Abstract
Objectives:
To determine how commonly medical inpatients with opioid use disorder (OUD) referred for post-acute medical care were rejected due to substance use or treatment with opioid agonist therapy (OAT). Additionally, to assess for changes in rejection rates following the United States Attorney’s May 2018 settlement with a Massachusetts nursing facility for violating anti-discrimination laws for such rejections.
Methods:
We linked electronic referrals to private Massachusetts post-acute medical care facilities from Boston Medical Center in 2018 with clinical data. We included referrals with evidence of OUD using ICD-10 diagnosis codes or OAT receipt. We identified the frequency of referrals where the stated rejection reason was substance use or OAT and classified these as discriminatory. We used segmented regression to assess for changes in proportion of referrals with substance use and OAT-related rejections before and after the settlement.
Results:
In 2018, 219 OUD-associated hospitalizations resulted in 1648 referrals to 285 facilities; 81.8% (1348) were rejected. Among hospitalizations, 37.4% (82) received at least one discriminatory rejection. Among rejections, 15.1% (203) were discriminatory (105 for OAT and 98 for substance use). Among facilities, 29.1% (83) had at least one discriminatory rejection. We found no differences in proportion of discriminatory rejections before and after the settlement.
Conclusions:
Individuals hospitalized with OUD frequently experience explicit discrimination when rejected from post-acute care despite federal and state protections. Efforts are needed to enhance enforcement of anti-discrimination laws, regulations, and policies to ensure access to post-acute medical care for people with OUD and ongoing medical needs.
Keywords: Opioid use disorder, medications for opioid use disorder, post-acute medical care, discrimination, skilled nursing facilities
Introduction:
Massachusetts has been particularly affected by the opioid crisis, with the second highest rate of inpatient hospitalizations related to opioids in the United States following a 201% increase in heroin-related hospitalizations between 2007 and 2014.1,2 These hospitalizations are often for conditions related to OUD and/or injection drug use, such as endocarditis, osteomyelitis, or trauma, that require weeks of ongoing inpatient medical treatment, such as intravenous antibiotics or physical therapy. Extended inpatient medical care provides an opportunity to continue, initiate, and stabilize patients with OUD on opioid agonist therapy (methadone or buprenorphine) or the opioid antagonist, naltrexone.3–6 To complete multiple weeks of inpatient medical rehabilitative care, many inpatients with OUD who would benefit from initiating or continuing OAT are referred to post-acute medical care facilities for ongoing medical, physical therapy, or nursing needs.
In 2016, the Massachusetts Department of Public Health issued statewide guidance to post-acute medical care facilities that individuals treated with OAT who were otherwise eligible for admission should not be rejected due to treatment with OAT.7 Additionally, on May 10, 2018, the U.S. Attorney’s office reached a settlement with Charlwell House, a Massachusetts nursing home, for violating the Americans with Disability Act (ADA) by refusing to accept a patient because of treatment with buprenorphine. The settlement states that screening out individuals with opioid use disorder (OUD) or those treated with OAT in admissions decisions discriminates against those with a disability and violates the ADA.8 On September 16th, 2019, the US Attorney’s office entered into a second settlement for similar violations with Athena Healthcare, which operates 16 nursing facilities in Massachusetts.9
Commentaries, resonating with our clinical experience, have highlighted the challenge of finding post-acute care settings for patients with OUD or treated with OAT. However, we are not aware of any systematic evaluations of facility practices or the proportion of OUD hospitalizations affected by this discrimination.10,11 Boston Medical Center’s (BMC) electronic post-acute care referral system includes data about rejections and frequently includes free-text communications from facilities detailing the reasons for rejections. We hypothesized that among individuals hospitalized with OUD, rejection from post-acute medical care would be common and that facilities would frequently cite substance use or OAT as the reason for rejection, against the policy of state regulators and defined as discrimination under the ADA. It is not known if the U.S. Attorney’s settlement in May 2018, the first to recognize and address these practices as discriminatory, resulted in changes in facility practices across Massachusetts. We hypothesized that following this settlement, fewer referrals would include explicit discriminatory explanations but that the proportion of referrals rejected for patients with OUD would remain unchanged.
Methods:
Study Design and Data Source
We reviewed all electronic referrals from BMC to private Massachusetts post-acute medical care facilities in 2018. Via the Boston Medical Center Clinical Data Warehouse (CDW), we linked these referrals with clinical data associated with these hospitalizations to include only individuals with OUD. We identified referrals where the stated reason for rejection was substance use or OAT, which we classified as discriminatory content based on legal precedent. We used segmented regression to investigate whether the May 2018 U.S. Attorney settlement with a nursing facility was associated with a change in the proportion of referrals that were associated with discriminatory comments and rejections. The Boston University Medical Campus institutional review board approved this study.
