Abstract
Liver transplantation is the current standard of care for end-stage liver disease and an accepted therapeutic option for acute liver failure and primary liver tumors. Despite the remarkable advances in the surgical techniques and immunosuppressive therapy, the postoperative morbidity and mortality still remain high and the leading causes are biliary complications, which affect up to one quarter of recipients. The most common biliary complications are anastomotic and non-anastomotic biliary strictures, leaks, bile duct stones, sludge and casts. Despite the absence of a recommended treatment algorithm many options are available, such as surgery, percutaneous techniques and interventional endoscopy. In the last few years, endoscopic techniques have widely replaced the more aggressive percutaneous and surgical approaches. Endoscopic retrograde cholangiography is the preferred technique when duct-to-duct anastomosis has been performed. Recently, new devices and techniques have been developed and this has led to a remarkable increase in the success rate of minimally invasive procedures. Understanding the mechanisms of biliary complications helps in their early recognition which is the prerequisite for successful treatment. Aggressive endoscopic therapy is essential for the reduction of morbidity and mortality in these cases. This article focuses on the common post-transplant biliary complications and the available interventional treatment modalities.
Keywords: Post-transplant biliary complications, Endoscopic retrograde cholangiopancreatography, Cholangioscopy, Percutaneous biliary interventions, Liver transplantation, Living-donor liver transplantation
Core Tip: Liver transplantation is the current standard of care for end-stage liver disease. Biliary complications are the leading cause of morbidity and mortality among recipients and despite the advances in surgical techniques they are seen in up to 25% of cases. Surgery, interventional endoscopy and percutaneous approaches are the available therapeutic options. Endoscopic retrograde cholangiography when possible is the most recommended therapeutic modality, replacing more aggressive surgical interventions. New techniques such as cholangioscopy overcome many of the limitations of conventional endoscopy. This article discusses the most common post-transplant biliary complications and the advances in treatment modalities.
INTRODUCTION
Liver transplantation (LT) is the widely endorsed method for treatment of end- stage liver disease, acute liver failure and primary liver cancer. The advances in surgical techniques, postoperative care, immunosuppression, and antiviral therapy have led to remarkable progress in survival of these patients. The currently reported 5-year survival rate is 70%-75%[1,2].
Biliary complications are a significant source of morbidity in the early and long-term period after LT (Table 1). Their overall incidence ranges between 15% and 25%. With associated mortality of 10%, they remain a major problem in post-transplant patients. Timely identification and treatment play a significant role in preserving the graft and improving the overall survival rate of patients[3,4].
Table 1.
Risk factors for the most common biliary complications
|
|
Anastomotic
|
Non-anastomotic
|
| Strictures | Advanced recipient age; Female donor; Failure to flush the donor duct; Preceding bile leakage; Acute rejection; Chronic rejection; Hepaticojejunostomy reconstruction | HAT; Chronic ductopenic rejection; Blood type ABO incompatibility; PSC, autoimmune hepatitis prolonged warm and cold ischemia times prolonged donor exposure to vasopressors |
| Leaks | Active bleeding at the bile duct end excessive dissection of periductal tissue tension on ductal anastomosis | T-tube tract, excessive use of electrocautery incorrect suture of the cystic duct stump |
| Stones and clots | Ischemia, stricture, infection | |
| Biliary cast syndrome | Acute cellular rejection, bile stasis, ischemia, infection, sepsis, HAT | |
| Haemobilia | Alcoholic liver disease, high body mass index of recipient; Iatrogenic: PTC, liver biopsy | |
PSC: Primary sclerosing cholangitis; PTC: Percutaneous; HAT: Hepatic artery thrombosis.
The most common current treatment is focused on interventional endoscopic (ERC) and percutaneous (PTC) procedures[4-6].
ERC provides minimal invasion with great long-term results and is a preferred method when surgical reconstruction allows this. ERC has been proven to be safe and highly effective in dealing with most of the early as well as late post-LT biliary complications. Procedural-related adverse events in post-LT cases are comparable with those among the general population[6].
The complication rate in patients after living donor liver transplantation (LDLT) in particular is about 10%, which is 2-fold higher than the standard[7,8].
PTC is an effective alternative in patients with altered anatomy which impedes endoscopy access. There is growing evidence that cholangioscopy could be a beneficial tool in the diagnostics and therapy of selected cases[9].
Surgery is available for cases when endoscopic and PCT methods have failed.
Biliary reconstruction techniques
The two major options for biliary reconstruction are bilio-enteric (hepatico-jejunostomy or choledocho-jejunostomy) and duct-to-duct anastomosis. Duct-to-duct anastomosis is the method of choice for biliary reconstruction in any type of transplantation: Cadaveric liver transplantation (DDLT), split transplantations, LDLT (left lobe or right lobe) transplantations[10,11].
Hepatico-jejunostomy is currently used only for selected cases such as those with primary sclerosing cholangitis, prior bilio-digestive surgery, significant ductal size mismatch, and insufficient length of recipient bile ducts[12].
Many benefits motivate the preference for direct duct-to-duct suturing: Preserved sphincter-of-Oddi function, lower risk of cholangitis, and reduction in the number of anastomoses. Besides, the preserved intestinal continuity ensures an endoscopic access to the biliary tree in case of potential complications[13,14].
T-tube placement has been widely abandoned over the last decades[15]. It has been proven that its usage increases the rate of biliary complications. A single-center retrospective review of 1041 transplantations reported that cholestatic liver disease, Roux-en-Y anastomosis, donor risk index > 2, and T-tubes were independent predictors of post-LT complications[16].
LDLT and DDLT
The rising number of LTs augments the need for liver grafts. This has led to the widespread tendency of LDLT. Multiple factors related to LDLT techniques contribute to the increased incidence of biliary complications[11].
Hepatic resection of the donor liver in LDLT requires dissection of the hilum, which could cause bile duct devascularization or subsequent bile leak from the cut surface of the liver. Excessive use of coagulation diathermy is another risk factor for the occurrence of bile leak. On the other hand, the need for dissection of the recipient’s left or right hepatic duct could prolong the ischemic time. Bringing the recipient’s hepatic duct to the graft’s hilum to ensure tension-free anastomosis could cause additional disturbance of the blood supply. In general, the reported biliary complication rate is 2-3-fold higher in LTLD than in DDLT. Furthermore, the treatment is usually more complicated due to the smaller size of the ducts or the presence of multiple anastomoses. Therefore, the success rate of treatment for complications is lower in LDLT[14,17-19].
Classification
The most common complications are strictures, leaks, and biliary stones. According to the timeframe of their occurrence, post-LT complications can be divided into early (occurring within the first 4 wk after transplantation) and late. Biliary leaks are the most common complication in the early postoperative period, while biliary strictures are the predominant complication as a whole. According to the lesion location, strictures and leaks are divided into anastomotic and non-anastomotic[20-22].
It is appropriate to make a distinction between biliary stricture and biliary obstruction. While the obstruction can be caused by external compression (biloma, haematoma), luminal cast, stones or tube remnants, the stricture is narrowing of the duct lumen, causing bile outflow disturbance.
Multiple factors can play a role in the occurrence of biliary complications. Anastomotic lesions are mostly due to technical issues, while non-anastomotic lesions are the result of ischemia or immune reactions[23].
With respect to the etiology, some authors divide the complications into five groups[21]: (1) Hepatic artery thrombosis-related; (2) Technical biliary complications; (3) Ischemic-type biliary lesions; (4) Infectious biliary complications; and (5) Uncommon: Sphincter of Oddi dysfunction (SOD), bile cast syndrome, haemobilia, lymphoproliferative disease, and other neoplasms.
