Abstract
Background
Identification of genetic risk factors that are shared between Alzheimer’s disease (AD) and other traits, i.e., pleiotropy, can help improve our understanding of the etiology of AD and potentially detect new therapeutic targets. Previous epidemiological correlations observed between cardiometabolic traits and AD led us to assess the pleiotropy between these traits.
Methods
We performed a set of bivariate genome-wide association studies coupled with colocalization analysis to identify loci that are shared between AD and eleven cardiometabolic traits. For each of these loci, we performed colocalization with Genotype-Tissue Expression (GTEx) project expression quantitative trait loci (eQTL) to identify candidate causal genes.
Results
We identified three previously unreported pleiotropic trait associations at known AD loci as well as four novel pleiotropic loci. One associated locus was tagged by a low-frequency coding variant in the gene DOCK4 and is potentially implicated in its alternative splicing. Colocalization with GTEx eQTL data identified additional candidate genes for the loci we detected, including ACE, the target of the hypertensive drug class of ACE inhibitors. We found that the allele associated with decreased ACE expression in brain tissue was also associated with increased risk of AD, providing human genetic evidence of a potential increase in AD risk from use of an established anti-hypertensive therapeutic.
Conclusion
Our results support a complex genetic relationship between AD and these cardiometabolic traits, and the candidate causal genes identified suggest that blood pressure and immune response play a role in the pleiotropy between these traits.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-021-00773-z.
Keywords: Pleiotropy, Cardiometabolic traits, Multi-trait GWAS, Colocalization
Background
Studies have consistently found a positive epidemiological correlation between Alzheimer’s disease (AD) and cardiometabolic traits, yet the biological mechanisms behind this correlation is not well understood [1–4]. A leading hypothesis is that this correlation is due to shared genetic influence, or pleiotropy, between AD and cardiometabolic traits [4]. By identifying pleiotropic loci between these traits, we can (i) identify new therapeutic targets or opportunities for drug repurposing, (ii) predict potential side effects, and (iii) better understand the etiology of these complex traits. The identification of new therapeutic targets for AD is of particular importance since AD afflicts approximately 50 million people, and there exist only a handful of therapeutics available for AD that have only limited efficacy in slowing the progression of the disease [5].
Pleiotropy has been an area of both theoretical and empirical study at least since the beginning of the twentieth century [6–8]. However, the topic has received renewed attention, given the pervasiveness of pleiotropy that has been uncovered through genome-wide association studies (GWAS) [8–10]. Recent methods and analysis have sought to characterize the extent of the phenomenon throughout the genome [8], quantifying pairwise genetic correlation across a battery of traits [8, 11], exploiting pleiotropy to perform causal inference in the framework of Mendelian randomization [8, 12], or statistically co-localizing association signals across two or more traits [13, 14]. These methods and publicly available GWAS summary statistics enable studies to dissect the shared genetic etiology between AD and cardiometabolic traits. Due to the epidemiological correlation between AD and cardiometabolic traits, coupled with the fact that many cardiometabolic traits are genetically correlated with one another, additional broader-scale pleiotropic studies are warranted, and recently the field has begun to do so [4, 11].
Statistical methods for detecting pleiotropy use the definition of a single locus associated with two or more traits, and these methods are generally intended to detect loci that have a single genetic variant underlying the shared heritability at the locus. However, recent studies have shown that at some pleiotropic loci there is no shared causal SNP, but instead different SNPs are causal for the different traits. These loci are associated with multiple traits but there is no shared causal genetic variant behind the associations [9, 15]. For this reason, we consider here a more stringent definition of pleiotropy: loci that are associated with two or more traits, and where the statistical data provides evidence of a shared causal genetic variant. We used colocalization analysis to identify which loci appear to share causal genetic variants and which appear to be cases of spurious pleiotropy [8, 13]. There are two models of pleiotropy for this scenario [8]. The first is horizontal pleiotropy, where a genetic variant has a direct effect on two or more traits. The other is vertical pleiotropy, where a genetic variant has a direct effect on a trait and a mediated effect on a second trait through the first trait [8].
In this study, we used summary statistics from the largest publicly available single-trait GWAS to investigate pleiotropy between AD and eleven cardiometabolic traits using the metaMANOVA bivariate GWAS method followed by colocalization analysis [16]. This bivariate GWAS method takes summary statistics for two traits as input and performs a GWAS for the pair of traits, while taking the correlation across association statistics into account [16]. We used this method to perform two different experiments. The first experiment was an “AD-centric” analysis, intended to detect loci that are associated with AD, but previously not shown to be pleiotropic for cardiometabolic traits. We also performed a locus discovery analysis to discover loci that are not previously reported to be associated with either AD or the cardiometabolic trait.
