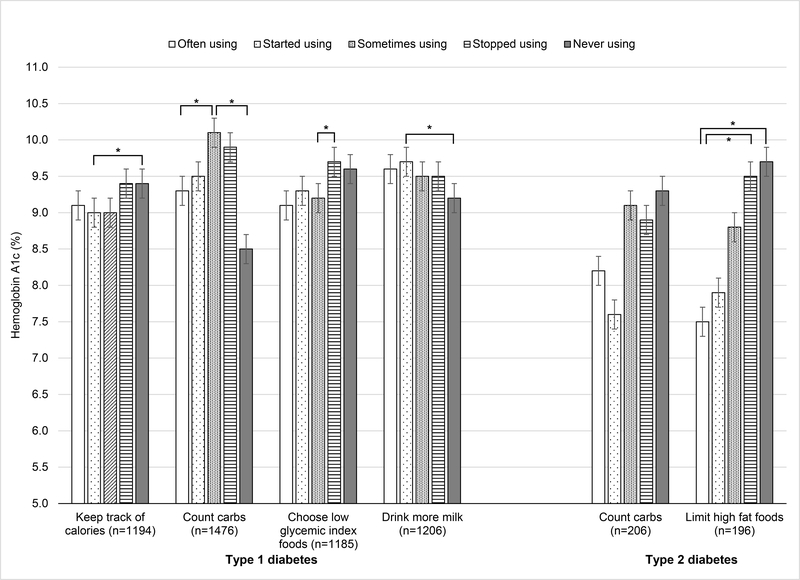
Adjusted mean A1c levels stratified by use of each dietary strategy are presented in Supplemental Table 1 (all results) and Figure 3 (statistically significant results). Four dietary strategies were significant associated with A1c in type 1 diabetes: keeping track of calories, counting carbohydrates, choosing low glycemic index foods, and drinking more milk. For tracking calories, mean A1c was ~0.4% lower among participants who often, started, or sometimes tracked calories compared to those who stopped or never tracked calories; however, the pairwise comparison was statistically significant only for the started versus never groups (9.0% [SE 0.2] versus 9.4% [SE 0.2], Tukey p=0.047). For counting carbohydrates, participants who often or started to count carbohydrates had a mean A1c that was 0.4–0.8% lower than those who sometimes or stopped counting carbohydrates, with the pairwise comparison being statistically significant for the often versus sometimes comparison (9.3% [SE 0.1] versus 10.1% [SE 0.2], Tukey p<0.001). Further, the lowest A1c (8.5% [SE 0.5]) was observed among participants who reported never counting carbohydrates, but was significantly different only from those who sometimes counted carbohydrates (Tukey p=0.01). For choosing low glycemic index foods, mean A1c was 0.3–0.6% lower among those who often, started, or sometimes used this strategy compared to those who stopped or never used it; the pairwise comparison was statistically significant only for the sometimes versus stopped groups (9.2% [SE 0.2] versus 9.7% [SE 0.2], Tukey p=0.02). Last, for drinking more milk, participants who reported never drinking more milk had a mean A1c that was 0.3–0.5% lower than the other groups, with the pairwise comparison significantly different only from the started group (9.2% [SE 0.2] versus 9.7% [SE 0.2], Tukey p=0.04)
Figure 3.
Adjusted mean A1c by dietary strategy use over time to manage diabetes
*Tukey p<0.05 for pairwise comparison. Models are adjusted for: age at diagnosis, gender, race/ethnicity, baseline parental education, current insurance status, duration of diabetes, diabetes medication (type 1: Pump Y/N, type 2: Pump, other insulin, non-insulin only, none), and received provider advice to use the relevant dietary strategy ever/never/DK (excluded if >90% recommendation rate: carbohydrates, limit sweets, fruits for both type 1 and type 2, fat foods and fiber for type 2), as well as clinical site.
Two dietary strategies were significantly associated with A1c in type 2 diabetes: counting carbohydrates and limiting high fat foods. For counting carbohydrates, mean A1c was 0.7–1.7% lower among those who often or started counting carbohydrates than to those who sometimes, stopped, or never counted carbohydrates; however, none of the pairwise comparisons reached statistical significance at the Tukey-adjusted level. For limiting high fat foods, mean A1c was 0.9–2.2% lower among those who often or started limiting high fat foods than those who sometimes, stopped, or never limited high fat foods; however, the pairwise comparison was statistically significant only for the often versus stopped comparison (7.5% [SE 0.5] versus 9.5% [SE 0.6], Tukey p=0.02) and the often versus never comparison (7.5% [SE 0.5] versus 9.7% [SE 0.6], Tukey p=0.01).