Biliary strictures
Up to 50% of post-LT biliary complications consist of biliary strictures[24]. They are divided into two major morphological types: Anastomotic (AS) and non-anastomotic (NAS).
Most frequently, the strictures are anastomotic. AS appear more often in LDLT than in DDLT. They are short, single narrowings, located at the anastomotic site. The incidence ranges between 5%-15% in DDLT and 13%-36% in LDLT[21-26]. They occur mostly during the first year after transplantation within a mean time of 5-8 wk[23,27].
The most common factors associated with AS are surgical issues over the first months and ischemia leading to fibrous healing at the later stages. Additionally, ABO incompatibility, advanced recipient age, small bile duct caliber, prolonged warm and cold ischemia time, and cytomegalovirus infection are reported to be significant risk factors[25,28-30].
Endoscopic retrograde cholangiography (ERCP) is the standard of care for AS treatment, whenever anatomy allows it. The overall reported success rate ranges between 70%-100%[31-33].
For patients with hepatico-jejunostomy, different scopes such as single or double balloon enteroscope, spiral enteroscope or pediatric colonoscope are used. These techniques are time-consuming and complex; they require additional expertise and are related to higher risk and higher cost[32,34-37].
For all these reasons, PTC is a widely accepted approach in cases of altered anatomy[38]. Surgical therapy is now used as salvage therapy and is required in about 1% of cases[39].
AS treatment aims to normalize bile outflow through the anastomosis. The endpoint of ERC is lack of narrowing during occlusive cholangiography or free contrast outflow during fluoroscopy (Figure 1). Clinical and laboratory resolution of cholestasis are the most reliable measures of successful treatment.
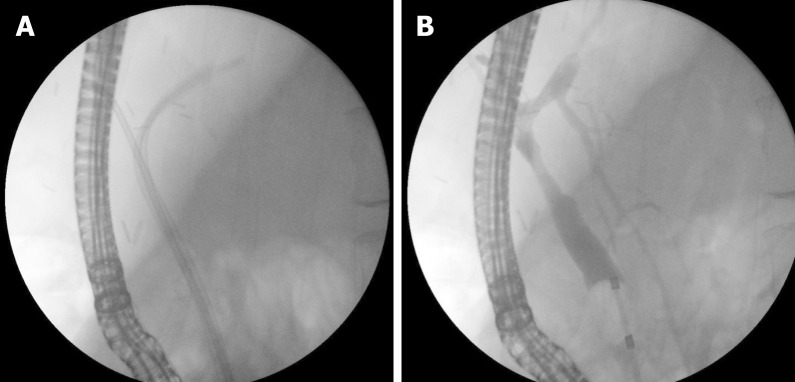
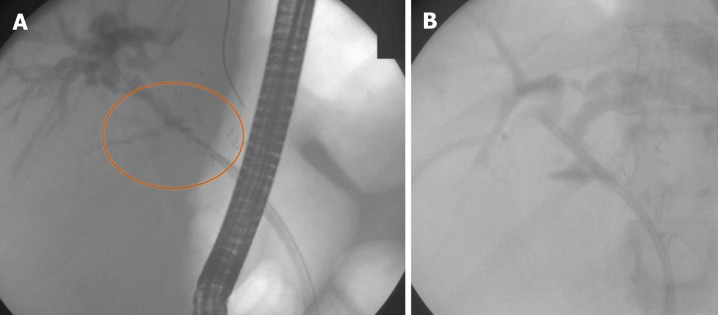
Figure 1.
Endoscopic treatment of anastomotic stricture after living donor liver transplantation. A: Two plastic stents; and B: Occlusive cholangiogram after treatment.
The standard treatment includes guidewire insertion across the stricture, followed by balloon dilation and stent insertion. Most commonly 10Fr or 7Fr plastic stents are used. These stents can be easily removed or replaced. Balloon dilation in itself is effective as a non-invasive technique, which has shown less than promising long-term results with a 30%-40% success rate[34,40] (Figure 2).
Figure 2.
Anastomotic stricture. A: Cholangiogram; B: Balloon dilation; and C: Multiple stent treatment.
Numerous large studies have proven that the combination of balloon dilation plus stent placement is more effective than dilation or stenting alone[41].
Several endoscopic strategies are applied in the management of anastomotic strictures. The most frequently used technique is balloon dilation with placement of a maximum number of 10Fr plastic stents with subsequent stent exchange until full resolution of the stricture on fluoroscopy (Table 2).
Table 2.
Studies on the effectiveness of maximal stent therapy in post-operative biliary strictures
|
Ref.
|
Patients
|
Treatment duration
|
Mean number of stents
|
Number of ERCPs
|
Success rate
|
| Costamagna et al[41], 2001 | 45 | 12.1 mo (range 2-24 mo) | 3.2 (range 1-6) | 4.1 (range 2-8) | 89% (40/45) |
| Hsieh et at[23], 2012 | 41 | 5.3 (range 3.8-8.9) | 7.0 (range 4-10) | 4.0 (range 3.0-5.3) | 100% (41/41) |
| Morelli et al[43], 2008 | 38 | 107 d (range 20-198 d) | 2.5 (range 1-6) | 3.4 (range 2-6) | 87% (33/38) |
| Pasha et al[90], 2004 | 25 | 3.3 mo (range, 2.2-7 mo) | 2.0 (range 1-4) | 3.5 (range 1-9) | 88% (22 of 25) |
| Tabibian et al[42], 2010 | 69 | 15 mo (range 12-60 mo) | 3.0 (range 2-7) | 2.5 (range 2-5) | 94% (65/69) |
ERCP: Endoscopic retrograde cholangiography.
The initial dilation requires 4-10 mm balloons. In rare cases of tight strictures a Soehendra catheter can be used to overcome the stricture. The progressive increase in the number of stents with every subsequent procedure has ensured more sustained resolution of the stricture[42,43].
Different time intervals between stent exchanges were investigated. In a study from 2008, a short-term stent exchange of every 2 wk was investigated. The reported resolution rate was 87%, achieved for a mean period of 107 d and a mean number of stents inserted of 2.5. More often stents are replaced every three months to prevent occlusion and cholangitis. The reported success rate in many large studies is 80%-95%[39,41-43]. In a review of 440 post-LT patients with AS, the success rate of stent therapy was 84%. The resolution rate was established to be dependent on therapy duration and was highest (94%-100%) when therapy lasted 12 mo or more[44].
The time it takes for the structure to evolve has also been proved to be a predictive factor for healing. Strictures manifested within the first 6 mo after LT have better prognosis for sustained resolution[25,31,45].
Due to elevated rupture risk, it is preferable for ERC to be postponed at least one month after the transplantation. When necessary, a 7-8.5 Fr stent is applied without balloon dilation. In tight strictures, a 4 mm angioplasty balloon may be considered[46].
Some new dilation balloons have been tested in order to improve bile stricture resolution. There are few published data on the usage of peripheral cutting balloons[47].
Paclitaxel-eluting balloons have been investigated, due to the fact that paclitaxel can suppress fibrotic proliferation[48]. The latter two are not in common use.
An available alternative to the standard multiple-plastic-stent therapy is the placement of fully covered self-expanding metal stents (fSEMS). Their major benefits are a reduction in the number of procedures and cost-effectiveness[49-52].
In a substantive study with 200 cases, the reported success was 80%-95%[51]. Eight and 10 mm SEMS are available according to the stricture size. FSEMS are not considered suitable for AS smaller than 5 mm[24].