Methods
We performed two bivariate GWAS experiments intended to detect loci that are pleiotropic between AD and cardiometabolic traits. For ease of reproducibility, we first performed a pairwise bivariate GWAS between AD and each of eleven cardiometabolic traits for both experiments. We then assessed whether there was evidence of a shared causal SNP at each bivariate significant locus by performing a colocalization analysis between the AD and cardiometabolic trait signals. To identify candidate causal genes, we performed colocalization analyses between the pleiotropic signals and single-tissue eQTLs from Genotype-Tissue Expression (GTEx) project v7 [13].
Bivariate GWAS
We used the summary statistics from publicly available single-trait GWAS to perform pairwise metaMANOVA bivariate GWAS between AD [17] and the following cardiometabolic traits: coronary heart disease (CHD) [18], type II diabetes (T2D) [19], systolic blood pressure (SBP) [20], diastolic blood pressure (DBP) [20], body mass index (BMI) [21], waist-hip ratio adjusted for BMI (WHRadjBMI) [22], body fat percentage (BFP) [23], total cholesterol (TC) [24], low-density lipoproteins (LDL) [24], high-density lipoproteins (HDL) [24], and triglycerides (TG) [24] (Table 1 and Additional file 1 - Supplementary Table 1; Availability of data and materials). For each of these studies, approval by an institutional review committee was obtained, and all subjects gave informed consent, as documented in each original publication. All bivariate GWAS were performed using the bivariate_scan software [16]. Each bivariate GWAS resulted in a set of independent loci, which we defined as the genomic region that includes all SNPs within 1 MB of the bivariate lead SNP and any other SNPs that are in LD of r2 > 0.2 with the lead SNP using the 1000 Genomes European ancestry cohort (1 kG EUR) [25]. Further detail on our bivariate GWAS pipeline can be found in the Additional file 1 - Supplemental Methods [16].
Table 1.
Single-trait GWAS summary statistics used for bivariate GWAS
| Trait | Publication | PMID | Sample size |
|---|---|---|---|
| AD | Jansen et al. [17] | 30617256 | 71,880 cases, 383,378 controls |
| BFP | Lu et al. [23] | 26833246 | 100,716 |
| BMI | Yengo et al. [21] | 30124842 | 681,275 |
| CHD | Van der Harst et al. [18] | 29212778 | 34,541 cases, 261,984 controls |
| DBP | Evangelou et al. [20] | 30224653 | 1,006,863 |
| HDL | Klarin et al. [24] (EUR samples only) | 30275531 | 404,128 |
| LDL | Klarin et al. [24] (EUR samples only) | 30275531 | 404,128 |
| SBP | Evangelou et al. [20] | 30224653 | 1,006,863 |
| TC | Klarin et al. [24] (EUR samples only) | 30275531 | 404,128 |
| TG | Klarin et al. [24] (EUR samples only) | 30275531 | 404,128 |
| T2D | Mahajan et al. [19] | 30297969 | 80,831 cases, 817,299 controls |
| WHRadjBMI | Pulit et al. [22] | 30239722 | 694,649 |
A list of the traits, original GWAS publication, and sample sizes for each trait used in our analyses
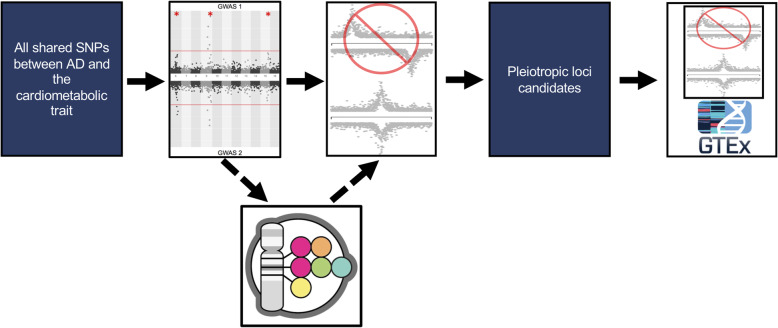
AD-centric analysis
We performed an AD-centric analysis to identify loci that are known to be associated with AD, but not previously known to be pleiotropic for cardiometabolic traits. We first performed pairwise bivariate GWAS between AD and each cardiometabolic trait (Additional file 1 - Supplementary Table 2). To reduce the list of bivariate GWAS genome-wide significant loci results to just the loci that are near genome-wide significantly associated with AD and potentially associated with a cardiometabolic trait, we applied a filter that required loci to have an AD P value < 1 × 10− 6 and a cardiometabolic trait P value < 5 × 10− 3 (Fig. 1).
Fig. 1.
