Abstract
Introduction: Cardiovascular diseases remain the leading cause of death and disease burden in China and worldwide. We aimed to evaluate the status of cardiovascular health among urban Chinese children and adolescents.
Methods: We conducted a cross-sectional study comprising 12,618 children and adolescents aged 6–18 years, who were recruited from Chinese urban areas during 2013–2015. The poor, intermediate, and ideal levels of 7 cardiovascular health metrics, including smoking, body mass index, dietary intake, physical activity, blood pressure, blood glucose, and total cholesterol were defined according to revised American Heart Association criteria.
Results: Ideal smoking status was the most prevalent health component (overall, 90.7%; males, 86.3% and females, 95.4%), whereas ideal health diet score (overall, 8.7%; males, 9.1% and females, 8.3%) was the least prevalent among urban Chinese children and adolescents. The majority (overall, 84.9%; males, 82.6% and females, 87.4%) of participants had 3–5 ideal metrics. The overall prevalence of ideal cardiovascular health (i.e. meeting all 7 ideal components) was extremely low (overall, 0.5%; males, 0.5% and females, 0.4%).
Conclusions: The prevalence of ideal cardiovascular health in urban Chinese children and adolescents is extremely low, particularly for physical activity and healthy dietary intake. Effective public health interventions are required to improve cardiovascular health in children and adolescents to reduce future cardiovascular risk.
Key messages
Ideal health diet score was the least prevalent health component among urban Chinese children and adolescents
The prevalence of ideal cardiovascular health in urban Chinese children and adolescents was extremely low
Effective public health interventions are required to improve cardiovascular health in children and adolescents to reduce future cardiovascular risk
Keywords: Child, adolescent, cardiovascular health, risk factor
Introduction
Cardiovascular disease (CVD) remains the leading cause of death and disease burden in China and worldwide [1,2]. In 2013, CVD accounted for 44.8% and 41.9% of the total deaths in Chinese urban and rural populations, respectively [3]. In 2010, the American Heart Association (AHA) set new national goals for cardiovascular health promotion and disease reduction through 2020 and beyond [4]. To monitor progress of these goals, AHA defined a construct of cardiovascular health for adults and youths based on seven health components, including four health behaviors (smoking, body mass index [BMI], physical activity and health diet score) and three health factors (total cholesterol [TC], blood pressure [BP] and fasting plasma glucose).
The progression of CVD begins at an early age [5]. Several traditional cardiovascular risk factors (e.g. obesity, elevated BP and dyslipidemia) track from childhood to adulthood [6–10], and increase risk of subclinical CVD in adulthood [11–13]. In addition, the number of ideal health metrics presented in childhood predicts subsequent cardiometabolic health in adulthood [14]. Understanding the current status of cardiovascular health among youths will provide evidence for developing effective strategies to prevent future cardiovascular events.
Data from the National Health and Nutrition Examination Surveys reported extremely low prevalence of ideal cardiovascular health among US adults and youths [15–17]. Several epidemiological studies demonstrated a very poor status of cardiovascular health in Chinese adults [18–21]. However, information is lacking regarding cardiovascular health among Chinese youths. Therefore, utilizing data from China Child and Adolescent Cardiovascular Health (CCACH) study, we aimed to evaluate the status of cardiovascular health among urban Chinese children and adolescents.
Materials and methods
The CCACH study is a population-based cross-sectional study conducted from 2013 to 2015, which was designed to select a representative sample of children and adolescents aged 6–18 years living in urban areas of China. We firstly stratified China into north and south regions by Qinling-Huaihe line according to their characteristics of climate, economic development and life habits. We then chose four cities from the north region (Beijing, Changchun, Jinan and Yinchuan) and three cities from the south region (Shanghai, Chongqing and Chengdu) using a nonrandom sampling method. Next, a list with name of all schools was obtained from local education commission for each city, and then several schools were randomly selected from the list. All students (n = 15,548) from the selected schools were invited to participate in a clinical examination, including a questionnaire survey, anthropometric measurements and blood sample collection. Finally, a total of 13,395 participants agreed and attended the examination, and the response rate was 86.2%.