Stent migration is the major limitation of this technique. The main strategies to prevent migration include skipping dilation of the stricture, using stents with flaps, and leaving the stent in the duodenum for a long period[49-51].
A large systematic review, published in 2013, reported a migration rate of fSEMS of 16%; the authors also mentioned a low risk of stent ingrowth and stent impaction. The comparison analysis in that study showed that neither technique was superior[49,53].
Management in LDLT is more challenging due to the frequent presence of multiple anastomoses with a smaller size (Figure 3). According to Coté et al[24], significant risk factors for treatment failure in LDLT are higher LT recipient age, longer operation duration, and a pouched morphology of the AS.
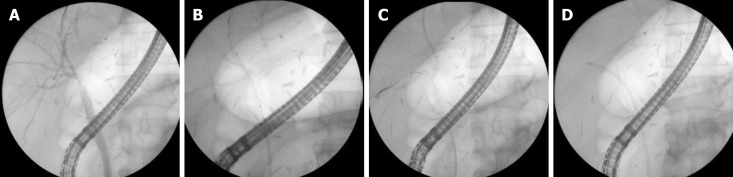
Figure 3.
Anastomotic stricture after living donor liver transplantation (right lobe). A: Guidewire insertion; B: Balloon dilation; C: Second guidewire insertion; and D: Stent placement (7Fr + 5Fr).
Non-anastomotic strictures consist of one or more duct narrowings proximal to the anastomosis. They are longer, complex, and usually multiple, and can affect intra- and extrahepatic ducts. NAS are more rarely observed: 5%-10% of biliary complications[54]. Ischemia and immunological reactions are the main aetiological mechanisms. The most common risk factors reported in the literature are hepatic artery thrombosis, prolonged cold and warm ischemia, prolonged exposure to vasopressors of the donor, ABO incompatibility, chronic ductopenic rejection, PSC or autoimmune hepatitis in the recipient[55,56]. In the case of acute hepatic artery thrombosis, early revascularization therapy is required to prevent multiple stricture formation.
Cases with NAS could benefit from mini-invasive (endoscopic and percutaneous) treatment, but the estimated results are significantly worse than in cases with AS. In cases with dominant strictures and extrahepatic localization ERC is the first treatment option. Endoscopic access to NAS is much more challenging due to the small caliber and relatively proximal location[53]. Cases with angulated, complex strictures, not suitable for ERC passage benefit from percutaneous approaches, followed by hybrid procedures such as the rendezvous technique. When intrahepatic strictures are present, PTC with direct radiology-guided percutaneous stent insertion could be in order[57,58].
Stricture recurrence and continued stricture formation are possible even after successful endoscopic therapy. Long-term observation (MRCP and laboratory) of these patients is required to evaluate the disease course and the response to treatment. Cases resistant to stent treatment, or those with diffuse bile duct injury, must be listed for re-transplantation. Percutaneous drainage could be a bridging therapy to the operation[54,58].
The reported success rate of stenting therapy in the literature is 50% to 75% for DDLT and 33%-50% for LDLT[26,50]. In most NAS cases, the treatment process also takes longer than with AS[11,59]. Passing a guidewire through the stricture is considered the most critical moment. Occlusion balloons and swing-tip catheters for selective cannulation are used for this purpose[54]. The rendezvous technique could also be used to deal with this issue[59,60].
After successful cannulation, the standard technique of balloon dilation followed by plastic stent insertion is performed. For this type of stricture, 4-6 mm balloons with a subsequent increase in caliber are used. Even when cannulated, the width, angulation and proximal location of the strictures often limit the stent insertion. The stents used are usually 7 or 8.5Fr and carry a high migration risk due to rigidity of the plastic[58,59].
A working group from Minnesota reported their treatment for NAS with long (12-20 cm), 10Fr flexible stents with side fenestration. They provide better bile drainage through the stent and through the side holes and could be inserted higher due to their flexibility[61].
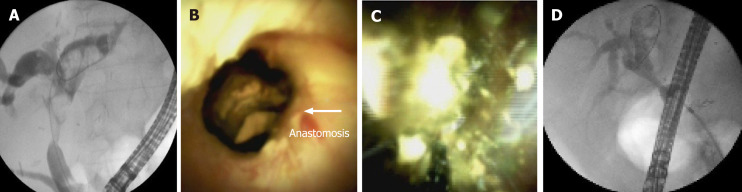
Cholangioscopy provides direct visualisation of the biliary tree. This allows visual assessment of the biliary epithelium at the stricture and tissue sampling if needed. In cases of strictures, not suitable for standard cannulation, cholangioscopy enables guidewire insertion under visual control (Figure 4). This facilitates guidewire placement in tight, angulated strictures. Cholangioscopy has been proven to increase the stricture cannulation rate and the success rate of endoscopy treatment as a whole (Figure 5). The implementation of cholangioscopy in stricture therapy could spare the need for percutaneous drainage and surgical interventions[62,63].
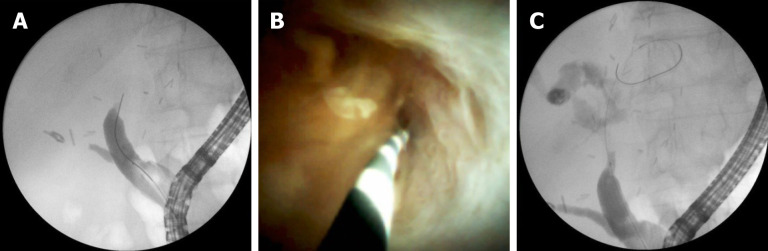
Figure 4.
Complex anastomotic stricture. A: Impossible insertion of guidewire through a stricture; B: Guidewire insertion under direct visual control; and C: Guidewire inserted above anastomosis.
Figure 5.
Digital cholangioscopy image of an anastomotic stricture.
Bile leaks
Bile leaks are the second most frequent biliary complication after LT. Bile leaks are also divided into anastomotic and non-anastomotic. Most of them are anastomotic and occur early - within the first 4 wk after LT[8,10,64].
The reported incidence in the literature ranges from 2% to 25%[13,22].
Their occurrence is slightly higher in patients with bilio-enteric reconstruction than with cases of duct-to-duct anastomosis. A systematic review, including data from 61 studies, reported the incidence of bile leaks to be 9.5% in LDLT and 7.8% in DDLT[64]. The presence of a bile leak is an independent risk factor for further development of a stricture[65].
Early bile leaks are usually caused by technical issues related to surgery, such as tension of the anastomosis, incomplete cystic stump suture, excessive use of diathermy, bleeding from the cut ends of ducts, premature T-tube extraction, and the cut surface of the graft. Ischemic injury is the other major cause of bile leaks[8,18,19,52]. Large studies have shown double and triple hepatico-jejunostomy and warm ischemia time as independent risk factors for the occurrence of bile leaks[17,18].
Bile diversion is the key to bile leak healing. Therapeutic options include ERC followed by stenting or nasobiliary drainage, percutaneous drainage, and surgical revision. Sphincterotomy with endoscopic stenting leads to reduction in the transpapillary pressure, usually followed by fast lesion closure. Stent placement leads to successful treatment in over 90% of cases with early leaks (Figure 6)[13,66]. Simple defects like T-tube exit, cystic duct remnant or small anastomotic leaks usually close in 2-5 wk. The biliary stent is usually extracted after no less than 3 mo due to potentially delayed tissue healing on account of immunosuppression. Some centers prefer the placement of nasobiliary drainage for early small defects. This allows close fluoroscopic follow-up of the defect closure and avoids the need for a second stent extraction procedure. Given the low patient tolerance, displacement risk, and prolonged hospital stay, this practice is currently of limited use[19,66].