Bivariate GWAS analysis workflow. Starting with all the SNPs that were in both GWAS summary statistics files, we performed a bivariate GWAS and filtered the bivariate significant loci based on their single-trait P values. For the locus discovery experiment, we removed loci that were in LD (1 kG EUR r2 > 0.2) or within 500 kb of a known AD or the cardiometabolic trait being tested according to the GWAS Catalog (dotted line arrows). The filtration steps were followed by trait-trait colocalization to confirm there was evidence of a shared causal SNP between the signals at each locus. Finally, we performed single-tissue-eQTL analysis to identify candidate causal genes for each locus
Locus discovery analysis
To performed a locus discovery analysis, we performed a bivariate GWAS between AD and each cardiometabolic trait (Additional file 1 - Supplementary Table 3). To identify loci that were both pleiotropic and novel, we required the bivariate GWAS lead SNP had r2 < 0.2 in 1 kG EUR and was greater than 500 kb away from all known single-trait associated loci for AD or the cardiometabolic trait being tested, as well as any loci from previous pleiotropic GWAS between the two traits [4, 26]. Additionally, each locus needed to have at least a nominal single-trait association with both traits, so we required an AD P value < 5 × 10− 3 and a cardiometabolic trait P value < 5 × 10− 3 (Fig. 1).
Trait-trait colocalization
We performed colocalization analysis between the AD and the cardiometabolic trait signals given a 500 kb window (± 250 kb) around each locus using COLOC [13]. Our threshold for this analysis was a conditional probability of colocalization (i.e., PP4/ (PP3 + PP4)) ≥ 0.8, which is defined as the posterior probability of colocalization conditioned on the presence of a signal for each trait (Fig. 1). Loci that had a conditional probability of colocalization > 0.45 and < 0.8 were visually inspected using LocusZoom plots, and if the LD structure suggested additional associations unlinked to the leading variant in the region, we performed approximate conditional analysis (see “Approximate conditional analysis,” below) [27]. We excluded loci in the HLA region and near the APOE locus from these experiments due to the difficulty in interpreting the independent contribution of these loci to these traits.
Single-tissue-eQTL colocalization
We performed single-tissue eQTL colocalization analysis to prioritize candidate causal genes implicated by the pleiotropic signals detected in our bivariate GWAS. We collected the list of genes and tissues for which each bivariate GWAS lead SNP was a significant single-tissue eQTL in GTEx v7 from the GTExPortal (Additional file 1 - Supplementary Tables 4–7,9; Additional file 2 -Supplementary Table 8) (data from GTEx as of 02-28-2018, v7) [28]. We then performed colocalization using the AD association data at each locus and each single-tissue eQTL signal from GTEx v7 using a 500-kb window (± 250 kb) around the lead SNP using COLOC [13] (Fig. 1). As above, we considered the AD and eQTL signals to colocalize if the conditional probability of colocalization was ≥ 0.8. We visually inspected the loci where the colocalization analysis resulted in a standard probability of colocalization < 0.8, but conditional probability of colocalization met our criteria [27]. For these loci, we performed approximate conditional analysis, when the LD structure suggested there could be allelic series (see “Approximate conditional analysis,” below).
Approximate conditional analysis
At each locus, we performed approximate conditional analysis on SNPs that appeared to be associated with the trait of interest independently of the lead SNP, because the presence of multiple associated variants in a region violates the assumptions of COLOC and can lead to false positives or false negatives [13]. We identified potential nearby association signals using LocusZoom plots and the LDassoc tool of LDlink [27, 28]. For each locus, we performed approximate conditional analysis using GCTA-COJO with 1000 Genome Project data (European samples, n = 503) as a reference panel [29, 30]. We conditioned our lead SNP on the most associated SNP for each potential confounding signals we identified at the locus. We then repeated the colocalization experiment on the locus using the conditional SNP P values. We provide a full list of traits and loci we performed conditional analysis on, the lead SNP for each analysis, and the SNPs we conditioned on for each analysis are in the supplement (Additional file 1 - Supplementary Table 10).
Results
AD-centric analysis results
We performed an AD-centric analysis to detect known AD loci that were not previously known to be pleiotropic with eleven cardiometabolic traits (“Methods”). We identified a total of 39 independent loci that were bivariate genome-wide significant, met our AD-centric single-trait P value threshold of P value < 1 × 10− 6 and a cardiometabolic trait P value < 5 × 10− 3, and were outside of the HLA and APOE regions (Additional file 1 Supplementary Table 2).
We next performed trait-trait colocalization analysis on all 39 bivariate genome-wide significant loci to identify the subset of loci with evidence of a causal SNP shared in common between the AD signal and the cardiometabolic trait signal. Three loci met our colocalization criteria (Table 2). All of these loci are novel pleiotropic loci between AD and the respective cardiometabolic traits, but have previously been identified as genome-wide significant for AD in recent single-trait AD GWAS [4, 17, 31].
Table 2.