Cohort Selection
We included all individuals 18 or older hospitalized with OUD who received at least one electronic referral to a private post-acute care medical facility in Massachusetts through BMC’s electronic referral system in 2018. Referrals to state-funded post-acute care and respite care for homeless individuals were not included in this data. OUD status was determined by the presence of International Classification of Disease, 10 Edition (ICD-10) Codes for OUD (F11.10, F11.11, F11.21, F11.221, F11.23, F11.90) or receipt of buprenorphine or methadone during the hospitalization or at time of discharge. Hospitalizations with methadone receipt were only included if methadone was formulated as a liquid to prevent inclusion of individuals who received methadone for the treatment of chronic pain, which was generally treated with tablets. Although naltrexone can also be used to treat OUD, it was more commonly used for alcohol use disorder in the acute medical hospital and, thus, naltrexone was not used to identify OUD-associated hospitalizations.
Variables of Interest
The primary outcome of interest was presence of substance use or treatment with OAT as a facility’s stated reason for declining admission to post-acute medical care. We defined these rejections as discriminatory. We also sought to identify comments about naltrexone. The electronic referral system allows admissions coordinators to transmit free text comments when a patient is rejected (e.g. question about insurance, clinical needs). As not all rejected referrals included transmitted comments in the electronic referral system, our categorization of discriminatory comments related to substance use or OAT was a specific, but not a sensitive, indication of facility intentions. Two reviewers read and coded all comments to identify and sub-categorize substance use-related content. We categorized comments relating to methadone or buprenorphine as OAT comments. We categorized comments as substance use-related if they referred to alcohol, cocaine, heroin, fentanyl, benzodiazepines, injection drug use (IDU), reference to toxicology, or non-specific substance use. We also recorded as an additional outcome any rejection for any reason, which we defined as any referral which was not accepted in the electronic referral system.
We included several individual characteristics at the hospitalization level which were obtained from the CDW, including age, race, language, intensive care unit (ICU) admission during the hospitalization, insurance status, and primary discharge diagnosis codes, and disposition, which included state-funded and homeless respite facilities. Our physician investigators grouped the primary discharge diagnoses into categories (acute infection, neurology, pulmonary, gastroenterology, trauma, pain, and other) based on clinical judgement.
Statistical Analyses
We calculated the mean, frequency, and proportion of cohort characteristics. We also calculated the frequency and proportion of discriminatory content accompanying rejections at the referral, hospitalization, and facility levels. At the referral level, we classified the rejections by comment category: substance use, OAT (sub-categorized into methadone, buprenorphine, methadone and buprenorphine), naltrexone, or non-substance use. We then divided the study period into 26 two-week intervals. December 31st did not fall evenly into the two-week intervals and was included in the last interval. We then analyzed outcomes in these intervals and divided the study period into two periods: pre-intervention (January 1 through May 6, 2018 or 9 two-week periods) and post-intervention (May 7 through December 31, 2018 or 17 two-week periods). The U.S. Attorney Settlement was May 10, but due to the division of two-week intervals, May 7 through May 9 were classified as part of the post-intervention period. However, this did not result in exposure misclassification as there were no OUD referrals on those dates. We plotted the crude proportion of referrals that were associated with direct evidence of discrimination and proportion of referrals which were rejected from post-acute medical care by two-week interval. We used segmented linear regression to test for changes in the proportions of referrals associated with rejections and with direct evidence of discrimination. Regression models for both outcomes included terms for baseline trend as well as trend and level changes after the intervention. To avoid inclusion of nonsignificant terms that may bias estimated trends, we used backward elimination to select the most parsimonious model, sequentially removing terms with p>0.20 and adjusted for autocorrelation.12 We used SAS, version 9.4 (SAS Institute Inc, Cary, NC, USA) for analyses.
Sensitivity Analysis
To account for a potential lag in the effect of the U.S. Attorney’s settlement on facility practices, we included a sensitivity analysis where the intervention time was changed from May 7, 2018 to July 2, 2018, approximately 8 weeks later.
Results:
There were 219 hospitalizations with evidence of OUD that received at least one referral for post-acute medical care. The cohort was largely white (54.3%), English speaking (92.2%), received OAT in the hospital or on discharge (87.7%), and was insured by Medicaid (53.4%). Acute infections accounted for 46% (100) of hospitalizations; Neurologic (9.2%), pulmonary (7.8%), and other diagnoses (18%) were also common. One hospitalization had no attached diagnosis in the data abstracted from the CDW. Of these hospitalizations, 63.9% ultimately were discharged to a post-acute medical care facility, 17.8% were discharged home without services, 9.1% home with services, 7.3% left the hospital against medical advice, and 1.8% died during the hospitalization (Table 1).