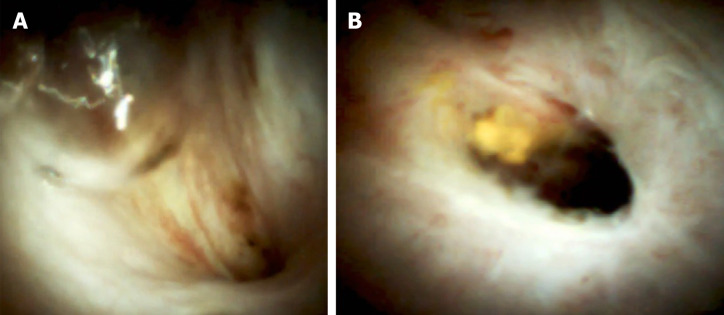
Figure 6.
Anastomotic leak. A: Guidewire insertion; and B: Stent placement (10Fr).
In cases with defects, refractory to plastic stent treatment, fcSEMS usage could be considered. Small studies have reported good closure success rate[67-69].
According to a study including 35 cases treated with 8 mm and 10 mm fcSEMS, the achieved leak resolution was 94%[68].
In some studies, a high incidence of stricture was observed after stent removal[70].
In cases with bilio-enteric anastomosis, percutaneous access to the biliary tree is used for bile diversion. An internal-external drainage placement for 3-6 mo is an effective alternative to the endoscopic approach. A technique with EUS-guided gastrostomy, used for ERCP access, is also reported in a small study from 2011[33].
In cases with a T-tube, drainage unclamping is sufficient. When bile juice is diverted outside the body (nasobiliary, percutaneous, T-tube drainage), the level of immunosuppression medication, in particular cyclosporine, should be closely monitored. If a significant collection is formed, the latter must be drained to prevent infection, sepsis, and late adhesion. Large or complex leaks often require surgical revision due to a high probability of intra-abdominal abscess formation[54,55].
Bile stones and sludge
Formation of sludge, clots, casts and stones can cause bile obstruction. The reported incidence after LT ranges widely between 4%-10%[71,72].
Cyclosporine therapy, mucosal damage due to ischemia or infection and cholesterol supersaturation (often seen post-LT) could predispose to lithogenesis. In many cases, there is an underlying stricture. Usually, an ERC and sludge/stone extraction procedure is sufficient for definitive treatment with a success rate over 90%[72-76].
According to Alazmi et al[45], there is a 17% incidence rate of recurrence within the first 6 mo after the procedure.
Well-known techniques, such as large balloon dilation and mechanical lithotripsy, are used in cases of large stones. In cases of difficult lithiasis such as multiple, large or intrahepatic stones, as well as stones over the stricture, extracorporeal lithotripsy could be applied. A study in 2015 reported six cases of difficult lithiasis that could not be treated with standard ERCP. Five of the six cases were managed with ECSL with no reported adverse events[77].
The limitations of endoscopic therapy can be overcome by means of digital cholangioscopy. Cholangioscopy provides an opportunity for visually controlled fragmentation of large biliary stones with little risk of biliary injury. Advanced intraductal techniques such as Holmium laser or Electrohydraulic lithotripsy achieve outstanding results in difficult cases, not suitable for ERC treatment (Figure 7)[62,78,79].
Figure 7.
Multiple intrahepatic stones above anastomotic stricture. A: Fluoroscopic image; B: Digital cholangioscopic image; C: Electrohydraulic lithotripsy performance; and D: Fluoroscopic image after treatment.
A research team from South Korea (Nam et al[79]) reported a case series of 15 patients (intrahepatic lithiasis n = 10, biliary cast syndrome n = 3, stones over the stricture n = 2) treated with percutaneous intrahepatic cholangioscopy. Eleven patients were successfully managed and no procedure-related adverse events were observed[79].
Biliary cast syndrome
This disorder represents multiple filling defects in intra- and extrahepatic bile ducts, caused by casts adherent to the biliary epithelium. The reported incidence varies between 2.5% and 18%[80,81].
The pathogenetic mechanism is considered to be cell injury as a result of ischemia, acute cellular rejection, chronic rejection, infection, or bile stasis. The desquamated epithelial cells combined with bile components may form hard casts[82].
ERC with bile tree flushing and cast extraction will suffice in many cases. Balloon extractors and Dormia baskets are used for this purpose[81]. In cases of extended intrahepatic involvement or altered anatomy, a percutaneous procedure could be needed. In a study of 10 patients with biliary cast syndrome, mini-invasive (endoscopic/percutaneous) treatment was successful in 60% of cases[83].
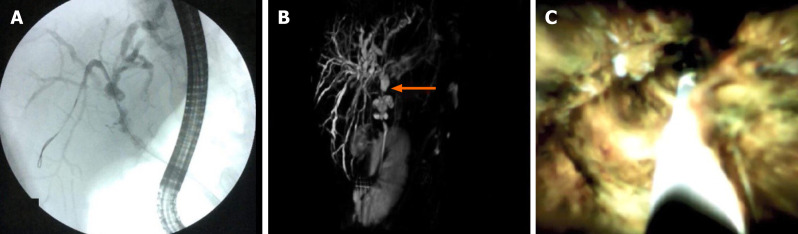
Several studies noted good outcomes following cholangioscopy-guided therapy of bile cast syndrome (Figure 8). Nam et al[79] reported three cases, treated by percutaneous cholangioscopy.
Figure 8.
Biliary cast syndrome. A: Fluoroscopic image; B: Magnetic resonance cholangiopancreatography; and C: Digital cholangioscopic image.
Ursodeoxycholic acid is considered to have a role in the prophylaxis of bile cast syndrome. In cases refractory to mini-invasive therapy, surgery is required.
Sphincter of Oddi dysfunction
Chronic injury, denervation of the recipient’s common bile duct (CBD), or fibrotic tissue formation could cause impaired ampullary relaxation and hypertension of the papilla of Vater. The role of biliary manometry in the diagnosis of SOD after transplantation is uncertain. Sphincterotomy is usually sufficient to resolve the obstruction[27,29]. In cases of firm fibrosis, stent placement could be in order[8,21].
Mucocele
In rare cases, the donor’s cystic duct could be incorporated in the suture line of the anastomosis. As a consequence, a blind mucosa-lined sac is formed. Due to accumulation of mucin, this sac can increase in size and cause bile obstruction due to external compression. Endoscopy could not provide sustainable resolution in such cases. Percutaneous drainage or surgical resection are effective treatment options. The differential diagnosis of mucocele is made with any type of fluid collection such as biloma, abscess, hemorrhage, and aneurysm[8,84,85].
Redundant CBD
The excessive length of the donor’s common hepatic duct could lead to a sigmoid-shaped deflection of the CBD. This could entail bile outflow deterioration. The reported incidence is 1.6% in all LT. ERC with long plastic stent placement usually resolves cholestasis. In very rare cases, surgery with a new biliodigestive anastomosis is needed[86].
Haemobilia
Spontaneous haemorrhage in the biliary tree after LT occurs rarely with a reported frequency of 1.2%. There are reported cases of haemobilia associated with large biliary stones over the stricture. More often, haemobilia is iatrogenic, i.e. subsequent to percutaneous biliary drainage or liver biopsy. Rupture of a hepatic artery pseudoaneurysm can cause severe biliary haemorrhage. Recipient high BMI and alcoholic liver disease were significant risk factors for spontaneous haemobilia reported in a study including 2701 post-LT patients[87].