AD-centric analysis pleiotropic loci
| Cardiometabolic trait | Locus name | Lead SNP | Chr | Position GRCh37 | Effect allele/other allele | Direction of effect AD/CM | Effect allele frequency | Bivariate P value | AD P value | Cardiometabolic trait P value | Conditional posterior probability of colocalization | Cardiometabolic GWAS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DBP | ADAM10 | rs442495 | 15 | 59022615 | T/C | +/+ | 0.65 | 1.98e−10 | 1.31e−09 | 9.71e−05 | 0.88 | Evangelou et al. [20] |
| WHRadjBMI | ADAMTS4 | rs4575098 | 1 | 161155392 | A/G | +/+ | 0.22 | 4.45e−13 | 2.05e−10 | 1.99e−06 | 0.87 | Pulit et al. [22] |
| DBP | ACE | rs4308 | 17 | 61559625 | G/A | +/− | 0.63 | 7.05e−15 | 8.52e−07 | 1.00e−16 | 0.98 | Evangelou et al. [20] |
| SBP | rs4308 | 17 | 61559625 | G/A | +/− | 0.63 | 8.01e−15 | 8.52e−07 | 1.00e−16 | 0.98 | Evangelou et al. [20] |
Chr chromosome of the SNP. Direction of effect first position is the direction of effect of the effect allele on AD and the cardiometabolic trait. Effect allele frequency from the Jansen et al. [17] allele frequency. Conditional posterior probability of colocalization, PP4/ (PP3 + PP4) the results of the trait-trait colocalization analysis
To identify candidate causal genes at these three loci, we performed single-tissue-eQTL colocalization analysis between the AD signal at each locus using eQTLs identified by GTEx (“Methods”). All three pleiotropic signals colocalized with one or more single-tissue eQTL signals (Additional file 1 -Supplementary Table 11), and we describe these loci in more detail below.
We detected a pleiotropic signal between AD and DBP at the ADAM10 locus, discovered as an AD association in Jansen et al. [17] (Additional file 1 - Fig. S1). Previous single-trait GWAS have identified several other cardiometabolic trait associations, including BMI and CHD, near this locus (within a 1-Mb window around the lead SNP), but our colocalization results suggest that these signals are independent of the AD signal at this locus [26]. Single-tissue eQTL colocalization analysis identified a single eQTL for MINDY2 in tibial nerve tissue that met our colocalization threshold (Additional file 1 - Fig. S1 and Supplementary Table 11).
The second pleiotropic signal we detected was at the ADAMTS4 locus between WHRadjBMI and AD, also discovered in Jansen et al. [17] AD GWAS (Additional file 1 - Fig. S2). Single-tissue-eQTL colocalization analysis demonstrated that eQTLs for the gene NDUFS2 across multiple tissues strongly colocalized with this signal (Additional file 1 - Supplementary Table 11). An eQTL for the gene FCER1G in tibial nerve also met our colocalization threshold (Additional file 1 - Supplementary Table 11).
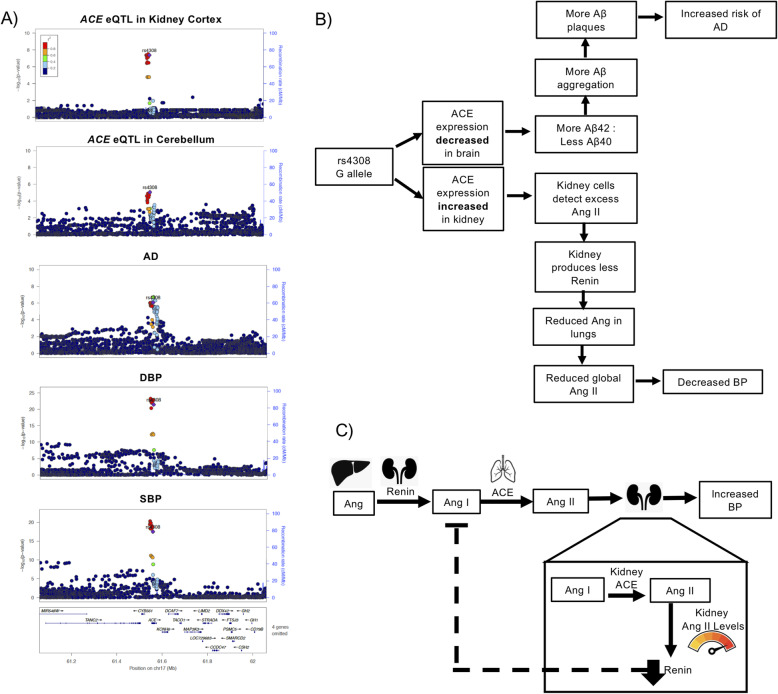
Finally, we detected pleiotropic signals at the ACE locus, which is a known blood pressure and AD association, between both DBP and AD and SBP and AD (Fig. 2a and Tables 2, [20, 31–35]). We noted a direction of effect opposite to the epidemiological correlation for both of these signals, meaning the allele that was associated with reduced risk of AD was associated with increased blood pressure. Our single-tissue eQTL colocalization showed that both pleiotropic signals had strong evidence of colocalization with eQTLs for ACE (Additional file 1 - Supplementary Table 11), but also were opposite directions of effect among different tissues (Additional file 1 - Supplementary Table 11, [36]).
