Abstract
Background
The SarsCoV2, novel coronavirus (COVID-19) pandemic necessitated a rapid transition from in-person evaluations to remote delivery of care, including both video and telephone visits, in allergy/immunology practices.
Objective
To evaluate patient satisfaction, patient and physician impression of encounter completeness, and reimbursement between in-person, video, and telephone encounters. This study also assessed factors influencing patient satisfaction, perception of completeness, and choice of future evaluation type.
Methods
This was a prospective study of all encounters at a health care–system owned practice. Encounter type, encounter modality, patient demographics, primary diagnoses, reimbursement data, and physician assessment of encounter completeness were tracked. Patient satisfaction was assessed via standardized questions.
Results
There were 447 encounters, with 303 in-person (67.8%), 98 video (21.9%), and 46 telephone (10.3%). Patient satisfaction data was obtained from 251 patients. There was similar patient satisfaction among all encounter modalities. Both patients and physicians were more likely to deem an in-person encounter as complete. Physicians were more likely to report an in-person encounter to be complete for food allergy (P < .001) and chronic rhinitis (P = .001) compared with video or telephone, whereas patients reported in-person encounters for food allergy to be complete compared with other modalities (P = .002). Patients reported that future encounter types should depend on the clinical situation.
Conclusions
There was similar patient satisfaction with in-person, video, and telephone encounters in an allergy/immunology practice during the COVID-19 pandemic. Chronic rhinitis and food allergy are more likely to call for an in-person evaluation. New patient visits are likely to be the highest yield to focus on for in-person evaluations.
Key words: Telemedicine, Telehealth, Video visit, Telephone, Allergy/immunology evaluation, COVID-19, Patient satisfaction
Abbreviations used: COVID-19, SarsCoV2, novel coronavirus; FU, Follow-up; IQR, Interquartile range; NP, New patient
What is already known about this topic? Patient satisfaction with remote visits during the COVID-19 pandemic has previously been reported.
What does this article add to our knowledge? This study demonstrates similar patient satisfaction among in-person, video, and telephone encounters but shows that patients and physicians were most likely to report encounter completeness with in-person visits, especially with food allergy and chronic rhinitis. There was no difference between video and telephone encounter perception of completeness among patients and physicians.
How does this study impact current management guidelines? This information can be immediately applied to scheduling patients in allergy/immunology practices to optimize space, time, and safety during the COVID-19 pandemic.
Introduction
The term telemedicine was first used in the 1970s. Taken literally, it means “health from a distance.”1 Historically, this distance was physical distance from health care access, and telemedicine helped to overcome this barrier. However, at the onset of the SarsCoV2, novel coronavirus (COVID-19), global pandemic, the distance became social in nature owing to widespread recommendations aimed at mitigating virus transmission.2 Many health care providers, including allergy/immunology specialists, were forced to quickly change their mode of care delivery from in-person evaluations to telemedicine evaluations, including both video and telephone encounters.3 The widespread adoption of telemedicine was in contrast to prior to the COVID-19 pandemic, when allergy/immunology uptake of telemedicine had been minimal.4
Multiple studies have previously demonstrated patient satisfaction with telemedicine during the COVID-19 pandemic.5, 6, 7 Although the pandemic persists, case numbers, increased testing, use of personal protective equipment, and the need to maintain economic viability has allowed for opening of medical facilities for nonemergent and routine in-person encounters. Previous reports5, 6, 7 regarding telemedicine focused only on video visits and did not include patient satisfaction data regarding in-person or telephone versus video encounters during the same time period.
The New York on Pause8 measures successfully decreased the prevalence of COVID-19 by early summer, allowing our health care system to resume in-person evaluations in May 2020, although our allergy/immunology practice continued video and telephone encounters in addition to in-person evaluations. We, therefore, sought to compare patient satisfaction among different encounter modalities, provider and patient assessment of visit completeness, and reimbursement information across modalities. We also assessed whether patient demographics and primary diagnoses influenced patient satisfaction, perception of completeness, and choice of future evaluation type.