Table 1.
Characteristics of 219 hospitalizations of people with opioid use disorder who were referred to a private post-acute medical care facility in Massachusetts in 2018 from a safety-net hospital
| Characteristic | Value |
|---|---|
| Age, years (mean) | 50.2 |
| Male, % | 71.7 |
| Race/ethnicity | |
| White, % (n) | 54% (119) |
| Black, % (n) | 29% (63) |
| Hispanic/Latino, % (n) | 3.2% (7) |
| Unknown, % (n) | 13%(29) |
| Native American, % (n) | 0.5% (1) |
| Language | |
| English, %(n) | 92% (202) |
| Spanish, % (n) | 7.3% (16) |
| Haitian-Creole, % (n) | 0.46% (1) |
| ICU stay, % (n) | 34.3% (75) |
| OAT, % (n) | 87.7% (192) |
| Insurance | |
| Medicaid, % (n) | 53% (117) |
| Medicare, % (n) | 22% (49) |
| Commercial, % (n) | 15% (32) |
| Worker’s compensation, % (n) | 7.3% (16) |
| Self, % (n) | 1.4% (3) |
| Other, % (n) | 0.9% (2) |
| Primary Diagnosis1 | |
| Infection, % (n) | 46% (100) |
| Other2, % (n) | 18% (39) |
| Neurologic, % (n) | 9.2% (20) |
| Pulmonary, % (n) | 7.8% (17) |
| Pain, % (n) | 6.4% (14) |
| Trauma, % (n) | 5.5% (12) |
| Gastroenterology, % (n) | 5.0% (11) |
| Cancer, % (n) | 2.3% (5) |
| Disposition3 | |
| Post-acute medical care facility | 63.9% (140) |
| Home | 17.8% (39) |
| Home with services | 9.1% (19) |
| Left against medical advice | 7.3% (16) |
| Deceased | 1.8% (4) |
Primary diagnosis was missing for one patient. Percentages are based on those with diagnoses.
Other category includes diagnoses codes without clear etiology (volume status changes, failure to thrive, metabolic abnormalities) as well as renal issues, cardiac arrest, syncope, rhabdomyolysis, and hypothermia.
Data for disposition to post-acute medical care facilities includes disposition to private, public, and respite care for homeless individuals. Referral and acceptance data was not available for these additional facilities.
Discriminatory Content in Facility Rejections
The 219 hospitalizations resulted in 1648 referrals to 285 facilities (an average of 7.5 referrals per hospitalization). Of these referrals, 81.8% (1348) were rejected. Facilities placed any comment in the electronic referral system in 51.9% (699) of rejected referrals, and 15.1% (203) of all rejections included comments related to substance use or OAT. OAT was identified as the reason for rejecting the referral in 105 cases and substance use was specifically identified in 98 referrals (Table 2). Naltrexone was not noted in any comments. In total, 37.4% (82) of OUD hospitalizations were associated with at least one referral rejection that included discriminatory content from a private post-acute care facility. Among Massachusetts private post-acute care facilities receiving at least one referral in this cohort, 29.1% (83) included at least one comment which was classified as discriminatory.
Table 2.
Frequency of direct evidence of discrimination among rejected referrals from private, Massachusetts post-acute medical care facilities in 2018, Boston Medical Center (n=1348 rejected referrals)
| Comment content | |
|---|---|
| OAT, % (n) | 7.8% (105) |
| Buprenorphine, % (n) | 3.0% (38) |
| Methadone, % (n) | 5.0% (65) |
| Buprenorphine and Methadone, % (n) | 0.1% (2) |
| Naltrexone, % (n) | 0% (0) |
| SUD Only, % (n) | 7.3% (98) |
| Total, % (n) | 15.1% (203) |
Effect of U.S. Attorney Settlement
Of the 1648 referrals in our study, 638 referrals (38.7%) occurred during the pre-intervention period (January 1 through May 6, 2018) and 1010 (61.3%) in the post intervention period (May 7 through December 31, 2018). In the pre-intervention period, 80.4% were rejected, and in the post-intervention period, 82.7% were rejected. Regression analyses showed no statistically significant change in proportion of referrals that were rejected or proportion that were explicitly discriminatory following the U.S. Attorney settlement in May, 2018. Terms for pre-intervention time trend and slope and level change following the settlement for both discriminatory comments and overall rejections were removed from the model based on prespecified p-value thresholds. All terms were sequentially removed, suggesting no significant changes (Table 3). The resulting modeled estimates show that throughout the study period, 77.3% of all OUD referrals were rejected (Figure 1) and discriminatory content was included in 11.8% of all OUD referrals throughout the study period (Figure 2).
Table 3.