Fig. 2.
ACE locus. a Pleiotropic signal between DBP, SBP, and AD at the ACE locus, and the eQTL signal for ACE in kidney cortex and cerebellum. b Flowchart of our hypothesized mechanism as to how tissue-specific expression of ACE could mediate the blood pressure (BP) and AD pleiotropic signal at this locus. c Diagram of a hypothesized mechanism by which increased kidney expression of ACE could alter renin expression and thus lead to reduce BP through the feedback loops of the renin-angiotensin system
The observed complexity of opposite direction effects at this locus motivated us to further investigate the potential of multiple variants associating with traits and/or eQTLs in the region to confound our colocalization analyses. Here, we performed approximate conditional analyses on the pleiotropic signal lead SNP, rs4308, and the lung ACE eQTL lead SNP, rs4324, in the single-tissue ACE eQTL data for kidney cortex (GTEx v8), lung (GTEx v7), and cerebellum (GTEx v7) (Table 3). The results of this analysis suggested that the ACE eQTL in lung was independent of the ACE eQTLs in the other tissues. These results also support that the ACE eQTLs in kidney and cerebellum share the same causal SNP, which has opposite directions of effect in these tissues (Table 3). Previous studies at this locus observed this same relationship between ACE expression in brain tissue and ACE expression in plasma [33].
Table 3.
Approximate conditional analysis on tissue-specific allelic series in ACE eQTLs
| Tissue of ACE eQTL | P value of rs4308 conditioned on rs4324 | Effect of rs4308 on the ACE eQTL conditioned on rs4324 | P value of rs4324 conditioned on rs4308 | Effect of rs4324 on the ACE eQTL conditioned on rs4308 |
|---|---|---|---|---|
| Lung | 0.15 | 0.048 | 2.57e−08 | 0.18 |
| Cerebellum | 5.34e−04 | − 0.25 | 0.66 | − 0.034 |
| Kidney cortex | 4.41e−08 | 0.49 | 0.21 | − 0.14 |
Approximate conditional analyses performed on the leading single-tissue eQTLs at the ACE locus
We next assessed which ACE eQTLs were most likely to be involved with each of the single-trait signals at this locus, which included the AD, DBP, and SBP signals that we report as pleiotropic as well as a T2D signal that occurred in this region (Additional file 1 - Fig. S3). We performed colocalization analysis of each of the trait signals with the single-tissue ACE eQTLs in kidney cortex, lung, and cerebellum (Table 4). The T2D signal colocalized with the lung ACE eQTL, but not with the kidney and cerebellum ACE eQTLs. The DBP and SBP signals colocalized with the cerebellum and kidney ACE eQTLs, but not the lung ACE eQTL. The AD signal colocalized with all three ACE eQTLs, but the evidence for colocalization was stronger for the cerebellum and kidney ACE eQTLs (Table 4). These results suggest that the blood pressure and AD pleiotropic signals share the same causal SNP that is in high LD with rs4308 and that these associations could be mediated by changes in ACE expression in kidney and brain tissue. However, the T2D signal at this locus appears to be independent of the rs4308 signal and could be mediated by changes in ACE expression in lung tissue.
Table 4.
Tissue-specific ACE eQTL colocalization with GWAS trait signals at the ACE locus
| Tissue of ACE eQTL | Conditional probability of colocalization with AD | Conditional probability of colocalization with T2D | Conditional probability of colocalization with DBP | Conditional probability of colocalization with SBP |
|---|---|---|---|---|
| Lung | 0.89 | 0.96 | 2.73e−04 | 2.72e−04 |
| Cerebellum | 0.95 | 0.58 | 0.98 | 0.97 |
| Kidney cortex | 0.97 | 0.22 | 0.99 | 0.99 |
Conditional Posterior Probability of Colocalization, PP4/ (PP3 + PP4) the results of the colocalization analysis between each trait and ACE eQTL
Locus discovery analysis results
We moved to a broad-scale locus discovery effort using bivariate GWAS to detect novel pleiotropic loci that were not previously associated with AD or the eleven cardiometabolic traits of interest (“Methods”). After applying a battery of filters to identify the subset of loci with positive evidence of pleiotropy and novelty, we were left with thirteen independent loci (Additional file 1 - Supplementary Table 3).
We next performed trait-trait colocalization analysis and found that three of the thirteen independent loci colocalized (Table 5). Thus, there was strong evidence of a shared causal SNP between AD and cardiometabolic traits at these loci. Among the thirteen independent loci was a locus with low-frequency exonic lead SNP with a bivariate P value of 7 × 10− 8. Due to the lead SNP being a low-frequency SNP, it had very little LD with other SNPs, which was not conducive to colocalization analyses (Table 5).