DISCUSSION
We found that use of dietary strategies to manage diabetes over time varies widely between individuals with youth-onset type 1 or type 2 diabetes. For participants with type 1 diabetes, more frequent tracking of calories, counting carbohydrates, or choosing low glycemic index foods was associated with lower mean A1c levels, while drinking more milk had the opposite pattern. For participants with type 2 diabetes, more frequent counting carbohydrates or limiting high fat foods was associated with lower mean A1c. Our study indicates that several dietary strategies hold promise for glycemic control in youth-onset diabetes independent of medication regimen.
In line with clinical guidelines (2), the dietary strategy used most often to manage type 1 diabetes over time was counting carbohydrates. We observed high use of carbohydrate counting at each visit, and across visits, which was associated with lower mean A1c more than 10 years after diagnosis. The reduction in A1c associated with carbohydrate counting observed here (−0.8%) is similar to the −0.6% reductions reported by clinical trials of carbohydrate counting interventions for pediatric type 1 diabetes patients (5,6). Thus, these data affirm this first-line approach to dietary management of type 1 diabetes. Surprisingly, the lowest A1c was observed among participants who reported never counting carbohydrates. We do note that only 16 participants (1% of our sample) were in this group, indicating that very few youth and young adults with type 1 diabetes have never counted carbohydrates. It is plausible that these individuals were not counting carbohydrates because their glucose levels were already effectively managed with medication or other dietary strategies. However, mean A1c in this group was 8.5%, which is above the recommended goal of <7% (2); thus, there remains room for improvement in glycemic control.
We also observed lower A1c levels among participants with type 1 diabetes who reported keeping track of calories or choosing low glycemic index foods over time. The magnitude of the benefit for A1c with these strategies was approximately half of the benefit we observed for carbohydrate counting (~0.4% versus 0.8%). However, the consistent association of lower A1c with any intensity of continued use over time suggests that they do have potential for supporting glycemic control, even if participants are able to apply these strategies only occasionally. Few participants used them often at any visit (~10%) or across visits (~5%), and approximately 50% reported never or no longer using them, indicating these potentially beneficial strategies are being underutilized, and may need more endorsement in clinical management of type 1 diabetes. In contrast, approximately 4 of 5 participants reported using the dietary strategy of drinking more milk at some point during the study, but this was associated with higher mean A1c. This strategy was included because of the noted association between vitamin D and insulin resistance nationally (14), which has SEARCH confirmed in cross-sectional analyses of type 1 diabetes (15). However, the present data indicate that drinking more milk is not a dietary strategy to encourage for type 1 diabetes patients; given the high reported use of this strategy, patient education to discourage use may be warranted.
For type 2 diabetes, counting carbohydrates appears to benefit glycemic control as it does for type 1 diabetes. Indeed, the difference between those who often or started counting carbs and those who sometimes, stopped, or never did was greater in type 2 diabetes (mean −1.2%) than in type 1 diabetes (mean −0.8%). None of the pairwise comparisons were statistically significant in type 2 diabetes at the Tukey-adjusted level, which could have been influenced by small cell sizes (n<60 for each of the 5 use categories). Yet, the overall pattern suggests that counting carbohydrates may have benefit for adolescents and young adults with type 2 diabetes. This strategy is being notably underutilized, with only one-third reporting often using it at any time in the first decade post-diagnosis. Our data suggest that this strategy should be promoted more for dietary management of youth-onset type 2 diabetes, in which providers may be able to extend their successful clinical approaches for promoting carbohydrate counting in type 1 diabetes to patients with youth-onset type 2 diabetes.