After excluding participants who were aged <6 years or >18 years, participants who had missing values for analysis variables, and participants who had acute intercurrent febrile or diarrheal illness, the final sample included 12,618 children and adolescents. Participants with available data for individual health components (n = 7955 to 12,618) were included when examining the distribution of specified health components, while only participants with available data for all 7 health components (n = 7484) were included when examining the prevalence of overall ideal cardiovascular health and distribution of number of ideal components.
The study protocol was approved by the Institution Review Board of each centre and the written informed consents were obtained from all children and adolescents and/or their parents.
The study investigators and staff members from all centres completed a training program that taught the methods and process of the study. A manual of procedures was distributed, and detailed instructions for administration of the questionnaires, taking of blood pressure and anthropometric measurements, and biological specimen collection and processing were provided. Information on demographic characteristics, medical history and lifestyle factors (including smoking, physical activity and dietary habits) was collected by a self-administered questionnaire survey. Participants answered the questions by themselves mainly and in assistance of their parents when necessary. Physical activity was assessed by asking questions about the frequency and duration of specific activities according to intensity over the past 12 months. Vigorous-intensity activities were defined as activities that require hard physical effort and cause large increases in breathing or heart rate (e.g. running and aerobics) and moderate-intensity activities as activities that require moderate physical effort and cause small increases in breathing or heart rate (e.g. brisk walking and cycling). Diet habits were assessed by asking questions about the frequency of consumption of specific food items over the past 12 months.
Weight and height were measured to the nearest 0.1 kg and 0.1 cm in lightweight clothing without shoes (Jianmin II, China Institute of Sport Science, Beijing, China). Weight and height were measured twice and the mean values were used to calculate BMI (calculated as weight in kilograms divided by height in meters squared). The sex- and age-specific BMI percentiles were calculated according to both the US Centers for Disease Control 2000 growth charts and the Working Group on Obesity in China reference to explore their differences [22,23]. BP was measured using a calibrated automatic electronic sphygmomanometer (Omron HEM-7012, Omron Co., Kyoto, Japan), which has been clinically validated [24], according to a standardized protocol. After resting for at least 15 min, BP was measured in a sitting position on the right upper arm at the level of the heart. The appropriate cuff size was determined by the participant’s arm circumference. Systolic and diastolic BP was measured three times with 1–2 min intervals and the mean value of the last two readings was used for analysis. If a difference of more than 10 mmHg was obtained between the two adjacent BP readings, an additional measurement was obtained. The BP percentiles were calculated according to both the US Fourth Report references and BP references for Chinese children and adolescents to examine their differences [25,26].
After fasting for at least 12 hours, blood samples were collected from the antecubital vein in the morning and then were transfused into vacuum tubes containing ethylenediamine tetraacetic acid. Blood specimens were centrifuged at 2000 g for 10 minutes within 1 hour of collection at room temperature and then aliquoted and frozen at −80 °C. Plasma specimens collected in each centre were shipped by air in dry ice to the central clinical laboratory of Capital Institute of Pediatrics in Beijing, where the specimens were stored at −80 °C until laboratory assays were performed. Fasting glucose was measured by using an enzyme hexokinase method and TC was measured with the enzymatic method. These biochemical variables were measured using an autoanalyzer (Hitachi 7080; Hitachi, Tokyo, Japan). The inter-assay coefficient of variation was <10%.
The status of cardiovascular health is described according to AHA based on 7 health metrics, including 4 health behaviours (BMI, smoking, physical activity and diet score) and 3 health factors (BP, fasting blood glucose and TC) [4]. Each health metric was categorized as poor, intermediate and ideal according to the revised AHA criteria (Supplementary eTable 1). Ideal cardiovascular health was defined by coexistence of all 7 ideal health metrics.
We defined ideal, intermediate and poor levels of health diet score based on frequency information on the consumption of specific foods over past 12 months. Since information on whole grain and salt intake were not collected in our study, we added bean- or dairy-products and fried or western fast foods into the diet metrics. Individual components of healthy diet score included daily fruit and vegetable consumption, fish or fish products ≥2 times per week, daily dairy-products, fried or western fast foods ≤2 times per week and sugar-sweetened beverages ≤2 times per week. According to the AHA criteria, participants who had 4 or 5, 2 or 3 and 0 or 1 ideal diet components were classified as having ideal, intermediate and poor healthy diet scores, respectively.