Segmented linear regression model results with backwards selection1
| a) Discriminatory Comments Model, post-intervention period begins May 12th, 2018 | |||
|---|---|---|---|
| Time | Level Change | Slope Change | |
| Full Model | 1.17 (p=0.2570) | −3.31 (p=0.5837) | −1.37 (p=0.1993) |
| Step 1 | 0.82 (p=0.2693) | −1.13 (p=0.2350) | |
| Step 2 | −0.12 (p=0.6357) | ||
| Step 3 | |||
| Intercept =11.84 when all terms sequentially removed | |||
| b) Rejection Model, post-intervention period begins May 12th, 2018 | |||
| Time | Level Change | Slope Change | |
| Full Model | 1.17 (p=0.5317) | −8.49 (p=0.4641) | −0.96 (p=0.6311) |
| Step 1 | 0.33 (p=0.6123) | −6.25 (p=0.5481) | |
| Step 2 | −1.91 (p=0.7414) | ||
| Step 3 | |||
| Intercept = 77.29 when all terms sequentially removed | |||
Model results are based on proportion of rejected referrals and proportion of rejections with discriminatory comment in 638 referrals divided into 9 two-week periods before the Settlement and 1010 referrals divided into 17 two-week periods after the Settlement.
Figure 1:
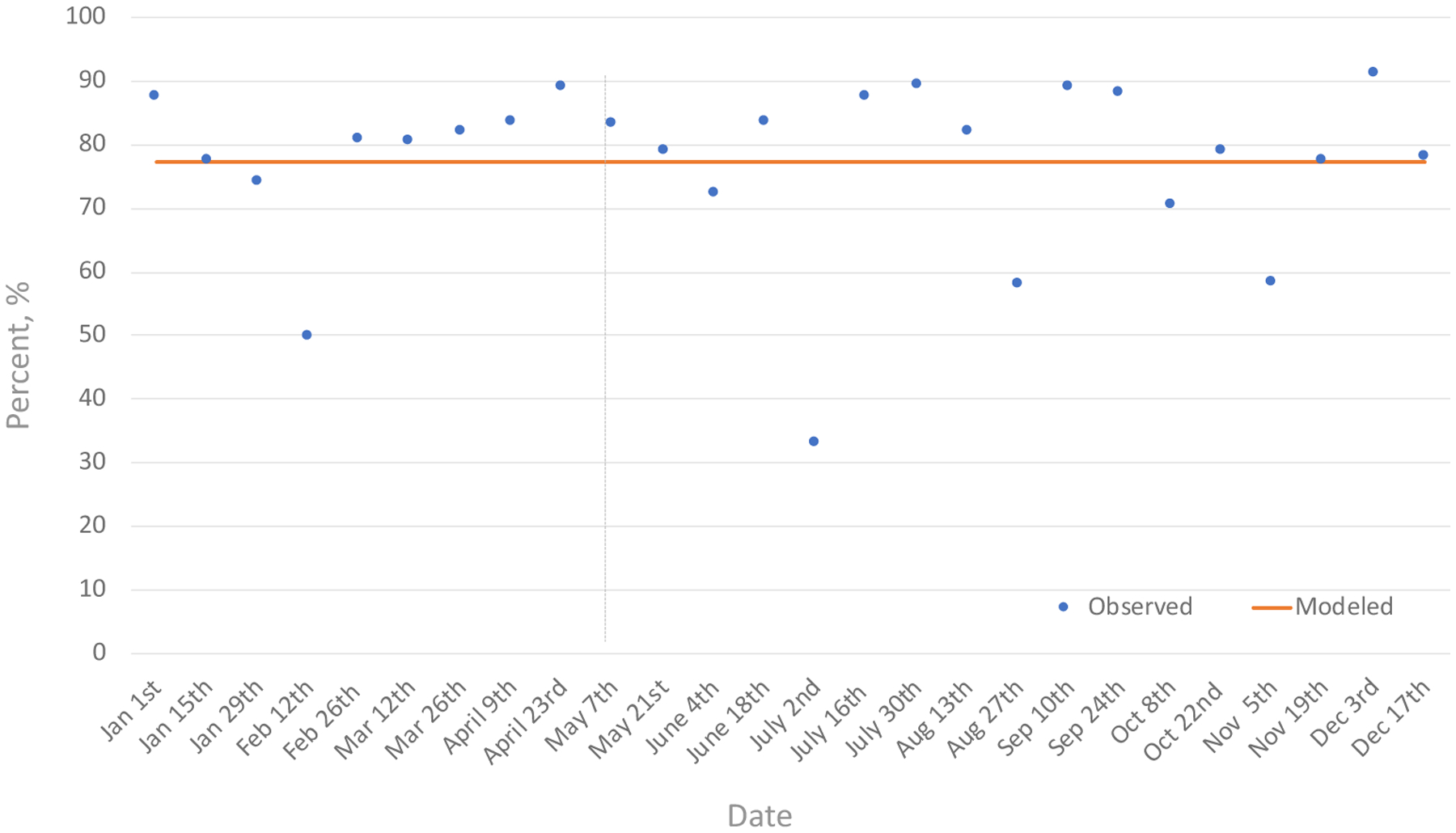
Proportion of post-acute care referrals rejected in 2018 for patients with opioid use disorder before and after a U.S. Attorney Settlement
1 Study sample includes 1648 referrals to 285 facilities
Figure 2:
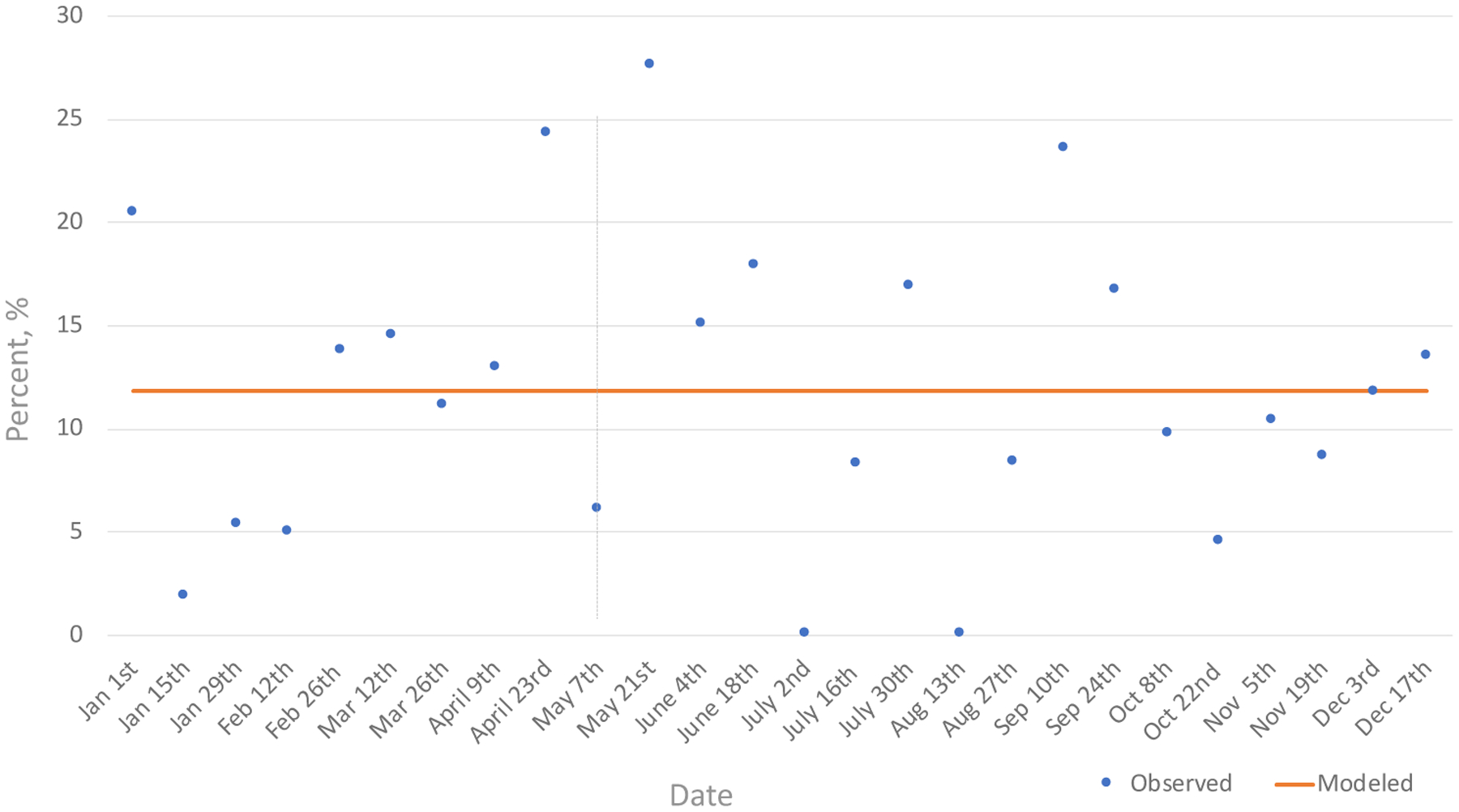
Proportion of post-acute care referrals with discriminatory communications in 2018 for patients with opioid use disorder before and after a U.S. Attorney Settlement
Sensitivity Analysis:
There were no substantive differences in the results when a lag was included, and the intervention time was changed to July 2nd, 2018 (Supplemental Table 1).