ERC with clot extraction and nasobiliary drainage placement is the first-choice therapy. Nasobiliary drainage ensures an opportunity for biliary lavage, which prevents the development of cholangitis and indicates the presence of recurrent bleeding. In most cases, the combination of endoscopic desobstruction therapy, coagulation correction, and supportive medication yields good results. In cases of severe haemorrhage, selective embolization techniques are reported to be successful. Plastic biliary stents or fSEMS were reported to be effective haemostatic tools in studies of non-transplant patients with significant haemobilia[88-90].
Due to low incidence, there are not enough data regarding post-transplant patients with severe haemobilia.
Foreign bodies
Suture materials or T-tube remnants could form a nidus for bile sediment and stones. ERC and PTC are effective methods for detection and clearance of bile duct remnants[59].
CONCLUSION
Known as the Achilles' heel of liver transplantation, biliary complications are observed in one quarter of all patients. Their prevalence has increased due to the worldwide increase in liver transplantation. Living donor liver transplantations have a higher complication rate and presuppose more complicated treatment scenarios with lower success rates. Endoscopic stent insertion is the key treatment for most biliary complications. Percutaneous or EUS-guided puncture and cholangioscopy are feasible options for biliary access when standard fluoroscopic cannulation fails. A wide variety of accessories have been developed to overcome the complexity of living donor liver transplantation complications, but the treatment success rate remains unsatisfactory. Early recognition and aggressive management are essential for the reduction of morbidity and mortality in patients with biliary complications.
Footnotes
Conflict-of-interest statement: Petko Karagyozov has received fees for proctoring SpyGlass DS procedures from Boston Scientific Corp.
Manuscript source: Invited manuscript
Peer-review started: June 14, 2020
First decision: October 21, 2020
Article in press: December 2, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Bulgaria
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Boteon YL, Lin J, Ozdemir F S-Editor: Zhang L L-Editor: Webster JR P-Editor: Zhang YL
Contributor Information
Irina Boeva, Department of Interventional Gastroenterology, Acibadem City Clinic Tokuda Hospital, Sofia 1407, Bulgaria.
Petko Ivanov Karagyozov, Department of Interventional Gastroenterology, Clinic of Gastroenterology, Acibadem City Clinic Tokuda Hospital, Sofia 1407, Bulgaria. petko.karagyozov@gmail.com.
Ivan Tishkov, Department of Interventional Gastroenterology, Acibadem City Clinic Tokuda Hospital, Sofia 1407, Bulgaria.
References
- 1.Yoshida EM, Haque M, Scudamore CH. Adult live donor liver transplantation: routine, commonplace, standard care for end stage liver disease (we hope) Ann Hepatol. 2010;9:89–90. [PubMed] [Google Scholar]
- 2.Charlton MR. Roadmap for improving patient and graft survival in the next 10 years. Liver Transpl. 2016;22:71–78. doi: 10.1002/lt.24602. [DOI] [PubMed] [Google Scholar]
- 3.Girotra M, Soota K, Klair JS, Dang SM, Aduli F. Endoscopic management of post-liver transplant biliary complications. World J Gastrointest Endosc. 2015;7:446–459. doi: 10.4253/wjge.v7.i5.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moy BT, Birk JW. A Review on the Management of Biliary Complications after Orthotopic Liver Transplantation. J Clin Transl Hepatol. 2019;7:61–71. doi: 10.14218/JCTH.2018.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel P, DiNorcia J. The devil is in the detail: current management of perioperative surgical complications after liver transplantation. Curr Opin Organ Transplant. 2019;24:138–147. doi: 10.1097/MOT.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 6.Stratta RJ, Wood RP, Langnas AN, Hollins RR, Bruder KJ, Donovan JP, Burnett DA, Lieberman RP, Lund GB, Pillen TJ. Diagnosis and treatment of biliary tract complications after orthotopic liver transplantation. Surgery. 1989;106:675–683; discussion 683-684. [PubMed] [Google Scholar]
- 7.Balderramo D, Bordas JM, Sendino O, Abraldes JG, Navasa M, Llach J, Cardenas A. Complications after ERCP in liver transplant recipients. Gastrointest Endosc. 2011;74:285–294. doi: 10.1016/j.gie.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857–863. doi: 10.1055/s-2005-870192. [DOI] [PubMed] [Google Scholar]
- 9.Elmunzer BJ, Debenedet AT, Volk ML, Sonnenday CJ, Waljee AK, Fontana RJ, Oza AB, Singal A, Englesbe MJ, Scheiman JM. Clinical yield of diagnostic endoscopic retrograde cholangiopancreatography in orthotopic liver transplant recipients with suspected biliary complications. Liver Transpl. 2012;18:1479–1484. doi: 10.1002/lt.23535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greif F, Bronsther OL, Van Thiel DH, Casavilla A, Iwatsuki S, Tzakis A, Todo S, Fung JJ, Starzl TE. The incidence, timing, and management of biliary tract complications after orthotopic liver transplantation. Ann Surg. 1994;219:40–45. doi: 10.1097/00000658-199401000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graziadei IW, Schwaighofer H, Koch R, Nachbaur K, Koenigsrainer A, Margreiter R, Vogel W. Long-term outcome of endoscopic treatment of biliary strictures after liver transplantation. Liver Transpl. 2006;12:718–725. doi: 10.1002/lt.20644. [DOI] [PubMed] [Google Scholar]
- 12.Graziadei IW. Recurrence of primary sclerosing cholangitis after liver transplantation. Liver Transpl. 2002;8:575–581. doi: 10.1053/jlts.2002.33952. [DOI] [PubMed] [Google Scholar]
- 13.Akamatsu N, Sugawara Y, Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 2011;24:379–392. doi: 10.1111/j.1432-2277.2010.01202.x. [DOI] [PubMed] [Google Scholar]
- 14.Welling TH, Heidt DG, Englesbe MJ, Magee JC, Sung RS, Campbell DA, Punch JD, Pelletier SJ. Biliary complications following liver transplantation in the model for end-stage liver disease era: effect of donor, recipient, and technical factors. Liver Transpl. 2008;14:73–80. doi: 10.1002/lt.21354. [DOI] [PubMed] [Google Scholar]
- 15.Rizk RS, McVicar JP, Emond MJ, Rohrmann CA Jr, Kowdley KV, Perkins J, Carithers RL Jr, Kimmey MB. Endoscopic management of biliary strictures in liver transplant recipients: effect on patient and graft survival. Gastrointest Endosc. 1998;47:128–135. doi: 10.1016/s0016-5107(98)70344-x. [DOI] [PubMed] [Google Scholar]
- 16.Senter-Zapata M, Khan AS, Subramanian T, Vachharajani N, Dageforde LA, Wellen JR, Shenoy S, Majella Doyle MB, Chapman WC. Patient and Graft Survival: Biliary Complications after Liver Transplantation. J Am Coll Surg. 2018;226:484–494. doi: 10.1016/j.jamcollsurg.2017.12.039. [DOI] [PubMed] [Google Scholar]