Methods
Setting and data collection
This was a single-center, prospective study conducted by two allergy/immunology physicians (S.S.M. and A.R.) at the Rochester Regional Health Allergy/Immunology practice, a health care system–owned practice, in Rochester, N.Y., from June 26, 2020, through July 31, 2020. During this time period, new patients (NPs) and follow-up patients (FUs) were evaluated in-person, via video, or via telephone. Video visits were conducted via Epic Warp (EHR, Verona, Wis), Skype (Palo Alto, Calif), FaceTime (Apple, Cupertino, Calif), and Doximity (San Francisco, Calif) depending on patient preference. The NPs were encouraged to schedule in-person evaluations, given the greater likelihood of needing diagnostic testing, with the reassurance that office staff and patients would maintain social distancing and use personal protective equipment. All patients evaluated by the participating physicians by any encounter modality were tracked. Patient age, gender, NP versus FU, encounter modality, primary diagnoses, billing codes, and physician impression of visit completeness were recorded prospectively. Patients were contacted regarding their visit satisfaction either via phone or via electronic health record messaging by a research nurse within 7 days of their visit with standardized questions. The study was approved by the institutional review board.
Satisfaction data collection
All patients were asked the following questions, with answer options listed after each question. Questions #6 and #7 were open-ended.
-
1.What is your current level of concern of being exposed to COVID-19 during a doctor visit?
- Not concerned, minimally concerned, very concerned
-
2.Overall, I was satisfied with my in-person/video/telephone encounter
- Strongly disagree, disagree, neutral, agree, strongly agree
-
3.My in-person/video/telephone encounter resulted in a complete evaluation
- Yes, no
-
4.In the future, I would prefer the following visit type
- In-person, video, telephone, any would be acceptable, depends on clinical situation
-
5.Patient copays should be the same regardless of appointment type
- Strongly disagree, disagree, neutral, agree, strongly agree
-
6.
What is the most important reason you would prefer an in-person encounter?
-
7.
What is the most important reason you would prefer a video or telephone encounter?
Outcome measures and data analysis
The primary outcome measures were patient satisfaction with each encounter modality. In addition, we assessed whether there was an association between physician and patient impression of evaluation completeness depending on encounter type, primary diagnosis, age, and gender. We also assessed whether there was an association between patient level of concern for COVID-19 and encounter type. We tracked reimbursement information for each encounter modality. In addition, we evaluated patient opinion of copay and future encounter type. Lastly, we categorized patient responses to the open-ended questions into recurring themes.
Statistical analysis
Statistical analysis was performed using STATA software (StataCorp LLC, College Station, Texas). Baseline characteristics and patient responses are reported as medians and interquartile ranges (IQRs) for continuous variables and proportions for categorical variables. We used the chi-square test of association to describe the significance of the association between baseline characteristics, encounter modalities, and patient satisfaction responses. Microsoft Excel software (Office 365; , Microsoft Corporation, Redmond, Wash) was used to create the figures.
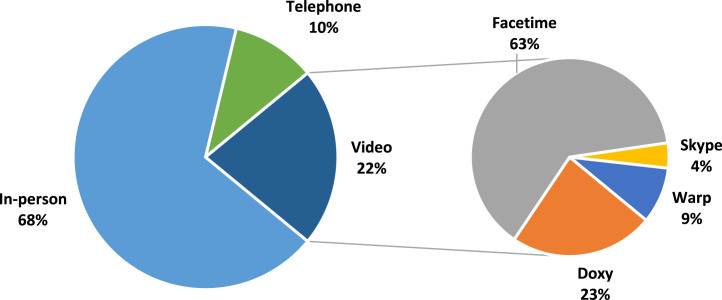
Results
There were a total of 447 unique patient encounters during the study period, with patient survey data completed for 251 encounters (56.2%). Of the 447 encounters, 303 (67.8%) were in-person, 98 (21.9%) were via video, and 46 (10.3%) were via telephone (Table I ). For the in-person group, the median age was 20 years (IQR 6-53), 167 (55%) were female, 184 (60.7%) were NP visits, and 119 (39.3%) were FU visits. The most common primary diagnoses for in-person encounters were food allergy (33.3%), chronic rhinitis/sinusitis (22.4%), and asthma (10.2%). For the video group, the median age was 29 years (IQR 11-53), 57 (58.1%) were female, 6 (6.1%) were NP, and 92 (93.9%) were FU visits. The most common primary diagnoses for video encounters were asthma (29.5%), chronic rhinitis/sinusitis (26.5%), and food allergy (16.3%). The most common video platform used was FaceTime, in 63% of patients, followed by Doximity in 23% of patients (Figure 1 ). For the telephone group, the median age was 48 years (IQR 29-61), 33 (71.7%) were female, and all 46 evaluations were FUs. The most common primary diagnoses in the telephone encounters were chronic rhinitis/sinusitis (32.6%), asthma (28.3%), and food allergy (10.9%). See Table I for additional demographic details.