Proportions for the 3 levels of the 7 metrics were performed in the total population and in subgroups of sex, age and region. Proportions for numbers of ideal health metrics ranging from 0 through 7, numbers of ideal health behaviours from 0 through 4, and numbers of ideal health factors through 0 through 3 were also calculated in the total population and in subgroups.
The comparisons between subgroups were performed using t tests for continuous variables and chi-square tests for categorical variables. Data analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina), and a 2-tailed p value <.05 was considered significant. Data were analyzed during 2017–2018.
Results
We finally included 12,618 individuals with available data for at least one health metric. Among them, 50.5% were males (n = 6394) and 40.5% aged 6–11 years (n = 5110). More participants (n = 8012, 63.5%) lived in the northern region than in the southern region. The number of participants for individual components ranged from 7955 for physical activity to 12,618 for smoking status. There were 7484 participants who had data on all 7 health metrics, 7514 who had data on all 4 health behaviours, and 12,014 who had data on all 3 health factors.
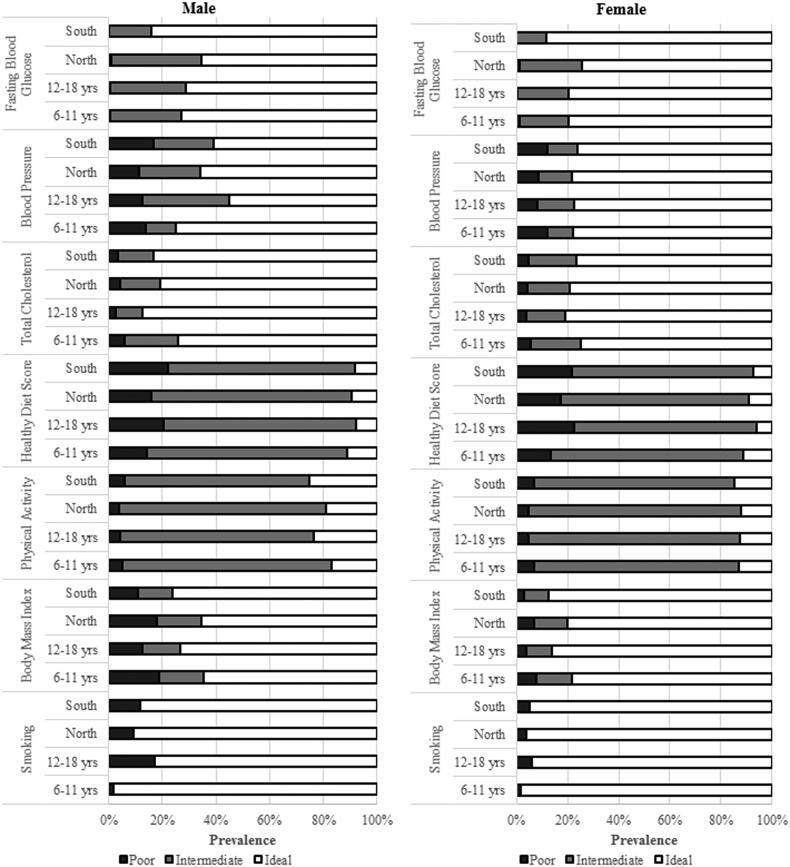
Table 1 and Figure 1 display the distributions of poor, intermediate and ideal levels of all 7 health metrics in the total population and in subgroups of sex, age and region. Ideal smoking status was the most prevalent health component (86.3% in males and 95.4% in females). Males and females aged 12–18 years tried smoking prior 30 days more frequently compared to participants aged 6–11 years. The majority of urban children and adolescents (77.3%) exhibited ideal BMI levels, and females versus males were less commonly overweight (i.e. intermediate levels) or obese (i.e. poor levels). Participants who were younger or lived in the northern region had higher prevalence of obesity for both sexes. Although only 5.2% of children and adolescents had poor physical activity levels, more than three-quarters had intermediate status. Females who were older or lived in south had higher prevalence of ideal physical activity.
Table 1.