- 17.Kasahara M, Egawa H, Takada Y, Oike F, Sakamoto S, Kiuchi T, Yazumi S, Shibata T, Tanaka K. Biliary reconstruction in right lobe living-donor liver transplantation: Comparison of different techniques in 321 recipients. Ann Surg. 2006;243:559–566. doi: 10.1097/01.sla.0000206419.65678.2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnston TD, Gates R, Reddy KS, Nickl NJ, Ranjan D. Nonoperative management of bile leaks following liver transplantation. Clin Transplant. 2000;14:365–369. doi: 10.1034/j.1399-0012.2000.14040102.x. [DOI] [PubMed] [Google Scholar]
- 19.Oh DW, Lee SK, Song TJ, Park DH, Lee SS, Seo DW, Kim MH. Endoscopic management of bile leakage after liver transplantation. Gut Liver. 2015;9:417–423. doi: 10.5009/gnl14117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El Deen FZ, Lee CS, Lee WC. Endoscopic Management of Biliary Complications after Liver Transplantation. Ther Gastrointest Endosc . 2011:93–114. [Google Scholar]
- 21.Wojcicki M, Milkiewicz P, Silva M. Biliary tract complications after liver transplantation: a review. Dig Surg. 2008;25:245–257. doi: 10.1159/000144653. [DOI] [PubMed] [Google Scholar]
- 22.Williams ED, Draganov PV. Endoscopic management of biliary strictures after liver transplantation. World J Gastroenterol. 2009;15:3725–3733. doi: 10.3748/wjg.15.3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tashiro H, Itamoto T, Sasaki T, Ohdan H, Fudaba Y, Amano H, Fukuda S, Nakahara H, Ishiyama K, Ohshita A, Kohashi T, Mitsuta H, Chayama K, Asahara T. Biliary complications after duct-to-duct biliary reconstruction in living-donor liver transplantation: causes and treatment. World J Surg. 2007;31:2222–2229. doi: 10.1007/s00268-007-9217-x. [DOI] [PubMed] [Google Scholar]
- 24.Coté GA, Slivka A, Tarnasky P, Mullady DK, Elmunzer BJ, Elta G, Fogel E, Lehman G, McHenry L, Romagnuolo J, Menon S, Siddiqui UD, Watkins J, Lynch S, Denski C, Xu H, Sherman S. Effect of Covered Metallic Stents Compared With Plastic Stents on Benign Biliary Stricture Resolution: A Randomized Clinical Trial. JAMA. 2016;315:1250–1257. doi: 10.1001/jama.2016.2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verdonk RC, Buis CI, Porte RJ, van der Jagt EJ, Limburg AJ, van den Berg AP, Slooff MJ, Peeters PM, de Jong KP, Kleibeuker JH, Haagsma EB. Anastomotic biliary strictures after liver transplantation: causes and consequences. Liver Transpl. 2006;12:726–735. doi: 10.1002/lt.20714. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh TH, Mekeel KL, Crowell MD, Nguyen CC, Das A, Aqel BA, Carey EJ, Byrne TJ, Vargas HE, Douglas DD, Mulligan DC, Harrison ME. Endoscopic treatment of anastomotic biliary strictures after living donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2013;77:47–54. doi: 10.1016/j.gie.2012.08.034. [DOI] [PubMed] [Google Scholar]
- 27.Sun N, Zhang J, Li X, Zhang C, Zhou X, Zhang C. Biliary tract reconstruction with or without T-tube in orthotopic liver transplantation: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2015;9:529–538. doi: 10.1586/17474124.2015.1002084. [DOI] [PubMed] [Google Scholar]
- 28.Shibuya ML, Buddenbaum WE, Don AL, Utsumi H, Suciu D, Kosaka T, Elkind MM. Amsacrine-induced lesions in DNA and their modulation by novobiocin and 2,4-dinitrophenol. Cancer Res. 1991;51:573–580. [PubMed] [Google Scholar]
- 29.Sawyer RG, Punch JD. Incidence and management of biliary complications after 291 liver transplants following the introduction of transcystic stenting. Transplantation. 1998;66:1201–1207. doi: 10.1097/00007890-199811150-00015. [DOI] [PubMed] [Google Scholar]
- 30.O'Connor TP, Lewis WD, Jenkins RL. Biliary tract complications after liver transplantation. Arch Surg. 1995;130:312–317. doi: 10.1001/archsurg.1995.01430030082017. [DOI] [PubMed] [Google Scholar]
- 31.Leidy K. Enjoyable learning experiences--an aid to retention? J Contin Educ Nurs. 1992;23:206–208. doi: 10.3928/0022-0124-19920901-08. [DOI] [PubMed] [Google Scholar]
- 32.Arain MA, Attam R, Freeman ML. Advances in endoscopic management of biliary tract complications after liver transplantation. Liver Transpl. 2013;19:482–498. doi: 10.1002/lt.23624. [DOI] [PubMed] [Google Scholar]
- 33.Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol. 2011;34:107–115. doi: 10.1016/j.gastrohep.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 34.Saleem A, Baron TH. Successful endoscopic treatment of biliary cast syndrome in an orthotopic liver transplant patient with a Roux-en-Y anastomosis via balloon enteroscopy. Liver Transpl. 2010;16:527–529. doi: 10.1002/lt.22007. [DOI] [PubMed] [Google Scholar]
- 35.Di Pisa M, Miraglia R, Volpes R, Gruttadauria S, Traina M. Single balloon enteroscopy for endoscopic retrograde cholangiography in a patient with hepaticojejunostomy after liver transplant. Gastroenterol Res Pract. 2010;2010:701696. doi: 10.1155/2010/701696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanada Y, Mizuta K, Yano T, Hatanaka W, Okada N, Wakiya T, Umehara M, Egami S, Urahashi T, Hishikawa S, Fujiwara T, Sakuma Y, Hyodo M, Yamamoto H, Yasuda Y, Kawarasaki H. Double-balloon enteroscopy for bilioenteric anastomotic stricture after pediatric living donor liver transplantation. Transpl Int. 2011;24:85–90. doi: 10.1111/j.1432-2277.2010.01156.x. [DOI] [PubMed] [Google Scholar]
- 37.Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608–1610. doi: 10.1002/lt.20623. [DOI] [PubMed] [Google Scholar]
- 38.Attam R, Leslie D, Freeman M, Ikramuddin S, Andrade R. EUS-assisted, fluoroscopically guided gastrostomy tube placement in patients with Roux-en-Y gastric bypass: a novel technique for access to the gastric remnant. Gastrointest Endosc. 2011;74:677–682. doi: 10.1016/j.gie.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 39.Zoepf T, Maldonado-Lopez EJ, Hilgard P, Malago M, Broelsch CE, Treichel U, Gerken G. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006;12:88–94. doi: 10.1002/lt.20548. [DOI] [PubMed] [Google Scholar]
- 40.Kim TH, Lee SK, Han JH, Park DH, Lee SS, Seo DW, Kim MH, Song GW, Ha TY, Kim KH, Hwang S, Lee SG. The role of endoscopic retrograde cholangiography for biliary stricture after adult living donor liver transplantation: technical aspect and outcome. Scand J Gastroenterol. 2011;46:188–196. doi: 10.3109/00365521.2010.522722. [DOI] [PubMed] [Google Scholar]
- 41.Holt AP, Thorburn D, Mirza D, Gunson B, Wong T, Haydon G. A prospective study of standardized nonsurgical therapy in the management of biliary anastomotic strictures complicating liver transplantation. Transplantation. 2007;84:857–863. doi: 10.1097/01.tp.0000282805.33658.ce. [DOI] [PubMed] [Google Scholar]