Table 5.
Locus discovery analysis pleiotropic loci
| Cardiometabolic trait | Locus name | Lead SNP | Chr | Position GRCh37 | Effect allele/ other allele | Direction of effect AD/CM | Effect allele frequency | Bivariate P value | AD P value | Cardiometabolic trait P value | Conditional posterior probability of colocalization | Cardiometabolic GWAS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LDL | DOC2A | rs11642612 | 16 | 30030195 | A/C | +/+ | 0.62 | 2.19e−08 | 5.32e−06 | 2.68e−06 | 0.98 | Klarin et al. [24] |
| HDL | SPPL2A | rs12595082 | 15 | 51007729 | C/T | +/+ | 0.81 | 3.27e−08 | 1.66e−06 | 1.09e−05 | 0.95 | Klarin et al. [24] |
| BFP | CCNT2 | rs10496731 | 2 | 135597628 | G/T | +/− | 0.48 | 1.74e−08 | 1.72e−05 | 2.67e−05 | 0.94 | Lu et al. [23] |
| DBP | DOCK4 | rs144867634 | 7 | 111580166 | T/C | +/+ | 0.98 | 8.33e−08 | 5.36e−05 | 1.089e−07 | NA | Evangelou et al. [20] |
Chr chromosome of the SNP. Direction of effect first position is the direction of effect of the effect allele on AD and the cardiometabolic trait. Effect allele frequency from the Jansen et al. [17] allele frequency. Conditional posterior probability of colocalization, PP4/ (PP3 + PP4) the results of the trait-trait colocalization analysis
To identify candidate causal genes, we performed single-tissue-eQTL colocalization analysis at the three loci that were conducive to colocalization analysis. We found that all three loci colocalized with one or more single-tissue eQTL signals from GTEx v7 (Additional file 3 - Supplementary Table 12).
The first novel pleiotropic signal we detected was between LDL and AD at the DOC2A locus (Additional file 1 - Fig. S4). This region has been implicated in other cardiometabolic and neurological traits in previous single-trait GWAS [26]. The lead SNP, rs11642612, is in LD (1 kG EUR r2=0.753) with SNPs that are associated with BMI and schizophrenia [26]. Single-tissue eQTL colocalization found that this pleiotropic signal colocalized with several eQTL signals, but it most strongly colocalized with an eQTL for DOC2A in pancreatic tissue (Additional file 3 - Supplementary Table 12).
The next pleiotropic signal was between AD and HDL at the SPPL2A locus with the lead SNP rs12595082 (Fig. S5). This locus was reported as near genome-wide significantly associated with late-onset AD in Kunkle et al. [31]; however, our bivariate result is the first analysis to detect it at genome-wide significance. This locus was also detected in our AD and DBP bivariate GWAS with the lead SNP rs12440570. Colocalization analysis suggests that the AD, HDL, and DBP association peaks all colocalize with each other (conditional probability of colocalization = 0.81) (Additional file 1 - Supplemental Methods: MOLOC for the SPPL2A locus) [37]. The single-tissue eQTL analysis showed that this signal colocalized with eQTLs for multiple nearby genes (Additional file 3 - Supplementary Table 12).
We detected an opposite direction of effect pleiotropic signal between AD and BFP at the CCNT2 locus (Additional file 1 – Figure S6). Several other neurological and cardiometabolic traits have been associated with this locus [26]. The lead SNP, rs10496731, is in LD with SNPs that are associated with Parkinson’s disease (1 kG EUR r2> 0.378), and DBP (1 kG EUR r2> 0.978) from single-trait GWAS [26]. Single-tissue-eQTL colocalization analysis indicated this signal colocalized with eQTLs for CCNT2 in skin and AC016725.4 in testis (Additional file 3 - Supplementary Table 12).
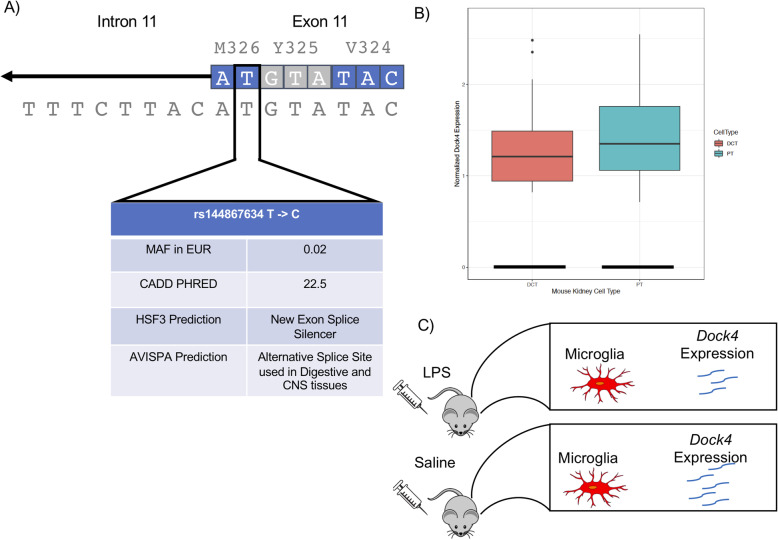
The pleiotropic signal we detected at the DOCK4 locus was between AD and DBP, with rs144867634 as the lead SNP (Fig. 3). rs144867634 is a low-frequency missense variant that is two bases away from the 3′ splice junction of the eleventh exon of DOCK4 (Fig. 3a). This led us to evaluate whether rs144867634 alters the splicing of DOCK4. According to our in silico evaluation of rs144867634’s effect on splicing, it is likely that it alters the splicing of DOCK4, leading to exon 11 being spliced out of the DOCK4 transcript (Fig. 3) (Additional file 1 - Supplemental Methods and Supplementary Tables 13–15).