Proportions (standard errors) of each individual cardiovascular health metric according to sex in urban Chinese children and adolescents aged 6–18 years in 2013–2015.
| Overall | Sex |
p | ||
|---|---|---|---|---|
| Males | Females | |||
| Smoking status | (n = 12,618) | (n = 6394) | (n = 6224) | |
| Poor (Tried prior 30 d) | 9.3 (0.3) | 13.7 (0.6) | 4.6 (0.3) | <.001 |
| Ideal (Never tried) | 90.7 (0.9) | 86.3 (1.2) | 95.4 (1.3) | |
| Body mass index | (n = 12,460) | (n = 6301) | (n = 6159) | |
| Poor (>95th percentile) | 9.9 (0.3) | 14.3 (0.5) | 5.0 (0.3) | <.001 |
| Intermediate (85–95th percentile) | 13.8 (0.3) | 14.4 (0.5) | 11.0 (0.4) | |
| Ideal (<85th percentile) | 77.3 (0.8) | 71.3 (1.2) | 84.0 (1.2) | |
| Physical activitya | (n = 7955) | (n = 4235) | (n = 3720) | |
| Poor | 5.2 (0.3) | 4.7 (0.4) | 5.7 (0.4) | <.001 |
| Intermediate | 78.2 (1.0) | 74.6 (1.4) | 82.2 (1.6) | |
| Ideal | 16.6 (0.5) | 20.7 (0.7) | 12.2 (0.6) | |
| Healthy Diet Score | (n = 10,449) | (n = 5298) | (n = 5151) | |
| Poor | 19.1 (0.5) | 18.7 (0.6) | 19.5 (0.7) | <.001 |
| Intermediate | 72.2 (0.9) | 72.2 (1.2) | 72.2 (1.2) | |
| Ideal | 8.7 (0.3) | 9.1 (0.4) | 8.3 (0.4) | |
| Total cholesterol | (n = 12,602) | (n = 6385) | (n = 6217) | |
| Poor (≥200 mg/dL) | 4.1 (0.2) | 3.8 (0.2) | 4.4 (0.3) | <.001 |
| Intermediate (170–199 mg/dL) | 15.2 (0.4) | 13.5 (0.5) | 17.0 (0.5) | |
| Ideal (<170 mg/dL) | 80.7 (0.9) | 82.7 (1.2) | 78.6 (1.2) | |
| Blood pressure | (n = 12,057) | (n = 6125) | (n = 5932) | |
| Poor (>95th percentile) | 11.1 (0.3) | 12.7 (0.5) | 9.4 (0.4) | <.001 |
| Intermediate (90–95th percentile) | 19.6 (0.5) | 26.0 (0.8) | 12.8 (0.5) | |
| Ideal (<90th percentile) | 69.3 (0.8) | 61.3 (1.0) | 77.8 (1.2) | |
| Fasting blood glucose | (n = 12,588) | (n = 6380) | (n = 6208) | |
| Poor (≥126 mg/dL) | 0.6 (0.1) | 0.7 (0.1) | 0.7 (0.1) | <.001 |
| Intermediate (100–125 mg/dL) | 22.9 (0.4) | 26.2 (0.7) | 19.1 (0.6) | |
| Ideal (<100 mg/dL) | 76.5 (0.8) | 73.1 (1.2) | 80.2 (1.2) | |
Numbers may not add up to 100% due to rounding. aPhysical activity was categorized as poor (no activity), intermediate (1–59 min/week moderate or vigorous activity every day), and ideal (≥60 min/week moderate or vigorous activity every day).
Figure 1.
Age- and region-specific distributions of individual cardiovascular health behaviours and factors in males and females.
Ideal health diet score was the least prevalent health component in the total population (8.7%) and across sex, age and region groups. Participants who were younger or lived in the northern region had higher prevalence of poor health diet score for both sexes. Most participants were classified as having 2–3 ideal dietary components. The proportions of participants who achieved the goal of each dietary component were 43.3% for fruits and vegetables, 21.9% for fish or fish products, 17.6% for bean- or dairy-products, 84.6% for fried food/western fast food, and 60.2% for sugar-sweetened beverages (Supplementary e Table 2).
Most participants had ideal TC levels in the total population and across all subgroups. Most participants had ideal BP levels (61.3% in males and 77.8% in females); however, 12.7% of males and 9.4% of females had elevated BP. Differences in the prevalence of ideal BP levels between age and region groups were observed in males but not in females. Approximately three-quarters of individuals had ideal levels of blood glucose and less than 1% had poor levels, but the proportion of participants who had intermediate levels was high (26.2% in males and 19.1% in females). Higher prevalence of ideal blood glucose levels was noted in participants who live in the south region for both sexes.
