Fig. 1.
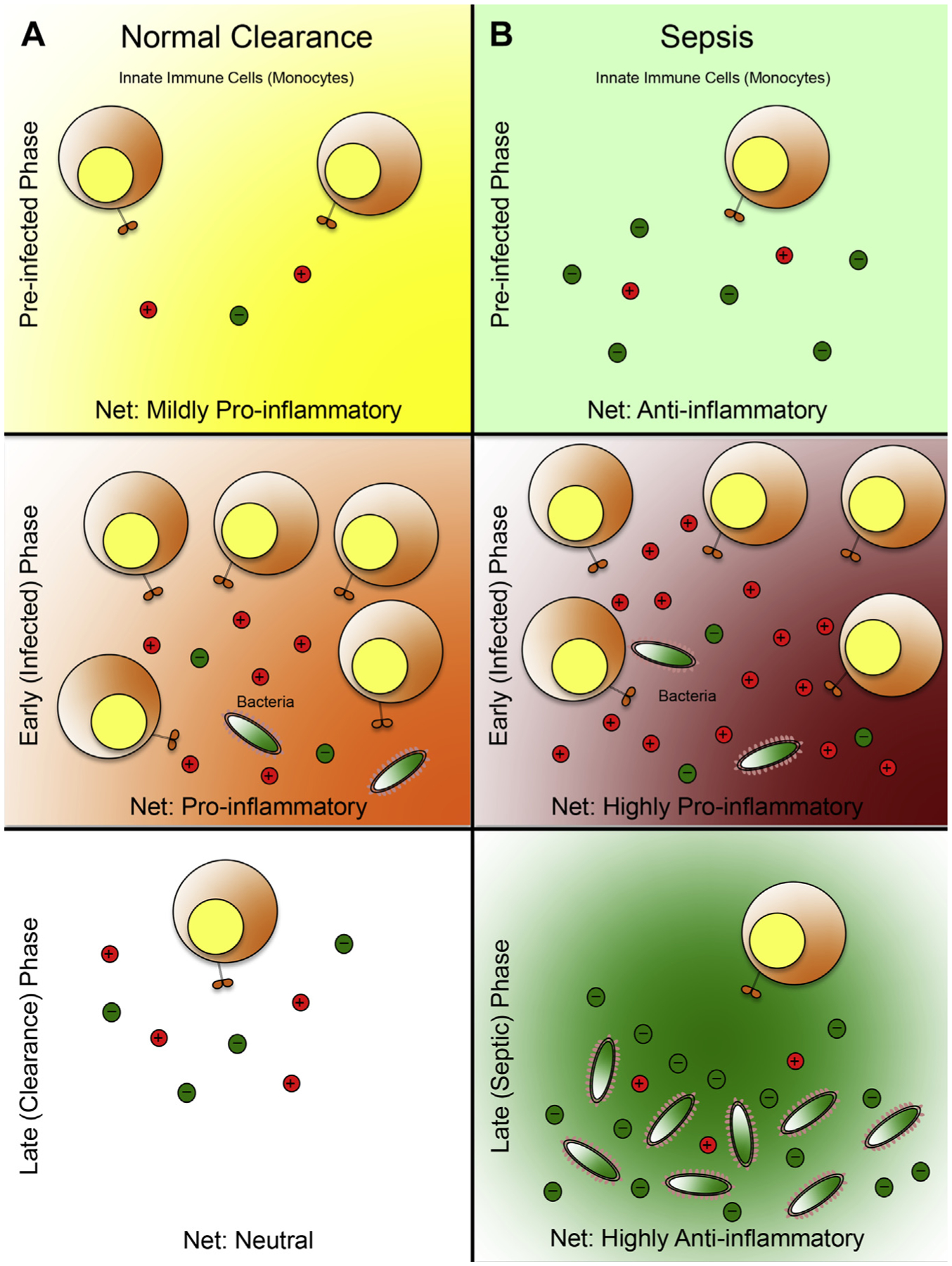
Systemic immunologic profile as a predictor of sepsis: a working model. (A) Microbial clearance of a patient who experiences opportunistic infection. In the preinfected phase, the patient blood microenvironment is in a mild proinflammatory state resulting from the mounted immune response against danger-associated molecular patterns (DAMP) molecules (generated in the process of the trauma or burn). This low-grade proinflammatory state primes the patient’s immune system to sense external insults, thus facilitating efficient detection of microbial infiltration. During the early, or infected phase, the invading bacteria are detected by the circulating leukocytes that were recruited to combat the original insult (trauma, burn). This detection results in a heightened proinflammatory response, which leads to additional proinflammatory cytokine production and recruitment of leukocytes, ultimately leading to bacterial eradication. In the late or clearance phase the invading microbes are eliminated, and the immune system is restored to a neutral state by a balance of proinflammatory and anti-inflammatory signals. (B) Sepsis development in an infected patient. In the preinfected phase, the net anti-inflammatory state of the blood microenvironment is defined by low-grade proinflammatory response mounted against the DAMP molecules, and an abundance of anti-inflammatory cytokines, produced possibly by the liver (the trigger for this response remains elusive). During the early/infected phase, a proinflammatory response is mounted against the invading microbes by the recruited leukocytes. However, because the blood microenvironment before the infected phase was anti-inflammatory, these recruited leukocytes must produce aberrantly higher levels of proinflammatory cytokines to achieve a net proinflammatory state to offset the effects of the preexisting anti-inflammatory soluble factors. As a result, these leukocytes will likely overexert their effector function and rapidly deplete their effector function potential, leading to immune exhaustion. This state is reminiscent of the systemic immune response syndrome (SIRS), or the classic cytokine storm that is observed in the acute phases of sepsis. Importantly this strong, yet relatively brief proinflammatory state does not lead to sterile immunity, which would lead to bacterial evasion from the host’s immune surveillance. In the late/sepsis phase, the immune system is exhausted and is therefore unable to produce additional proinflammatory mediators, despite having the residual bacteria from the infected phase. Furthermore, to counter the spike of proinflammatory signals in the infected phase, a massive surge in anti-inflammatory response is produced, resulting in a net anti-inflammatory microenvironment, similar to the compensatory anti-inflammatory response syndrome, which is conducive to bacterial growth, dissemination, and, ultimately, sepsis. Spheres with plus symbols denote proinflammatory mediators; spheres with minus symbols denote anti-inflammatory mediators. The immunologic state of each phase is determined by the ratio of proinflammatory mediators relative to anti-inflammatory mediators (mildly proinflammatory, 2:1; proinflammatory, 3:1; neutral, 1:1; anti-inflammatory, 1:3; highly proinflammatory, 5:1; highly anti-inflammatory, 1:5).