- 42.Costamagna G, Pandolfi M, Mutignani M, Spada C, Perri V. Long-term results of endoscopic management of postoperative bile duct strictures with increasing numbers of stents. Gastrointest Endosc. 2001;54:162–168. doi: 10.1067/mge.2001.116876. [DOI] [PubMed] [Google Scholar]
- 43.Tabibian JH, Asham EH, Han S, Saab S, Tong MJ, Goldstein L, Busuttil RW, Durazo FA. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video) Gastrointest Endosc. 2010;71:505–512. doi: 10.1016/j.gie.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 44.Morelli G, Fazel A, Judah J, Pan JJ, Forsmark C, Draganov P. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc. 2008;67:879–885. doi: 10.1016/j.gie.2007.08.046. [DOI] [PubMed] [Google Scholar]
- 45.Alazmi WM, Fogel EL, Watkins JL, McHenry L, Tector JA, Fridell J, Mosler P, Sherman S, Lehman GA. Recurrence rate of anastomotic biliary strictures in patients who have had previous successful endoscopic therapy for anastomotic narrowing after orthotopic liver transplantation. Endoscopy. 2006;38:571–574. doi: 10.1055/s-2006-925027. [DOI] [PubMed] [Google Scholar]
- 46.Freeman ML, Cass OW, Dailey J. Dilation of high-grade pancreatic and biliary ductal strictures with small-caliber angioplasty balloons. Gastrointest Endosc. 2001;54:89–92. doi: 10.1067/mge.2001.116176. [DOI] [PubMed] [Google Scholar]
- 47.Hüsing A, Reinecke H, Cicinnati VR, Beckebaum S, Wilms C, Schmidt HH, Kabar I. Paclitaxel-eluting balloon dilation of biliary anastomotic stricture after liver transplantation. World J Gastroenterol. 2015;21:977–981. doi: 10.3748/wjg.v21.i3.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hansen T, Hollemann D, Pitton MB, Heise M, Hoppe-Lotichius M, Schuchmann M, Kirkpatrick CJ, Otto G. Histological examination and evaluation of donor bile ducts received during orthotopic liver transplantation--a morphological clue to ischemic-type biliary lesion? Virchows Arch. 2012;461:41–48. doi: 10.1007/s00428-012-1245-8. [DOI] [PubMed] [Google Scholar]
- 49.Kao D, Zepeda-Gomez S, Tandon P, Bain VG. Managing the post-liver transplantation anastomotic biliary stricture: multiple plastic versus metal stents: a systematic review. Gastrointest Endosc. 2013;77:679–691. doi: 10.1016/j.gie.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 50.Kurita A, Kodama Y, Minami R, Sakuma Y, Kuriyama K, Tanabe W, Ohta Y, Maruno T, Shiokawa M, Sawai Y, Uza N, Yazumi S, Yoshizawa A, Uemoto S, Chiba T. Endoscopic stent placement above the intact sphincter of Oddi for biliary strictures after living donor liver transplantation. J Gastroenterol. 2013;48:1097–1104. doi: 10.1007/s00535-012-0705-x. [DOI] [PubMed] [Google Scholar]
- 51.Villa NA, Harrison ME. Management of Biliary Strictures After Liver Transplantation. Gastroenterol Hepatol (NY) 2015;11:316–328. [PMC free article] [PubMed] [Google Scholar]
- 52.Weiss S, Schmidt SC, Ulrich F, Pascher A, Schumacher G, Stockmann M, Puhl G, Guckelberger O, Neumann UP, Pratschke J, Neuhaus P. Biliary reconstruction using a side-to-side choledochocholedochostomy with or without T-tube in deceased donor liver transplantation: a prospective randomized trial. Ann Surg. 2009;250:766–771. doi: 10.1097/SLA.0b013e3181bd920a. [DOI] [PubMed] [Google Scholar]
- 53.Kaffes A, Griffin S, Vaughan R, James M, Chua T, Tee H, Dinesen L, Corte C, Gill R. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol. 2014;7:64–71. doi: 10.1177/1756283X13503614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee HW, Shah NH, Lee SK. An Update on Endoscopic Management of Post-Liver Transplant Biliary Complications. Clin Endosc. 2017;50:451–463. doi: 10.5946/ce.2016.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Macías-Gómez C, Dumonceau JM. Endoscopic management of biliary complications after liver transplantation: An evidence-based review. World J Gastrointest Endosc. 2015;7:606–616. doi: 10.4253/wjge.v7.i6.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yazumi S, Chiba T. Endoscopic management of biliary stricture after right-lobe living-donor liver transplantation with biliary anastomosis. Clin Gastroenterol Hepatol. 2006;4:1296; author reply 1296. doi: 10.1016/j.cgh.2006.07.019. [DOI] [PubMed] [Google Scholar]
- 57.Park JS, Kim MH, Lee SK, Seo DW, Lee SS, Han J, Min YI, Hwang S, Park KM, Lee YJ, Lee SG, Sung KB. Efficacy of endoscopic and percutaneous treatments for biliary complications after cadaveric and living donor liver transplantation. Gastrointest Endosc. 2003;57:78–85. doi: 10.1067/mge.2003.11. [DOI] [PubMed] [Google Scholar]
- 58.Verdonk RC, Buis CI, van der Jagt EJ, Gouw AS, Limburg AJ, Slooff MJ, Kleibeuker JH, Porte RJ, Haagsma EB. Nonanastomotic biliary strictures after liver transplantation, part 2: Management, outcome, and risk factors for disease progression. Liver Transpl. 2007;13:725–732. doi: 10.1002/lt.21165. [DOI] [PubMed] [Google Scholar]
- 59.Choi JH, Lee SK. Percutaneous transhepatic cholangioscopy: does its role still exist? Clin Endosc. 2013;46:529–536. doi: 10.5946/ce.2013.46.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chang JH, Lee IS, Chun HJ, Choi JY, Yoon SK, Kim DG, You YK, Choi MG, Choi KY, Chung IS. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver. 2010;4:68–75. doi: 10.5009/gnl.2010.4.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shin M, Joh JW. Advances in endoscopic management of biliary complications after living donor liver transplantation: Comprehensive review of the literature. World J Gastroenterol. 2016;22:6173–6191. doi: 10.3748/wjg.v22.i27.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Karagyozov P, Boeva I Tishkov I. The benefits of adding digital cholangioscopy in the evaluation and treatment of post-transplant biliary complication. Gastrointest Endosc. 2020;5S:AB304. [Google Scholar]
- 63.Wright H, Sharma S, Gurakar A, Sebastian A, Kohli V, Jabbour N. Management of biliary stricture guided by the Spyglass Direct Visualization System in a liver transplant recipient: an innovative approach. Gastrointest Endosc. 2008;67:1201–1203. doi: 10.1016/j.gie.2007.10.055. [DOI] [PubMed] [Google Scholar]
- 64.Kochhar G, Parungao JM, Hanouneh IA, Parsi MA. Biliary complications following liver transplantation. World J Gastroenterol. 2013;19:2841–2846. doi: 10.3748/wjg.v19.i19.2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shah SA, Grant DR, McGilvray ID, Greig PD, Selzner M, Lilly LB, Girgrah N, Levy GA, Cattral MS. Biliary strictures in 130 consecutive right lobe living donor liver transplant recipients: results of a Western center. Am J Transplant. 2007;7:161–167. doi: 10.1111/j.1600-6143.2006.01601.x. [DOI] [PubMed] [Google Scholar]