The proportions of ideal BMI and BP levels in the total population and in subgroups became higher, whereas the proportions of poor levels became lower when using Chinese references (Supplementary eTable 3).
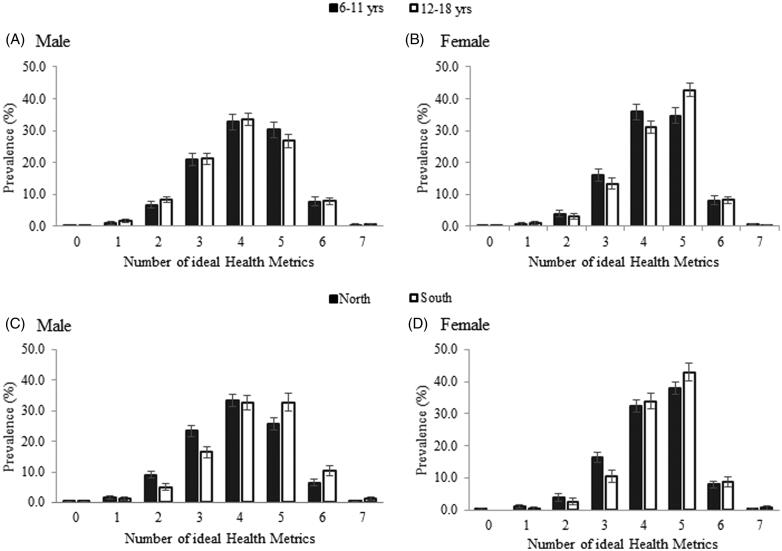
Table 2 and Figure 2 present the distributions of numbers of ideal health metrics in the total population and by sex, age and region. The majority of urban Chinese children and adolescents had 3–5 ideal metrics, accounting for 84.8% of the whole population. A very low proportion (0.5%) had all 7 ideal health metrics in the whole population (0.5% in males and 0.4% in females). In addition, about 42% had ≥5 ideal health components, with a higher proportion of ≥5 ideal health components observed in females compared with males (49.3 versus 35.8%). In females, participants aged 12–18 years versus aged 6–11 years had a higher proportion of ≥5 ideal health components compared (51.2% versus 43.5%); however, the difference was not observed in males (35.3% versus 38.5%). Individuals who lived in the southern region had higher proportions of ≥5 ideal health components compared with those who lived in the north region for both males (44.4% versus 32.4%) and females (52.3% versus 46.1%). When the numbers of ideal health behaviours and health factors were separately analyzed, 44.2% of urban Chinese children and adolescents had all 3 ideal health factors, with females reporting a higher proportion (50.5% versus 38.4%). In contrast, only 0.9% had all 4 ideal health behaviours and males had a higher proportion (1.1% versus 0.7%). The proportions of numbers of ideal health metrics almost did not change when using Chinese references to calculate BMI and BP percentiles (Supplementary eTable 4).
Table 2.
Proportions (standard errors) of numbers of ideal cardiovascular health metrics, Ideal health behaviours, and ideal health factors according to sex in urban Chinese children and adolescents aged 6–18 years in 2013–2015.