The dietary strategy of limiting high fat foods was also associated with better glycemic control in type 2 diabetes, with those often using it over time exhibiting an A1c more than 2.0% lower than those who never used it. This finding aligns with dietary results from the Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study, which showed that females with stable or reduced intake of saturated fat over 24 months had lower A1c than females with increased saturated fat intake (16). This result also aligns with dietary recommendations for type 2 diabetes that emphasize eating a healthy diet (more nutrient-dense foods and fewer calorie-dense/nutrient-poor foods) (2), affirming this first-line approach to dietary management in this population. However, uptake among patients is notably low, with only 1 in 5 of our participants often using this strategy and 1 in 4 never or no longer using this strategy in the first decade post-diagnosis. As above, these data highlight an opportunity for increased attention to supporting the dietary strategy of limiting high fat food intake in youth-onset type 2 diabetes.
At the cohort level, we observed remarkable consistency in the overall proportion of participants using each strategy often, sometimes, or never over ~5 years diabetes duration. This suggests that the dietary strategies being used by participants over time are relatively static. However, by examining use over time at an individual level, we determined that approximately 50% of participants changed their use of dietary strategies during that period. This could reflect a necessary adaptation of dietary strategies in response to changing life circumstances, a clinical approach recommended by diabetes care organizations (2). Or, this could reflect the challenge of maintaining use of these dietary strategies over time. Regardless, our results emphasize the need to tailor dietary support to individual circumstances, including the consideration of dietary strategies not frequently associated with a specific diabetes type but may yet be beneficial.
A remaining question is how well self-reported use of these dietary strategies for either diabetes type translates to measurable differences in actual dietary intake, which is the ostensible mediator between self-reported use of dietary strategies and A1c. For example, participants who report often using dietary exchanges may not be very proficient in doing so, which would minimize between-group differences in A1c. We speculate that, at an individual level, participants who are reporting use of a particularly strategy, regardless of proficiency, likely have better A1c control than they would if they were not attempting to manage their diabetes in that way. If baseline dietary intake is quite poor, as has been reported in youth-onset diabetes (19), then incremental changes in intake that are captured here by self-reported use of dietary strategies may not be enough to impact A1c. This could explain why only 4 and 2 of 10 strategies for type 1 and type 2 diabetes, respectively, were significantly related to A1c. Investigation of how use of these dietary strategies over time matches with dietary intake over time can identify those individuals who are successfully using these strategies, and further clarify how much of a potential benefit specific strategies may have in management of youth-onset diabetes. Understanding the individual- and provider-level factors that predict who receives specific dietary recommendations can also highlight subgroups most at risk of not getting sufficient dietary support and thereby missing out on any potential benefits for disease management. Overall, we note that A1c is higher than recommended in all participants (2), regardless of self-reported use of any particular dietary strategy. This highlights the need for additional glycemic control strategies in this population, such as intensification of therapy, or addressing social determinants of health like barriers to health care access (20,21) and food insecurity (22) that are associated with higher A1c.
Our study has strengths and limitations. Our large sample had geographic and racial/ethnic diversity, and included adolescents and young adults with either type 1 or type 2 youth-onset diabetes. The longitudinal design allowed us to examine how use of dietary strategies changes over time and is related to current A1c, which is more informative than cross-sectional analyses alone. However, this longitudinal design increased the number of use categories, which resulted in small cell sizes for some strategies and may have resulted in limited power for pairwise comparisons. We examined A1c for each dietary strategy individually without adjusting for use of other strategies, and thus cannot comment on the potential benefit of specific combinations of strategies, or potential confounding between strategies. Further, we did not include multiple measures of A1c over time, and thus cannot draw conclusions about the impact of A1c on sustained versus variable use of dietary strategies over time. The number of statistical tests we performed could have contributed to type 1 error; however, all comparisons were specified a priori and we interpreted pairwise tests at a conservative Tukey-adjusted p-value. By adjusting for sociodemographic and clinical factors known to be related to glycemic control, we provide robust evidence that dietary strategies may support diabetes management via A1c reductions of 0.4%−2.2%, which is similar to the differences in A1c we previously reported between SEARCH participants who transitioned to more versus less intensive insulin regimens over 24 months (23).
In conclusion, we found that for several dietary strategies, adolescents and young adults with youth-onset type 1 or type 2 diabetes with more frequent use over time have improved glycemic control. These results suggest that specific strategies likely can support diabetes management, above and beyond pharmacological treatment. However, the promising dietary strategies identified herein were often used by few participants consistently over time, indicating an opportunity to increase clinical support to promote these behaviors. Further investigation into the factors predicting who receives such recommendations and how that translates to true improvements in dietary intake is needed.
