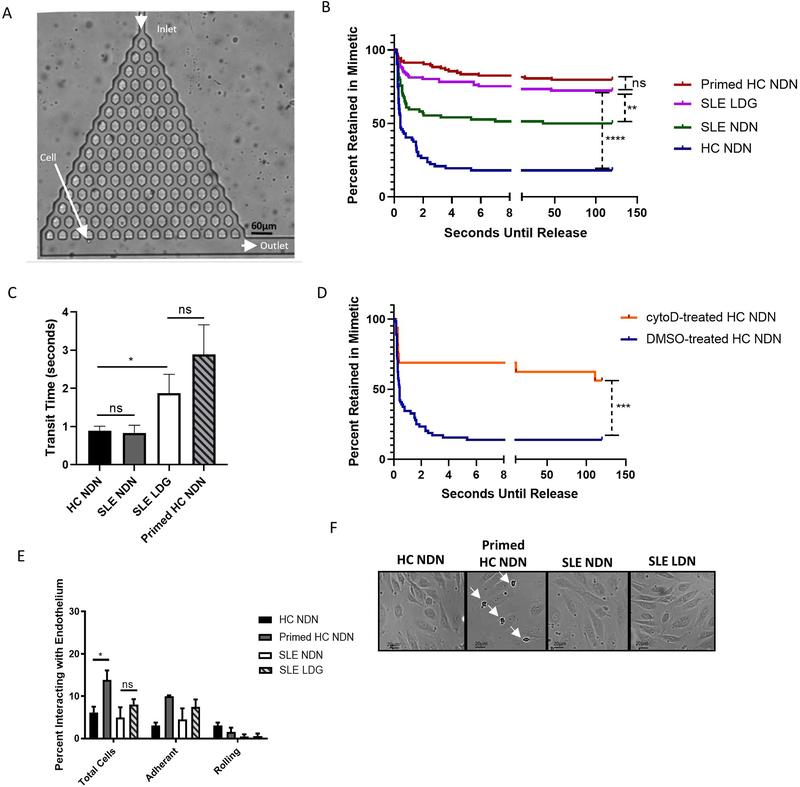
Figure 5. SLE LDGs are increasingly retained within a three-dimensional pulmonary microvasculature mimetic, but do not display enhanced adherence to endothelial cells in a two-dimensional system of flow.
(A) A branching microfluidic mimetic of the pulmonary microvasculature was designed. Arrows indicate the inlet, outlet, and a cell navigating the network, 10x objective. (B) Retention of NDNs and LDGs in the microvasculature mimetic (n>150 neutrophils per subset from n=6 HC volunteers and n=6 SLE patients). Seconds until release refers to the amount of time each neutrophil was retained within the mimetic, measured from entry at the inlet to exit at an outlet. Seconds until release was recorded as >120 seconds if cells did not exit the mimetic within the two-minute video. Times were determined manually with a timer superimposed on the video during data collection. Significance was determined by log-rank test. (C) Transit times through the microvasculature mimetic for all NDNs and LDGs navigating the entire device. Significance assessed by Mann-Whitney U-test. (D) Retention of HC NDNs treated with DMSO or cytochalasin D in the microvasculature mimetic (n>50 neutrophils from n=3 HC volunteers). Significance was determined by log-rank test. (E) Percentage of neutrophils interacting with endothelium under 0.4mL/min flow. Significance was determined by Kruskal-Wallis test with post hoc Dunn’s tests for multiple comparisons. (F) Light microscopy of neutrophil binding to endothelium post-flow assay. Arrows show enhanced binding of primed NDNs. Images representative of n=4 images obtained for each neutrophil subset isolated from n=6 SLE patients or n=6 HC volunteers. All results are mean ± SEM with significance was set at *p ≤ 0.05, **p≤ 0.01, ****p≤ 0.0001, ns=not significant.