Discussion:
Nearly 4 out of 10 individuals hospitalized with OUD who were referred for post-acute medical care were explicitly rejected admission to private facilities due to the presence of substance use or OAT. Despite being classified as discriminatory under the federal ADA and unequivocally prohibited by state regulation, explicit discrimination due to substance use and receipt of OAT is widespread. However, no referrals were explicitly rejected due to naltrexone. Examining referrals from one safety-net academic medical center alone, we identified 83 (29.1%) private Massachusetts facilities that provided explicitly discriminatory reasons for rejecting patients. Despite indications for post-acute medical care, 8 in 10 referrals resulted in a rejection and only 2 in 3 individuals referred for post-acute medical care were ultimately discharged to a post-acute medical care facility, including state-funded or homeless respite facilities. Patients who are not accepted into post-acute care may ultimately be denied necessary medical treatments, wound care, or physical or occupational therapy. Failing to provide these services may exacerbate the stigma people who use drugs experience in the healthcare system.10,13,14 Moreover, increased effort to find post-acute care and potentially longer inpatient hospitalizations may result in resentment among hospital staff toward patients with OUD. Amidst the current opioid crisis, which is driving both surges in overdose deaths and morbidity due to medical complications, the healthcare system must provide high-quality post-acute medical care for people with substance use disorder (SUD), including those treated with OAT. This will require efforts to enhance enforcement of existing regulations and to address barriers to acceptance to post-acute medical care for individuals with SUD.
There are several possible explanations for this systematic discrimination. Facilities and individuals making admissions decisions may harbor stigma against individuals with substance use disorders or toward OAT, biases which may have been formally or informally codified in admissions criteria. Stigma has been demonstrated to impact the care of individuals with OUD in other clinical domains and may operate similarly in post-acute medical care settings.15–19 Additionally, clinical staff at these facilities may lack expertise in treating SUD and administering OAT and, thus, avoid taking on this responsibility and perceived liability. These barriers have been demonstrated when SUD care was first integrated into other general medical settings, such as primary care.20,21 Finally, the policies surrounding OAT administration create specific logistical challenges in accessing and dispensing buprenorphine or methadone. This may be especially true for methadone, which under current regulations requires facility coordination with an opioid treatment program to access methadone. Policies which allow post-acute care facilities to dispense methadone directly, as is already done in acute care hospitals, may ease this barrier.11 To administer buprenorphine, post-acute care facilities must either maintain their own buprenorphine waivered provider or develop relationships with an outpatient prescriber from the referring hospital or elsewhere.11 Policies that ease the prescriber training requirements for buprenorphine may address this barrier.22 The ADA requires facilities to address these barriers and the Massachusetts Department of Public Health clarified this responsibility to facilities in 2016, but in the absence of significant scrutiny of their practices or sufficient support for implementing changes, facilities may not have changed their historical practices.
Our study also demonstrates that a single settlement enforcing federal ADA regulations alone did not result in facilities substantially increasing acceptances for individuals with OUD referred for care. In fact, rejecting individuals with OUD was so normalized that facilities continued communicating their openly discriminatory conduct to the referring hospital even after the settlement. In addition to increased enforcement targeting direct and covert discriminatory conduct, efforts to increase knowledge about OUD, trainings on providing OAT, and development of workflows to streamline care are necessary. The Massachusetts Department of Public Health funded an effort to provide technical assistance in 2019 with this goal in mind.23
This study has a number of strengths which allow for better understanding of post-acute medical care admission practices and assessment of the degree to which these practices impact clinical care for hospitalized individuals with OUD. First, this is the only study to our knowledge which quantifies these discriminatory practices. Second, we used data from a unique electronic post-acute medical care referral system. We are not aware of other studies which incorporate post-acute care referral-level data. These data allowed for detailed assessments that may not be accessible in administrative or insurance claims data. Additionally, the inclusion of communications associated with facility rejections provides a unique window into post-acute care admissions decisions. These communications are typically intended for hospital case managers and are generally not the subject of additional scrutiny. Third, we increased the rigor of our analysis by employing segmented regression analysis, a quasi-experimental design, to determine if a public settlement resulted in changes in proportion of rejected referrals or inclusion of discriminatory content as a rationale for rejections.