Fig. 3.
DOCK4 locus. Evidence that supports rs144867634 being the causal variant for the pleiotropic signal at the DOCK4 locus. a In silico evidence that rs144867634 alters DOCK4 splicing. The variant is at the splice junction and is predicted to alter splicing by Human Splice Finder 3 (HSP3) and ASVIPA. b Single-cell mouse kidney data show that Dock4 is expressed by proximal convoluted tubule cells (PT) (128 PT cells of 26,482 assayed have clear evidence of expressing Dock4) and distal convoluted tubule cells (DCT) (27 DCT cells of 8544 assayed have clear evidence of expressing Dock4) (Park et al. 2018). c Mouse brain single-cell data show that Dock4 expression is reduced in microglia when mice have a neuroinflammatory response induced by endotoxin lipopolysaccharide (LPS) injections (Srinvasan et al. 2016)
Discussion
Here, we demonstrate that a bivariate GWAS method coupled with colocalization analysis enabled the detection of pleiotropic loci between these complex traits and identification of plausible causal genes and potential therapeutic targets. We detected three AD-associated loci with previously unknown pleiotropy for cardiometabolic traits and four loci that were pleiotropic and novel for both AD and the pertinent cardiometabolic trait, all of which we were able to map to one or more candidate causal genes. While our manuscript was under consideration, we note that a report was posted which indicated the DOC2A locus is a genome-wide significant AD locus supporting our results [38].
Our findings support those of previous pleiotropy studies between these traits: that there is a complex genetic relationship between AD and cardiometabolic traits involving both vertical and horizontal pleiotropy [4]. Many of the loci suggest a mechanism where AD and cardiometabolic traits have different causal tissues for the two traits. Further evaluation of the loci we reported could aid in predicting the side effects of medications and for drug repurposing for AD and cardiometabolic diseases.
The candidate causal genes we identified through single-tissue-eQTL colocalization analysis support the roles of blood pressure and immune response in both AD and cardiometabolic traits. Three of the pleiotropic loci we report implicate blood pressure mechanisms involved in the pleiotropic relationship at the locus, and four loci had candidate causal genes that have been shown to be involved in immune responses. While these mechanisms make sense given that hypertension and inflammation have both been linked with AD and cardiometabolic diseases, they have not been prevalent in the discussion of pleiotropy between these traits [4, 34, 39–42]. We did not perform experiments to identify causal variants at these loci in this study. However, for some of these loci, previous work has identified plausible causal variants tagged by the pleiotropic signal (e.g., the ALU insertion/deletion at the ACE locus) [32].
The pleiotropic signal at the ACE locus allowed us to shed more light on a locus that is potentially clinically relevant, but complex. ACE is an important enzyme in the renin-angiotensin system, and it is the target gene of ACE inhibitors, a common hypertension medication. This locus has also been well studied from an AD perspective [32, 33, 35]. We found that the allele associated with increased risk of AD and decreased DBP and SBP was associated with decreased ACE expression in brain tissues and most other tissues, but increased ACE expression in transverse colon and kidney (Fig. 2b and Additional file 1 - Supplemental Table 11). These opposite direction of effect single-tissue ACE eQTLs appear to colocalize with one another and be independent of a lung ACE eQTL nearby (Table 3 and Table 4). However, we cannot exclude the possibility of two causal variants that are both in LD (1 kG EUR r2 > 0.8) with the lead SNP of the pleiotropic signal, rs4308.
The decrease in blood pressure could be due to the increase in ACE expression in the kidney and the negative feedback loop between angiotensin II and renin (Fig. 2b,c) [43]. Our hypothesis is that increased expression of ACE in the kidney leads to increased levels of angiotensin II in the kidney. These locally increased levels of angiotensin II lead to reduced expression of renin, slowing the entire renin-angiotensin system, and decreasing blood pressure (Fig. 2c).