Table I.
Patient demographics∗
| Characteristic | In-Person | Video | Telephone |
|---|---|---|---|
| n | 303 | 98 | 46 |
| Age, y | 20 (6-52.5) | 29 (11-52.5) | 48 (28.7-61) |
| Female | 167 (55.1%) | 57 (58.1%) | 33 (71.7%) |
| NP | 184 (60.7%) | 6 (6.1%) | 0 |
| FU | 119 (39.3%) | 92 (93.9%) | 46 (100%) |
| Primary diagnosis | |||
| Food allergy | 101 (33.3%) | 16 (16.3%) | 5 (10.9%) |
| Chronic rhinitis/sinusitis | 68 (22.4%) | 26 (26.5%) | 15 (32.6%) |
| Asthma | 31 (10.2%) | 29 (29.5%) | 13 (28.3%) |
| Urticaria/angioedema | 24 (7.9%) | 7 (7.1%) | 3 (6.5%) |
| Drug allergy | 21 (6.9%) | 0 | 0 |
| Dermatitis | 19 (6.3%) | 4 (4.1%) | 1 (2.2%) |
| Other | 39 (12.8%) | 16 (16.3%) | 9 (19.6%) |
Continuous variables are expressed in median and IQR; discrete variables are expressed in count and frequency.
Figure 1.
Percentage of visit types.
Patients were satisfied with their encounters regardless of encounter modality. For in-person evaluations, 148 of 157 patients (94.3%) either strongly agreed or agreed with “Overall, I was satisfied with my in-person/video/telephone encounter” (Table II ). For video encounters, 61 of 66 patients (92.4%) strongly agreed or agreed with being satisfied with their encounter, and 23 of 28 patients (82.1%) felt the same of their telephone encounter. There was no difference between patient satisfaction with in-person, video, or telephone encounters (P = .069).
Table II.
Patient satisfaction
| Overall, I was satisfied with my encounter | In-person (n = 157) | Video (n = 66) | Telephone (n = 28) |
|---|---|---|---|
| Strongly disagree | 3 (1.9%) | 1 (1.5%) | 1 (3.6%) |
| Disagree | 2 (1.3%) | 0 | 1 (3.6%) |
| Neutral | 4 (2.5%) | 4 (6.1%) | 3 (10.7%) |
| Agree | 20 (12.7%) | 13 (19.7%) | 7 (25%) |
| Strongly agree | 128 (81.5%) | 48 (72.7%) | 16 (57.1%) |
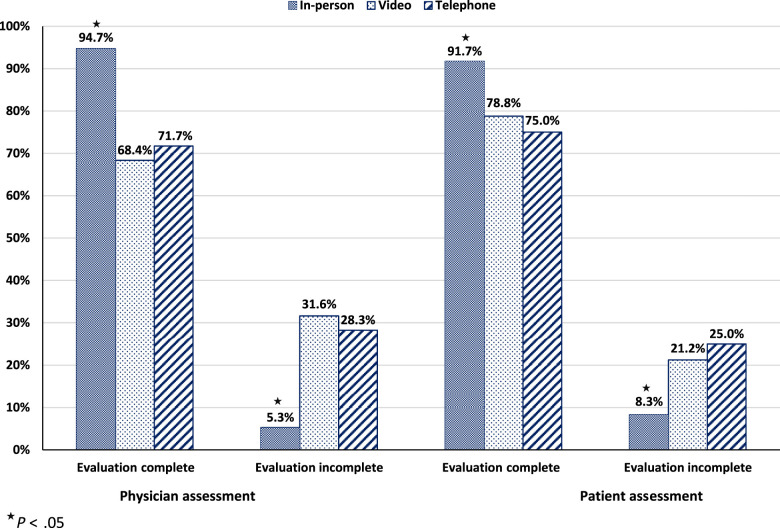
However, patient impression of visit completeness did depend on encounter modality (Figure 2 ). For in-person encounters, 144 of 157 patients (91.7%) reported their encounter resulted in a complete evaluation, compared with 52 of 66 patients (78.8%) who had a video encounter, and 21 of 28 patients (75%) who had a telephone encounter (P = .006). There was no difference between a video and a telephone encounter and patient impression of visit completeness (P = .687). Physicians reported in-person encounters led to a complete evaluation of 287 of 303 patients (94.7%), compared with 67 of 98 of video encounters (68.4%), and 33 of 46 of telephone encounters (71.7%) (P < .001). There was no significant difference between video and telephone encounters and physician assessment of completeness (P = .682). In addition, physicians were more likely to report in-person evaluations to be complete for food allergy (P < .001) and chronic rhinitis (P = .001) compared with other encounter modalities. There was no significant difference between encounter modality and physician-reported completeness for other diagnoses, including asthma and urticaria (Table III ). Patients evaluated for food allergy were more likely to report an in-person evaluation to be complete compared with a video or telephone visit (P = .002) (Table IV ). There was no such association with the diagnoses of asthma, chronic rhinitis, chronic sinusitis, dermatitis, or drug allergy, regardless of evaluation modality. Lastly, there was no difference in patient assessment of encounter completeness between gender, with 170 of 190 men (89.4%) feeling they had complete encounters versus 217 of 257 woman (84%) (P = .07) or between children younger than 18 years old, 176 of 199 (88.4%), and adults, 211 of 248 (85.1%) (P = .185).