| Overall | Sex |
pa | ||
|---|---|---|---|---|
| Males | Females | |||
| Number of ideal health components | (n = 7484) | (n = 3992) | (n = 3492) | |
| 0 | 0.1 (0.1) | 0.2 (0.1) | 0.1 (0.1) | <.001 |
| 1 | 1.2 (0.1) | 1.5 (0.1) | 0.9 (0.1) | |
| 2 | 5.6 (0.3) | 7.8 (0.5) | 3.2 (0.3) | |
| 3 | 17.8 (0.5) | 21.3 (0.8) | 14.0 (0.6) | |
| 4 | 33.1 (0.7) | 33.5 (1.0) | 32.7 (1.0) | |
| 5 | 34.0 (0.7) | 27.8 (0.7) | 40.7 (1.1) | |
| 6 | 7.8 (0.3) | 7.5 (0.4) | 8.2 (0.5) | |
| 7 | 0.5 (0.1) | 0.5 (0.1) | 0.4 (0.1) | |
| Number of ideal health behaviours | (n = 7514) | (n = 4009) | (n = 3505) | |
| 0 | 1.5 (0.1) | 2.1 (0.1) | 0.8 (0.1) | <.001 |
| 1 | 21.6 (0.6) | 27.5 (0.9) | 15.2 (0.7) | |
| 2 | 60.4 (0.9) | 52.8 (1.2) | 68.6 (1.5) | |
| 3 | 15.6 (0.5) | 16.3 (0.7) | 14.8 (0.7) | |
| 4 | 0.9 (0.1) | 1.1 (0.1) | 0.7 (0.1) | |
| Number of ideal health factors | (n = 12014) | (n = 6103) | (n = 5911) | |
| 0 | 2.0 (0.1) | 2.5 (0.2) | 1.6 (0.2) | <.001 |
| 1 | 14.0 (0.4) | 16.5 (0.6) | 11.2 (0.4) | |
| 2 | 39.8 (0.6) | 42.7 (0.9) | 36.7 (0.8) | |
| 3 | 44.2 (0.6) | 38.4 (0.8) | 50.5 (1.0) | |
Numbers may not add up to 100% due to rounding. ap-values for difference between sex groups adjusting for age.
Figure 2.
Age- and region-specific distributions of numbers of ideal cardiovascular health metrics in males and females.
Discussion
Using the AHA’s concept and definition of seven health metrics, we evaluated the status of cardiovascular health in a representative sample of urban Chinese children and adolescents aged 6–18 years in 2013–2015. China has experienced rapid urbanization over the past three decades, and the urbanization rate will increase to 71% by 2030 [27]. Therefore, understanding cardiovascular health among current urban pediatric population is important for developing effective strategies to prevent cardiovascular events.
Many large epidemiological studies have demonstrated the poor status of cardiovascular health among Chinese adults. Data from a national population-based study (i.e. the China Noncommunicable Disease Surveillance 2010) showed that the estimated percentage of ideal cardiovascular health among Chinese adults aged ≥20 years old was only 0.2% [21]. The Chinese Health Examination Database showed that only 0.6% of male and 2.6% of female adults from Chinese urban areas met all 7 health components [20]. In the present study, only 0.5% of urban Chinese children and adolescents met all 7 ideal health components with only 0.9% having all 4 ideal behaviours. Our findings, together with those in adults, indicate that cardiovascular risk factors and behaviours develop early in life and effective clinical and public health interventions are required to improve cardiovascular health among youths.
It is well documented that unhealthy lifestyle behaviours and obesity lie at the root of many chronic diseases. In our study, ideal diet score (8.7%) was the least prevalent health component, which was consistent with US adolescents [16]. We included fast-food consumption as one diet component due to the increasing consumption of fast foods [28]. Elevated salt intake has been associated with cardiovascular disease [29], and Chinese adults and youths have high salt intake compared with other countries [30]. Lack of information on salt intake in our study might overestimate the prevalence of ideal diet score. Physical inactivity among youths has been shown to contribute to obesity-related diseases. However, only 16.6% of urban Chinese youths met the ideal levels of physical activity, which is consistent with a previous study showing that about 80% of Chinese children had physical inactivity [31]. In contrast, the prevalence of ideal physical activity among US adolescents reached up to 67.0% for boys and 43.5% for girls [16]. Although we found that few children and adolescents smoked, the prevalence of smoking among Chinese adult men is one of the highest in the world and is consistently increasing [32]. Therefore, strengthening tobacco control strategies among children and adolescents are warranted. Also, childhood obesity plays an important role in the development of multiple cardiometabolic risk factors. Although the prevalence of obesity (14.3% for boys and 5.0% for girls) was lower compared to that for US youths [16], it should be noted that childhood obesity rate has risen dramatically over the last two decades in China, and will continue to increase in future [33]. All these findings indicate that substantial clinical and policy efforts targeting unhealthy lifestyles and obesity among urban Chinese children and adolescents are urgently required.