Supplementary Material
ACKNOWLEDGEMENTS
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible. The authors wish to acknowledge the involvement of the Kaiser Permanente Southern California’s Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group); the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina, NIH/National Center for Advancing Translational Sciences (NCATS) grant number UL1 TR000062, UL1 Tr001450; Seattle Children’s Hospital and the University of Washington, NIH/NCATS grant number UL1 TR00423; University of Colorado Pediatric Clinical and Translational Research Center, NIH/NCATS grant Number UL1 TR000154; the Barbara Davis Center at the University of Colorado at Denver (DERC NIH grant number P30 DK57516); the University of Cincinnati, NIH/NCATS grant number UL1 TR000077, UL1 TR001425; and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions.
FUNDING
Grant Support (SEARCH 1, 2, 3):
SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases.
Grant Support (SEARCH 4):
The SEARCH for Diabetes in Youth Cohort Study (1UC4DK108173) is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and supported by the Centers for Disease Control and Prevention.
The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, U18DP006139) is funded by the Centers for Disease Control and Prevention and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Sites (SEARCH 1 through 4):
Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235-4, U01 DP000244, and U18DP002710-01), Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200-2010-35171)
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Role of the Sponsors. K.R.S., an employee of the Centers for Disease Control and Prevention, is a member of the Writing Group for this manuscript because of the cooperative funding agreement. She was not involved in the collection, management, and analysis of the data, but was involved in results interpretation, manuscript review, and the decision to submit the manuscript for publication.
Footnotes
Duality of Interest. R.B.D. reports personal fees from Amgen and KCI outside the submitted work. The other authors declared no conflicts of interest.
REFERENCES
- 1.American Diabetes Association. 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S48–S65 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. 13. Children and Adolescents: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S163–S182 [DOI] [PubMed] [Google Scholar]
- 3.Patton SR, Clements MA, George K, Goggin K. “I Don’t Want Them to Feel Different”: A Mixed Methods Study of Parents’ Beliefs and Dietary Management Strategies for Their Young Children with Type 1 Diabetes Mellitus. J Acad Nutr Diet 2016;116:272–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The NS, Crandell JL, Thomas J, Couch SC, Shah AS, Maahs DM, Dabelea D, Marcovina SM, D’Agostino RB Jr., Mayer-Davis EJ, SEARCH for Diabetes in Youth Study Group. Correlates of medical nutrition therapy and cardiovascular outcomes in youth with type 1 diabetes. J Nutr Educ Behav 2013;45:661–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goksen D, Atik Altinok Y, Ozen S, Demir G, Darcan S. Effects of carbohydrate counting method on metabolic control in children with type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol 2014;6:74–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marigliano M, Morandi A, Maschio M, Sabbion A, Contreas G, Tomasselli F, Tommasi M, Maffeis C. Nutritional education and carbohydrate counting in children with type 1 diabetes treated with continuous subcutaneous insulin infusion: the effects on dietary habits, body composition and glycometabolic control. Acta Diabetol 2013;50:959–964 [DOI] [PubMed] [Google Scholar]
- 7.Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, Marcovina S, Pihoker C, Standiford D, Waitzfelder B, Mayer-Davis E, SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr 2009;155:668–672 e661–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik F, Sauder K, Isom S, Roberts A, Mayer-Davis E,Dolan L, Dabelea D, Lawrence J, Pihoker C. Trends in Glycemic Control among Youth with Diabetes: The Search for Diabetes in Youth Study. In American Diabetes Association 80th Scientific Sessions; Chicago, IL, 2020 [Google Scholar]