Figure 2.
Physician and patient perception of the completeness of the evaluation.
Table III.
Doctor's perception of encounter completeness by primary diagnosis
| Diagnosis | Total | In-person |
Video |
Telephone |
P value | |||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |||
| Asthma | 73 | 26 (35.6%) | 5 (6.8%) | 19 (26%) | 10 (13.7%) | 10 (13.7%) | 3 (4.1%) | .254 |
| Chronic rhinitis/sinusitis | 109 | 65 (59.6%) | 3 (2.7%) | 22 (20.1%) | 4 (3.6%) | 9 (8.2%) | 6 (5.5%) | .001 |
| Dermatitis | 24 | 18 (75%) | 1 (4.1%) | 3 (12.5%) | 1 (4.1%) | 1 (4.1%) | 0 | .380 |
| Drug allergy | 21 | 19 (90.4%) | 2 (9.5%) | 0 | 0 | 0 | 0 | NA |
| Food allergy | 122 | 101 (82.7%) | 0 | 5 (4.1%) | 11 (9.2%) | 2 (1.6%) | 3 (2.4%) | <.001 |
| Urticaria/angioedema | 34 | 24 (70.5%) | 0 | 6 (17.6%) | 1 (2.9%) | 3 (8.8%) | 0 | .294 |
Table IV.
Patient's perception of encounter completeness by primary diagnosis
| Diagnosis | Total | In-person |
Video |
Telephone |
P value | |||
|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |||
| Asthma | 46 | 16 (34.7%) | 4 (8.7%) | 17 (36.9%) | 3 (6.5%) | 4 (8.7%) | 2 (4.3%) | .680 |
| Chronic rhinitis/sinusitis | 59 | 29 (49.1%) | 4 (6.7%) | 15 (25.4%) | 4 (6.7%) | 5 (8.4%) | 2 (3.3%) | .229 |
| Dermatitis | 13 | 7 (53.8%) | 2 (15.3%) | 2 (15.3%) | 1 (7.6%) | 1 (7.6%) | 0 | >.999 |
| Drug allergy | 10 | 10 (100%) | 0 | 0 | 0 | 0 | 0 | NA |
| Food allergy | 66 | 53 (80.3%) | 1 (1.5%) | 4 (6%) | 3 (4.5%) | 4 (6%) | 1 (1.5%) | .002 |
| Urticaria/angioedema | 20 | 11 (55%) | 1 (5%) | 3 (15%) | 2 (10%) | 3 (15%) | 0 | .186 |
The most commonly cited reason that patients preferred an in-person encounter was to have a physical examination (25.9%) (Table V ). Patients almost equally cited that “in-person care is better for serious conditions,” “in-person care allows for a more personal interaction and more questions,” and “I want allergy and/or breathing tests.” The most common reasons cited for utilizing a video or telephone encounter were “routine follow-up or simple visit” (32.8%), “more convenient” (23.8%), and they “feel safer during COVID-19 pandemic” (13.5%) (Table V).
Table V.