In parallel with the epidemic of unhealthy lifestyles and obesity in childhood, other health factors are also worsening. The prevalence of elevated BP in childhood increased from 6.9% in 1991 to 10.7% in 2011; the latter was comparable to that in our study (11.1%) [33]. A prior study of 20,191 Chinese children and adolescents aged 7–16 years from 6 representative geographical areas reported that the prevalence of dyslipidemia was 5.4% for high TC [34]. Although only 0.6% of urban Chinese children and adolescents had poor levels of blood glucose, it should be noted that 22.9% of youths had impaired fasting glucose in our study. It is projected that the prevalence of adverse levels of these cardiovascular risk factors among Chinese children and adolescents would continue to increase without effective interventions targeting unhealthy lifestyles and obesity.
Exposure to cardiovascular risk factors in childhood may cause permanent adverse effects on adult health [14]. Therefore, it is important to implement the life course approach by maintaining ideal cardiovascular health from childhood to adulthood and beyond. The definition of cardiovascular health by AHA emphasizes prevention of adverse levels of health behaviours and factors (i.e. primordial prevention) early in life rather than addressing or treating risk factors later in adulthood (i.e. primary prevention)[4]. Both individual-level and population-based primordial prevention strategies are urgently needed to optimize ideal cardiovascular health across the life course.
To our knowledge, this is the first study reporting the prevalence estimate of ideal cardiovascular health among Chinese urban children and adolescents. However, our study has several limitations. First, the participants in the present study were all from urban areas, and thus the status of cardiovascular health from rural areas needs to be investigated in future. Previous studies have shown that youths from rural areas have lower prevalence of overweight/obesity and elevated BP compared to those from the urban areas [35]. Second, diet information was collected using a self-administered food frequency questionnaire, which was not as accurate as that using multiple 24-h dietary recalls. In addition, information on physical activity was also collected using self-administered questionnaire; however, more accurate tool, such as accelerometer, is available though it may be costly for large survey because it provides an objective measure of a child’s participation in physical activity across the entire range of physical activity intensities. Third, information on consumption of sodium and whole grains was not recorded. Consumption of bean-/dairy-products and fried/western fast foods is very popular among Chinese children and adolescents, and both have been reported to be associated with cardiovascular health[36,37], and thus we added these two items to replace whole grain and salt into the diet metrics. Finally, cut-off points for some health metrics, including BMI and BP, were defined based on percentiles from the general population, which pose challenges to the accurate identification of children at risk. Further studies are required to define these cut-points in children with reference to adult cardiovascular endpoints.
In conclusion, the prevalence of ideal cardiovascular health in urban Chinese children and adolescents is extremely low. Effective public health interventions are required to improve overall cardiovascular health in children and adolescents to reduce future CVD risk.
Supplementary Material
Disclosure statement
The authors have no relevant conflicts of interest to disclose.
References
- 1.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou M, Wang H, Zhu J, et al. . Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Cardiovascular Disease C Report on Cardiovascular Diseases in china. Beijing: Encyclopedia of China Publishing House; 2014. [Google Scholar]
- 4.Lloyd-Jones DM, Hong Y, Labarthe D, et al. . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 5.Berenson GS, Srinivasan SR, Bao W, et al. . Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. [DOI] [PubMed] [Google Scholar]
- 6.Bayer O, Krüger H, von KR, et al. . Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity. 2011;19:1069–1076. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magnussen CG, Raitakari OT, Thomson R, et al. . Utility of currently recommended pediatric dyslipidemia classifications in predicting dyslipidemia in adulthood: evidence from the Childhood Determinants of Adult Health (CDAH) study, Cardiovascular Risk in Young Finns Study, and Bogalusa Heart Study. Circulation. 2008;117:32–42. [DOI] [PubMed] [Google Scholar]
- 9.Telama R, Yang X, Viikari J, et al. . Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med. 2005;28:267–273. [DOI] [PubMed] [Google Scholar]