- 9.Search for Diabetes in Youth Study Group, Liese AD, D’Agostino RB Jr., Hamman RF, Kilgo PD, Lawrence JM, Liu LL, Loots B, Linder B, Marcovina S, Rodriguez B, Standiford D, Williams DE. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics 2006;118:1510–1518 [DOI] [PubMed] [Google Scholar]
- 10.Hamman RF, Bell RA, Dabelea D, D’Agostino RB Jr., Dolan L, Imperatore G, Lawrence JM, Linder B, Marcovina SM, Mayer-Davis EJ, Pihoker C, Rodriguez BL, Saydah S, SEARCH for Diabetes in Youth Study Group. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, Imperatore G, Linder B, Marcovina S, Pettitt DJ, Pihoker C, Saydah S, Wagenknecht L, SEARCH for Diabetes in Youth Study Group. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N Engl J Med 2017;376:1419–1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dabelea D, Stafford JM, Mayer-Davis EJ, D’Agostino R Jr., Dolan L, Imperatore G, Linder B, Lawrence JM, Marcovina SM, Mottl AK, Black MH, Pop-Busui R, Saydah S, Hamman RF, Pihoker C, SEARCH for Diabetes in Youth Study Group. Association of Type 1 Diabetes vs Type 2 Diabetes Diagnosed During Childhood and Adolescence With Complications During Teenage Years and Young Adulthood. JAMA 2017;317:825–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore CE, Murphy MM, Holick MF. Vitamin D intakes by children and adults in the United States differ among ethnic groups. J Nutr 2005;135:2478–2485 [DOI] [PubMed] [Google Scholar]
- 14.Scragg R, Sowers M, Bell C, Third National H, Nutrition Examination S. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 2004;27:2813–2818 [DOI] [PubMed] [Google Scholar]
- 15.The NS, Crandell JL, Lawrence JM, King IB, Dabelea D, Marcovina SM, D’Agostino RB Jr., Norris JM, Pihoker C, Mayer-Davis EJ. Vitamin D in youth with Type 1 diabetes: prevalence of insufficiency and association with insulin resistance in the SEARCH Nutrition Ancillary Study. Diabet Med 2013;30:1324–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kriska A, El Ghormli L, Copeland KC, Higgins J, Ievers-Landis CE, Levitt Katz LE, Trief PM, Wauters AD, Yasuda PM, Delahanty LM, Group TS. Impact of lifestyle behavior change on glycemic control in youth with type 2 diabetes. Pediatr Diabetes 2018;19:36–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S66–S76 [DOI] [PubMed] [Google Scholar]
- 18.Franz MJ, MacLeod J, Evert A, Brown C, Gradwell E, Handu D, Reppert A, Robinson M. Academy of Nutrition and Dietetics Nutrition Practice Guideline for Type 1 and Type 2 Diabetes in Adults: Systematic Review of Evidence for Medical Nutrition Therapy Effectiveness and Recommendations for Integration into the Nutrition Care Process. J Acad Nutr Diet 2017;117:1659–1679 [DOI] [PubMed] [Google Scholar]
- 19.Mayer-Davis EJ, Nichols M, Liese AD, Bell RA, Dabelea DM, Johansen JM, Pihoker C, Rodriguez BL, Thomas J, Williams D, SEARCH for Diabetes in Youth Study Group. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc 2006;106:689–697 [DOI] [PubMed] [Google Scholar]
- 20.Liese AD, Ma X, Reid L, Sutherland MW, Bell BA, Eberth JM, Probst JC, Turley CB, Mayer-Davis EJ. Health care access and glycemic control in youth and young adults with type 1 and type 2 diabetes in South Carolina. Pediatr Diabetes 2019;20:321–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Snyder LL, Stafford JM, Dabelea D, Divers J, Imperatore G, Law J, Lawrence JM, Pihoker C, Mayer-Davis EJ. Socio-economic, demographic, and clinical correlates of poor glycaemic control within insulin regimens among children with Type 1 diabetes: the SEARCH for Diabetes in Youth Study. Diabet Med 2019;36:1028–1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendoza JA, Haaland W, D’Agostino RB, Martini L, Pihoker C, Frongillo EA, Mayer-Davis EJ, Liu LL, Dabelea D, Lawrence JM, Liese AD. Food insecurity is associated with high risk glycemic control and higher health care utilization among youth and young adults with type 1 diabetes. Diabetes Res Clin Pract 2018;138:128–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pihoker C, Badaru A, Anderson A, Morgan T, Dolan L, Dabelea D, Imperatore G, Linder B, Marcovina S, Mayer-Davis E, Reynolds K, Klingensmith GJ, SEARCH for Diabetes in Youth Study Group. Insulin regimens and clinical outcomes in a type 1 diabetes cohort: the SEARCH for Diabetes in Youth study. Diabetes Care 2013;36:27–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.