Patient free text responses
| What is the most important reason you would prefer an in-person encounter? (n = 247) | |
| I want a physical examination | 64 (25.9%) |
| In-person care is better for serious conditions | 56 (22.6%) |
| In-person care allows for a more personal interaction and more questions | 52 (21%) |
| I want allergy and/or breathing tests | 52 (21%) |
| I have a greater comfort level in-person | 17 (6.8%) |
| I want to avoid technological difficulties | 6 (2.4%) |
| What is the most important reason you would prefer a video/telephone encounter? (n = 222) | |
| Routine FU or simple visit | 73 (32.8%) |
| More convenient | 53 (23.8%) |
| Feel safer during COVID-19 pandemic | 30 (13.5%) |
| Safer option when I am feeling sick | 20 (9%) |
| No testing or examination needed | 19 (8.6) |
| Easier for an acute visit | 11 (4.9%) |
| Only if doctor's office is closed | 10 (4.5%) |
| Quicker access to an appointment | 6 (2.7%) |
Values are n (%).
The minority of patients reported being very concerned about the COVID-19 pandemic; 22 of 157 patients (14%) evaluated in-person, 3 of 66 (4.5%) evaluated via video, and 4 of 28 (14.3%) evaluated via telephone, with no difference between encounter modality (P = .190).
In-person encounters yielded greater median reimbursement of $304.03 (IQR $187.40-$589.30) compared with $116.57 (IQR $116.00-$172.00) for video encounters and $92.82 (IQR $69.00-$116.50) for telephone encounters (P = .001). Video encounters generated higher reimbursement than telephone encounters (P < .001). Patients across all encounter modalities wished to choose an evaluation modality based on the clinical situation (P = .001). Patient impression of copays did not differ depending on encounter modality (P = .099).
Discussion
Our analysis is the first to compare allergy/immunology in-person, video, and telephone encounters during the COVID-19 pandemic. Importantly, we demonstrate comparable patient satisfaction across all encounter types. We show that both physicians and patients reported the highest visit completeness for in-person encounters, but there was no difference between video and telephone encounters. Importantly, physician impression of completeness for managing urticaria and asthma was the same across all encounter modalities. Conversely, physicians reported a higher likelihood of complete evaluation when seeing patients in-person for chronic rhinitis and food allergy. Patients evaluated for food allergy felt in-person encounters led to more complete evaluations than video or telephone encounters. In our study, patients indicated that they would like to choose their future encounter type based on the clinical situation.
Recent work by Thomas et al9 out of the United Kingdom looked at synchronous telephone encounters only. Similar to our data, most of these patients (85%) were satisfied with their evaluations; however, there was no comparison with video or in-person encounters. The authors reported that food allergy was the most common diagnosis requiring further evaluation, which is consistent with our data of food allergy evaluations most likely to call for an in-person evaluation. Thomas et al's report9 that most of their assessments for urticaria and angioedema were successfully completed by telephone evaluation is also consistent with our data. Another recent study by Lanier et al7 of 289 video encounters also demonstrated a high rate of patient satisfaction. The breakdown of allergy diagnoses in this study were different from ours in that they reported 20% of their population was seen for immune deficiency and only 14% were seen for rhinitis.7 Their analysis found that only 46% of patients would prefer a video visit postpandemic,7 whereas our results demonstrate that patients would most often choose future encounter modality based on the clinical situation. Lanier et al7 showed that being of Caucasian race was significantly more likely to report comfort with a video encounter than Hispanic patients. This is an important finding that we did not analyze for our study. Importantly, Kahwash et al10 recently demonstrated that the majority of allergy/immunology trainees have also used remote evaluations and are comfortable doing so, which is helpful when planning for implementation of telemedicine following the COVID-19 pandemic.
Our data add to the existing and growing body of literature regarding the expanding role of telemedicine visits in the allergy/immunology field.11 , 12 As we continue to face the COVID-19 pandemic, emerging data are reassuring that patients are satisfied with their evaluations regardless of encounter type and provide guidance for targeting specific diagnoses for certain encounter modalities.9 Food allergy and chronic rhinitis evaluations may require in-person evaluations in order to complete appropriate diagnostic testing such as skin testing, whereas urticaria may be adequately addressed via video or telephone encounters. Our data also show that patients believe encounter modality should depend on the clinical situation, and this presents an opportunity for shared decision making when deciding how to schedule future appointments. Surprisingly, there was no difference in comfort using telemedicine with respect to age. We believe this information can be immediately applied to scheduling patients in allergy/immunology practices to optimize space, time, and safety during the COVID-19 pandemic.