- 66.Dumonceau JM, Tringali A, Blero D, Devière J, Laugiers R, Heresbach D, Costamagna G European Society of Gastrointestinal Endoscopy. Biliary stenting: indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2012;44:277–298. doi: 10.1055/s-0031-1291633. [DOI] [PubMed] [Google Scholar]
- 67.Irani S, Baron TH, Law R, Akbar A, Ross AS, Gluck M, Gan I, Kozarek RA. Endoscopic treatment of nonstricture-related benign biliary diseases using covered self-expandable metal stents. Endoscopy. 2015;47:315–321. doi: 10.1055/s-0034-1391093. [DOI] [PubMed] [Google Scholar]
- 68.Luigiano C, Bassi M, Ferrara F, Fabbri C, Ghersi S, Morace C, Consolo P, Maimone A, Galluccio G, D'Imperio N, Cennamo V. Placement of a new fully covered self-expanding metal stent for postoperative biliary strictures and leaks not responding to plastic stenting. Surg Laparosc Endosc Percutan Tech. 2013;23:159–162. doi: 10.1097/SLE.0b013e318278c201. [DOI] [PubMed] [Google Scholar]
- 69.Ayoub WS, Esquivel CO, Martin P. Biliary complications following liver transplantation. Dig Dis Sci. 2010;55:1540–1546. doi: 10.1007/s10620-010-1217-2. [DOI] [PubMed] [Google Scholar]
- 70.Phillips MS, Bonatti H, Sauer BG, Smith L, Javaid M, Kahaleh M, Schmitt T. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy. 2011;43:512–517. doi: 10.1055/s-0030-1256389. [DOI] [PubMed] [Google Scholar]
- 71.Spier BJ, Pfau PR, Lorenze KR, Knechtle SJ, Said A. Risk factors and outcomes in post-liver transplantation bile duct stones and casts: A case-control study. Liver Transpl. 2008;14:1461–1465. doi: 10.1002/lt.21511. [DOI] [PubMed] [Google Scholar]
- 72.Sheng R, Ramirez CB, Zajko AB, Campbell WL. Biliary stones and sludge in liver transplant patients: a 13-year experience. Radiology. 1996;198:243–247. doi: 10.1148/radiology.198.1.8539387. [DOI] [PubMed] [Google Scholar]
- 73.Farouk M, Branum GD, Watters CR, Cucchiaro G, Helms M, McCann R, Bollinger R, Meyers WC. Bile compositional changes and cholesterol stone formation following orthotopic liver transplantation. Transplantation. 1991;52:727–730. [PubMed] [Google Scholar]
- 74.Waldram R, Williams R, Calne RY. Bile composition and bile cast formation after transplantation of the liver in man. Transplantation. 1975;19:382–387. doi: 10.1097/00007890-197505000-00004. [DOI] [PubMed] [Google Scholar]
- 75.Maheshwari A, Maley W, Li Z, Thuluvath PJ. Biliary complications and outcomes of liver transplantation from donors after cardiac death. Liver Transpl. 2007;13:1645–1653. doi: 10.1002/lt.21212. [DOI] [PubMed] [Google Scholar]
- 76.Rerknimitr R, Sherman S, Fogel EL, Kalayci C, Lumeng L, Chalasani N, Kwo P, Lehman GA. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc. 2002;55:224–231. doi: 10.1067/mge.2002.120813. [DOI] [PubMed] [Google Scholar]
- 77.Lisotti A, Caponi A, Gibiino G, Muratori R. Safety and efficacy of extracorporeal shock-wave lithotripsy in the management of biliary stones after orthotopic liver transplantation. Dig Liver Dis. 2015;47:817–818. doi: 10.1016/j.dld.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 78.Gürakar A, Wright H, Camci C, Jaboour N. The application of SpyScope® technology in evaluation of pre and post liver transplant biliary problems. Turk J Gastroenterol. 2010;21:428–432. doi: 10.4318/tjg.2010.0131. [DOI] [PubMed] [Google Scholar]
- 79.Nam K, Lee SK, Song TJ, Park DH, Lee SS, Seo DW, Kim MH. Percutaneous transhepatic cholangioscopy for biliary complications after liver transplantation: a single center experience. J Hepatobiliary Pancreat Sci. 2016;23:650–657. doi: 10.1002/jhbp.388. [DOI] [PubMed] [Google Scholar]
- 80.Gor NV, Levy RM, Ahn J, Kogan D, Dodson SF, Cohen SM. Biliary cast syndrome following liver transplantation: Predictive factors and clinical outcomes. Liver Transpl. 2008;14:1466–1472. doi: 10.1002/lt.21492. [DOI] [PubMed] [Google Scholar]
- 81.Starzl TE, Putnam CW, Hansbrough JF, Porter KA, Reid HA. Biliary complications after liver transplantation: with special reference to the biliary cast syndrome and techniques of secondary duct repair. Surgery. 1977;81:212–221. [PubMed] [Google Scholar]
- 82.Voigtländer T, Negm AA, Strassburg CP, Lehner F, Manns MP, Lankisch TO. Biliary cast syndrome post-liver transplantation: risk factors and outcome. Liver Int. 2013;33:1287–1292. doi: 10.1111/liv.12181. [DOI] [PubMed] [Google Scholar]
- 83.Navaneethan U, Venkatesh PG, Al Mohajer M, Gelrud A. Successful diagnosis and management of biliary cast syndrome in a liver transplant patient using single operator cholangioscopy. JOP. 2011;12:461–463. [PubMed] [Google Scholar]
- 84.Zajko AB, Bennett MJ, Campbell WL, Koneru B. Mucocele of the cystic duct remnant in eight liver transplant recipients: findings at cholangiography, CT, and US. Radiology. 1990;177:691–693. doi: 10.1148/radiology.177.3.2243970. [DOI] [PubMed] [Google Scholar]
- 85.Chatterjee S, Das D, Hudson M, Bassendine MF, Scott J, Oppong KE, Sen G, French JJ. Mucocele of the cystic duct remnant after orthotopic liver transplant: a problem revisited. Exp Clin Transplant. 2011;9:214–216. [PubMed] [Google Scholar]
- 86.Torres V, Martinez N, Lee G, Almeda J, Gross G, Patel S, Rosenkranz L. How do we manage post-OLT redundant bile duct? World J Gastroenterol. 2013;19:2501–2506. doi: 10.3748/wjg.v19.i16.2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Park TY, Lee SK, Nam K, Oh D, Song TJ, Park DH, Lee SS, Seo DW, Kim MH. Spontaneous hemobilia after liver transplantation: Frequency, risk factors, and outcome of endoscopic management. J Gastroenterol Hepatol. 2017;32:583–588. doi: 10.1111/jgh.13497. [DOI] [PubMed] [Google Scholar]
- 88.Shinjo K, Matsubayashi H, Matsui T, Kawata N, Uemura S, Yamamoto Y, Ono H. Biliary hemostasis using an endoscopic plastic stent placement for uncontrolled hemobilia caused by transpapillary forceps biopsy (with video) Clin J Gastroenterol. 2016;9:86–88. doi: 10.1007/s12328-016-0637-8. [DOI] [PubMed] [Google Scholar]
- 89.Goenka MK, Harwani Y, Rai V, Goenka U. Fully covered self-expandable metal biliary stent for hemobilia caused by portal biliopathy. Gastrointest Endosc. 2014;80:1175. doi: 10.1016/j.gie.2014.03.029. [DOI] [PubMed] [Google Scholar]
- 90.Pasha SF, Harrison ME, Das A, Nguyen CC, Vargas HE, Balan V, Byrne TJ, Douglas DD, Mulligan DC. Endoscopic treatment of anastomotic biliary strictures after deceased donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2007;66:44–51. doi: 10.1016/j.gie.2007.02.017. [DOI] [PubMed] [Google Scholar]