There are a number of limitations to this study. First, this is the experience of a single safety-net hospital in Massachusetts and may not be generalizable. Second, there is incomplete documentation of reasons for rejections in our data source. Not every facility includes a comment for each rejection, and when a comment is included, facilities may state reasons less likely to receive scrutiny (i.e. no bed available), when the underlying reason is diagnosis of SUD or treatment with OAT. Homelessness, which is not protected under the ADA nor state policies in post-acute care admissions decisions, may be noted as the reason for rejection in place of SUD. Discrimination due to homelessness warrants its own investigation. Third, we are unable to account for patterns of referrals by case managers whose referrals may be impacted by their previous experiences with particular facilities. For example, an individual with OUD may be less likely to be referred to a facility that has already stated in previous referrals outside of this study period that they will not be accepted. Furthermore, two state-funded facilities are known to accept patients with OUD or on OAT but are not included in this dataset, and case managers may preferentially refer individuals with SUD or treated with OAT to just those two facilities to increase odds of acceptance and facilitate rapid discharge. In fact, it may be that facilities to which case managers make referrals for individuals with OUD are ones that have been historically more accepting of patients with SUDs. These limitations likely result in our study under-representing the extent to which facilities both directly and covertly discriminate against individuals with OUD or who are treated with OAT. Fourth, due to the small sample and because the primary outcome specification was dependent on facility communication of practices, we did not adjust for important patient factors in the models.
Our results have significant implications for policy makers, health systems leaders, managers of post-acute care facilities, clinicians, case managers, civil rights advocates, and individuals hospitalized with OUD. This study documents normalized discriminatory conduct towards individuals hospitalized with OUD and the failure of a single settlement to change these practices. Discrimination is widespread and ongoing, resulting in poor access to needed healthcare. Enhanced enforcement of state policy and federal law that address barriers to OAT delivery in post-acute medical facilities is urgently needed. Further studies are needed to better understand these barriers (regulatory, technical, behavioral) so that they can be confronted. Amidst the current opioid crisis, it is imperative that the health system provides high quality post-acute medical care for people with SUD, including those treated with OAT.24
Conclusions:
Individuals hospitalized with OUD frequently experience explicit discrimination in post-acute care admissions decisions. A large percentage of post-acute medical care facilities, in direct contradiction of state policy and federal law, directly stated that they reject individuals with OUD or those being treated with OAT. Efforts are needed to enhance legal enforcement and address barriers to acceptance.
Supplementary Material
Acknowledgements:
The authors acknowledge Zoe Weinstein, MD, MSc in the Department of Medicine at Boston Medical Center for her role in identifying and obtaining access to this data source and Gregory Dorchak, JD from the U.S. Attorney’s Office for sharing expertise about the ADA.
Source of support: Dr. Kimmel reports support from the National Institute on Drug Abuse (NIDA) (R25DA013582, R25DA033211), and the National Institute of Allergy and Infectious Diseases (5T32AI052074). He consults for Abt Associates on a Massachusetts Department of Public Health project to expand access to medications for opioid use disorder in post-acute medical care facilities. Ms. Rosenmoss was supported by the Boston University School of Medicine’s Medical Student Summer Research Program. Dr. Bearnot was supported by NIDA (K12DA043490). Dr. Larochelle was supported by NIDA (K23 DA042168) and a Boston University School of Medicine Department of Medicine Career Investment Award. Dr. Walley also reports support from NIDA (R25DA013582) and works as the medical director of the overdose prevention program at the Massachusetts Department of Public Health.
References:
- 1.Weiss AJ, Heslin KC, Barrett ML, Izar R B A. Opioid-Related Inpatient Stays and Emergency Department Visits Among Patients Aged 65 Years and Older, 2010 and 2015. HCUP Statistical Brief #244. 2018. www.hcup-us.ahrq.gov/reports/statbriefs/sb244-Opioid-Inpatient-Stays-ED-Visits-Older-Adults.pdf. Accessed September 24, 2018. [PubMed] [Google Scholar]
- 2.Massachusetts Health Policy Commission. Opioid Use Disorder in Massachusetts: An Analysis of Its Impact on the Health Care System, Availability of Pharmacologic Treatment, and Recommendations for Payment and Care Delivery Reform. Boston, MA; 2016. https://www.mass.gov/files/documents/2016/09/vv/opioid-use-disorder-report.pdf. Accessed July 8, 2019. [Google Scholar]
- 3.Trowbridge P, Weinstein ZM, Kerensky T, et al. Addiction consultation services - Linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat. 2017;79:1–5. doi: 10.1016/j.jsat.2017.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient Addiction Consultation for Hospitalized Patients Increases Post-Discharge Abstinence and Reduces Addiction Severity. J Gen Intern Med. 2017;32(8):909–916. doi: 10.1007/s11606-017-4077-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suzuki J. Medication-assisted treatment for hospitalized patients with intravenous-drug-use related infective endocarditis. Am J Addict. 2016;25(3):191–194. doi: 10.1111/ajad.12349 [DOI] [PubMed] [Google Scholar]
- 6.Aron Mohan AN. Managing Opioid Use Disorder During and After Acute Hospitalization: A Case-Based Review Clarifying Methadone Regulation for Acute Care Settings. J Addict Behav Ther Rehabil. 2015;04(02). doi: 10.4172/2324-9005.1000138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheehan E. Circular Letter: DHCQ 16–11-662. Bureau of Health Care Safety and Quality, Massachusetts Department of Public Health. https://www.mass.gov/circular-letter/circular-letter-dhcq-16-11-662-admission-of-residents-on-medication-assisted#purpose. Published 2016. [Google Scholar]
- 8.U.S. Attorney’s Office vs Charlwell Operating LLC Representative, Charlwell Op. Settlement Agreement between the United States and Charlwell Operating, LLC. https://www.ada.gov/charlwell_sa.html. Published 2018. Accessed July 8, 2019.