During the course of our study, our office focused on scheduling NPs for in-person encounters. We believe this is the most practical approach because we demonstrate that an in-person NP encounter was most likely to result in an impression of a complete visit and maximal reimbursement than other encounter types. We previously demonstrated that video and telephone encounters alone are not likely to be financially sustainable for an allergy immunology practice,3 and this current hybrid scheduling approach is more sustainable. In our analysis, patients also expressed wishes to have in-person evaluations for physical examinations, building rapport with their physician, and necessary diagnostic testing. A NP in-person evaluation accomplishes all of these goals, and then may lay the groundwork to have productive subsequent video or telephone visits. Patients were agreeable to video and telephone encounters for routine or simple FU, and cited convenience as a strength of these encounters. Although telephone encounters did not reimburse as well as video encounters, our analysis demonstrates that these modalities were deemed equally complete by patients and physicians. We, therefore, offer that telephone encounters may be easily added to a provider schedule as a way to maintain patient access for short, routine FUs without concern for technological barriers with video encounters or space considerations for in-person evaluations.
We acknowledge that a weakness of our study is that approximately half of eligible patients responded to the survey, and these patients may have had an established physician/patient relationship with the authors. Despite being contacted by an independent research nurse, there is likely to be an element of response bias for both of these reasons. Although including pediatric patients is a strength of our analysis, parents answered on behalf of their children for satisfaction survey. We also did not evaluate patient satisfaction with respect to reported race or language spoken, and this may have been enlightening in regards to health care disparities. Even though a larger sample size is always desirable, we wished to put forth this information in a timely manner during the COVID-19 pandemic. Lastly, our results and suggestions for practical implementation of various encounter modalities will depend on the local response to the COVID-19 pandemic, which varies greatly from state to state. In addition, the practice setting (private vs academic) will likely also significantly contribute to these decisions based on varying reimbursement models.
In summary, we demonstrate patient satisfaction with in-person, video, and telephone encounters in an allergy/immunology practice during the COVID-19 pandemic. Certain diagnoses, such as urticarial, lend themselves particularly well to a remote evaluation, whereas chronic rhinitis and food allergy are more likely to necessitate an in-person encounter. New patient visits are likely to be the highest yield to focus on for in-person evaluations. We believe that our data will help allergy/immunology practices optimize patient scheduling during the COVID-19 pandemic and beyond.
Footnotes
Funding: No funding has been received for this study.
Conflicts of interest: S. S. Mustafa is on the Speaker's bureaus of Sanofi/Regeneron, Genentech, AstraZeneca, CSL Behring, and GlaxoSmithKline
A. Ramsey is on the Speaker's bureaus of Sanofi/Regeneron, and GlaxoSmithKline
K. Vadamalai declares that he has no relevant conflicts of interest.
References
- 1.Strehle E.M., Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child. 2006;91:956–959. doi: 10.1136/adc.2006.099622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y., et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramsey A., Yang L., Vadamalai K., Mustafa S.S. Appointment characteristics in an allergy/immunology practice in the immediate aftermath of COVID-19 restrictions. J Allergy Clin Immunol Pract. 2020;8:2771–2773. doi: 10.1016/j.jaip.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane C.K., Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood) 2018;37:1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 5.Portnoy J., Waller M., Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mustafa S.S., Yang L., Vadalamai K., Ramsey A. Patient satisfaction with telemedicine encounters in an allergy and immunology practice during the coronavirus disease 2019 pandemic. Ann Allergy Asthma Immunol. 2020;125:478–479. doi: 10.1016/j.anai.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanier K., Kuruvilla M., Shih J. Patient satisfaction and utilization of telemedicine services in allergy: an institutional survey. J Allergy Clin Immunol Pract. 2021;9:484–486. doi: 10.1016/j.jaip.2020.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New York State Department of Health Home. https://coronavirus.health.ny.gov/home Available from:
- 9.Thomas I., Siew L.Q.C., Rutkowski K. Synchronous telemedicine in allergy: lessons learned and transformation of care during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2021;9:170–176.e1. doi: 10.1016/j.jaip.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahwash B.M., Deshpande D.R., Guo C., Panganiban C.M., Wangberg H., Craig T.M. Allergy/immunology trainee experiences during the COVID-19 pandemic: AAAAI Work Group Report of the Fellows-in-Training Committee. J Allergy Clin Immunol Pract. 2021;9:1–6.e1. doi: 10.1016/j.jaip.2020.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Portnoy J.M., Waller M., De Lurgio S., Dinakar C. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117:241–245. doi: 10.1016/j.anai.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Brown W., Odenthal D. The uses of telemedicine to improve asthma control. J Allergy Clin Immunol Pract. 2015;3:300–301. doi: 10.1016/j.jaip.2014.10.003. [DOI] [PubMed] [Google Scholar]