- 10.Craigie AM, Lake AA, Kelly SA, et al. . Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas. 2011;70:266–284. [DOI] [PubMed] [Google Scholar]
- 11.Juonala M, Magnussen CG, Berenson GS, et al. . Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. [DOI] [PubMed] [Google Scholar]
- 12.Juhola J, Magnussen CG, Berenson GS, et al. . Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation. 2013;128:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magnussen CG, Venn A, Thomson R, et al. . The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol. 2009;53:860–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laitinen TT, Pahkala K, Magnussen CG, et al. . Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2012;125:1971–1978. [DOI] [PubMed] [Google Scholar]
- 15.Shay CM, Ning H, Allen NB, et al. . Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003-2008. Circulation. 2012;125:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shay CM, Ning H, Daniels SR, et al. . Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005-2010. Circulation. 2013;127:1369–1376. [DOI] [PubMed] [Google Scholar]
- 17.Ning H, Labarthe DR, Shay CM, et al. . Status of cardiovascular health in US children up to 11 years of age: the National Health and Nutrition Examination Surveys 2003-2010. Circ Cardiovasc Qual Outcomes. 2015;8:164–171. [DOI] [PubMed] [Google Scholar]
- 18.Wu S, Huang Z, Yang X, et al. . Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5:487–493. [DOI] [PubMed] [Google Scholar]
- 19.Zeng Q, Dong SY, Song ZY, et al. . Ideal cardiovascular health in Chinese urban population. Int J Cardiol. 2013;167:2311–2317. [DOI] [PubMed] [Google Scholar]
- 20.Wu HY, Sun ZH, Cao DP, et al. . Cardiovascular health status in Chinese adults in urban areas: analysis of the Chinese Health Examination Database 2010. Int J Cardiol. 2013;168:760–764. [DOI] [PubMed] [Google Scholar]
- 21.Bi Y, Jiang Y, He J, et al. . Status of cardiovascular health in Chinese adults. J Am Coll Cardiol. 2015;65:1013–1025. [DOI] [PubMed] [Google Scholar]
- 22.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. . CDC growth charts: United States. Adv Data 2000;314:1–27. [PubMed] [Google Scholar]
- 23.Ji CY Report on childhood obesity in China (1)–body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed Environ Sci. 2005;18:390–400. [PubMed] [Google Scholar]
- 24.Meng L, Hou D, Shan X, et al. . Accuracy evaluation of omron HEM-7012 electronic sphygmomanometers in measuring blood pressure of children and adolescents. Chin J Hypertens. 2013;21:158–162. [Google Scholar]
- 25.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 26.Jie M, Tianyou W, Linghui M, et al. . Development of blood pressure reference standards for Chinese children and adolescents. Chin J Evid-Based Pediatr. 2010;5:4–14. [Google Scholar]
- 27.NBSC. National statistics yearbook. Beijing: National Bureau of Statistics of China; 2017. [Google Scholar]
- 28.Wang Z, Zhai F, Zhang B, et al. . Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr. 2012;21:253–262. [PMC free article] [PubMed] [Google Scholar]
- 29.Mozaffarian D, Fahimi S, Singh GM, et al. . Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. [DOI] [PubMed] [Google Scholar]
- 30.Hipgrave DB, Chang S, Li X, et al. . Salt and sodium intake in China. JAMA. 2016;315:703–705. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y, Zheng Z, Yi J, et al. . Associations between physical inactivity and sedentary behaviors among adolescents in 10 cities in China. BMC Public Health. 2014;14:744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang G, Wang Y, Wu Y, et al. . The road to effective tobacco control in China. Lancet. 2015;385:1019–1028. [DOI] [PubMed] [Google Scholar]
- 33.Yan W, Li X, Zhang Y, et al. . Reevaluate secular trends of body size measurements and prevalence of hypertension among Chinese children and adolescents in past two decades. J Hypertens. 2016;34:2337–2343. [DOI] [PubMed] [Google Scholar]
- 34.Zhu JF, Liang L, Fu JF, et al. . Survey on the levels of lipids in school-aged children of Beijing, Tianjin, Hangzhou, Shanghai, Chongqing and Nanning cities. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33:1005–1009. [PubMed] [Google Scholar]
- 35.Chen TJ, Modin B, Ji CY, et al. . Regional, socioeconomic and urban-rural disparities in child and adolescent obesity in China: a multilevel analysis. Acta Paediatr. 2011;100:1583–1589. [DOI] [PubMed] [Google Scholar]
- 36.He J, Gu D, Wu X, et al. . Effect of soybean protein on blood pressure: a randomized, controlled trial. Ann Intern Med. 2005;143:1–9. [DOI] [PubMed] [Google Scholar]
- 37.Reynolds K, Chin A, Lees KA, et al. . A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol. 2006;98:633–640. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.