- 9.U.S. Attorney’s Office vs Athena Health Care Systems. Settlement Agreement Between the United States of America and Athena Health Care Systems. https://www.ada.gov/athena_healthcare_sa.html. Published 2019.
- 10.Wakeman SE, Rich JD. Barriers to Post-Acute Care for Patients on Opioid Agonist Therapy; An Example of Systematic Stigmatization of Addiction. J Gen Intern Med. 2017;32(1):17–19. doi: 10.1007/s11606-016-3799-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pytell JD, Sharfstein JM, Olsen Y. Facilitating Methadone Use in Hospitals and Skilled Nursing Facilities. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.5731 [DOI] [PubMed] [Google Scholar]
- 12.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x [DOI] [PubMed] [Google Scholar]
- 13.Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–86. doi: 10.1016/j.drugalcdep.2019.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horner G, Daddona J, Burke DJ, Cullinane J, Skeer M, Wurcel AG. “You’re kind of at war with yourself as a nurse”: Perspectives of inpatient nurses on treating people who present with a comorbid opioid use disorder. PLoS One. 2019;14(10). doi: 10.1371/journal.pone.0224335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haffajee RL, Bohnert ASB, Lagisetty PA. Policy Pathways to Address Provider Workforce Barriers to Buprenorphine Treatment. Am J Prev Med. 2018;54(6):S230–S242. doi: 10.1016/J.AMEPRE.2017.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bagley SM, Hadland SE, Carney BL, Saitz R. Addressing Stigma in Medication Treatment of Adolescents With Opioid Use Disorder. J Addict Med. 2017;11(6):415–416. doi: 10.1097/ADM.0000000000000348 [DOI] [PubMed] [Google Scholar]
- 17.Olsen Y, Sharfstein JM. Confronting the Stigma of Opioid Use Disorder—and Its Treatment. JAMA. 2014;311(14):1393. doi: 10.1001/jama.2014.2147 [DOI] [PubMed] [Google Scholar]
- 18.Wakeman SE, Rich JD. Barriers to Post-Acute Care for Patients on Opioid Agonist Therapy; An Example of Systematic Stigmatization of Addiction. J Gen Intern Med. 2017;32(1):17–19. doi: 10.1007/s11606-016-3799-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai AC, Kiang MV., Barnett ML, et al. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLOS Med. 2019;16(11):e1002969. doi: 10.1371/journal.pmed.1002969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beetham T, Saloner B, Wakeman SE, Gaye M, Barnett ML. Access to office-based buprenorphine treatment in areas with high rates of opioid-related mortality: An audit study. Ann Intern Med. 2019;171(1):1–9. doi: 10.7326/M18-3457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wakeman SE, Barnett ML. Primary Care and the Opioid-Overdose Crisis — Buprenorphine Myths and Realities. N Engl J Med. 2018;379(1):1–4. doi: 10.1056/NEJMp1802741 [DOI] [PubMed] [Google Scholar]
- 22.Fiscella K, Wakeman SE, Beletsky L. Buprenorphine Deregulation and Mainstreaming Treatment for Opioid Use Disorder: X the X Waiver. JAMA Psychiatry. 2019;76(3):229–230. doi: 10.1001/jamapsychiatry.2018.3685 [DOI] [PubMed] [Google Scholar]
- 23.Massachusetts Department of Public Health. Medication Assisted Treatment in Long Term Care Technical Support (RFQ 20SPRF610421; CommBuys BID #BD-19–1031-BHCSQ-HCS01–40474). Boston, MA; 2019. https://www.commbuys.com/bso/external/publicContracts.sdo. [Google Scholar]
- 24.Englander H, Wilson T, Collins D, et al. Lessons learned from the implementation of a medically enhanced residential treatment (MERT) model integrating intravenous antibiotics and residential addiction treatment. Subst Abus. 2018;39(2):225–232. doi: 10.1080/08897077.2018.1452326 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