In recent years, the relationship between ACE inhibitors and AD has been an active field of study and has resulted in two leading hypotheses of how ACE inhibitors may alter AD risk [34, 39]. Several studies have found that patients on ACE inhibitors that cross the blood-brain barrier (centrally acting) are at reduced risk of dementia and have improved cognitive ability. Other studies have found evidence that patients taking ACE inhibitors have decreased cognitive function and increased levels of β-amyloid (Aβ) protein in their central nervous system; these results were also replicated in mice [40]. This is thought to be due to ACE’s ability to cleave Aβ42 to Aβ40, which is a form of Aβ that is less pathogenic than Aβ42 due to it being less prone to aggregate in the brain [40]. Increases in Aβ42 to Aβ40 ratios have been associated with the PSEN1 and PSEN2 mutations in the familial form of AD [44]. Our results support this second hypothesis, that reduced ACE activity in the brain leads to more Aβ42, which in turn could lead to more Aβ plaques and an increase in AD risk (Fig. 2b). Our findings suggest that further work should be done to evaluate the role of ACE therapeutics for risk of AD.
The BFP and AD pleiotropic signal at the CCNT2 locus has a particularly compelling potential mechanism. Single-tissue-eQTL colocalization analysis detected colocalization between the bivariate signal and an eQTL for CCNT2 in skin tissue (Table 5 and Additional file 1 – Figure S6). The gene CCNT2 is a strong candidate for being involved with both the BFP and the AD association. CCNT2 has been shown to be important in adipose biology [45]. Human CCNT2 knockout adipocytes have altered adipogenesis gene expression and decreased secretion of the hunger inhibiting hormone leptin, which is consistent with increased BFP [45]. CCNT2 has also been shown to be used by herpes simplex virus 1 (HSV-1) when it transcribes its genome [46]. This is a plausible link to AD due to the hypothesis that HSV-1 can trigger amyloid plaques [47, 48].
Finally, our results suggest that DOCK4 is the putative causal gene for the pleiotropic signal between DBP and AD at the DOCK4 locus, since the lead SNP is a low-frequency exonic variant in DOCK4 that is predicted to lead to exon 11 of DOCK4 being spliced out of the DOCK4 transcript (Fig. 3a). For these reasons, and the fact that the rare allele is associated with lower risk of AD and reduced DBP, DOCK4 is our strongest candidate for a novel therapeutic target. The human genetics data observed here is consistent with the simple hypothesis that reduced efficacy of DOCK4 in vivo could treat both hypertension and AD. There is already evidence that DOCK4 could be involved with AD and DBP. Previous genetic studies have shown that DOCK4 variants are associated with multiple neurological phenotypes, and DOCK2, the other member of DOCK4’s protein subfamily, expression is increased in the microglia of patient’s with AD [49, 50]. It has also been shown that Dock4 expression in mouse microglia is altered when mice are given an endotoxin lipopolysaccharide (LPS) injection to induce a neuroinflammatory response (Fig. 3c) [51]. DOCK4 could also affect DBP through changes in kidney function. DOCK4 is expressed in kidney in GTEx v8, and Dock4 is expressed in mouse kidney proximal tubule cells and distal convoluted tubule cells. These cells are responsible for reabsorption of salts, sugars, and amino acids in the nephron of the kidney, and thus altering their function could change blood volume (Fig. 3b) [52, 53].
Limitations
There are several limitations of our study. The Jansen et al. [17] AD GWAS and many of the cardiometabolic trait GWAS we used included individuals from the UK Biobank dataset. This sample overlap will increase the estimated covariance between our traits making the resulting bivariate P value more conservative for a locus that has the same direction of effect as the phenotypic correlation and less conservative when a locus has an opposite direction of effect. The overlapping samples may also inflate our posterior probability of colocalization between these traits. A phenotypic limitation of our study is that it is difficult to differentiate between AD, vascular dementia, and mixed dementia [54]. It is possible that some of the pleiotropic loci we detected are due to vascular or mixed dementia patients being included in this AD cohorts, particular since Jansen et al. include some Proxy-AD patients [17] .
Conclusion
We have shown that bivariate GWAS paired with colocalization analysis can be an effective way to detect pleiotropic loci between complex traits and generate hypotheses as to why these loci are pleiotropic. We detected seven loci that have evidence of being pleiotropic between AD and a cardiometabolic trait, and we were able to identify candidate causal genes for all of these loci. Two loci seem to stand out in their potential to improve our ability to prevent and treat AD. The first is the ACE locus, which provides more evidence to support a potential link between AD risk and ACE inhibitors. The other is the DOCK4 locus which is our most promising candidate for a novel therapeutic target. Our results may aid in resolving the etiology of AD and help identify new therapeutic targets for this disease. AD is a complex disease, and we expect that applying this method to other traits that have been associated with AD, such as educational attainment and immune traits, should also lead to novel pleiotropic loci, new candidate causal genes, and a better understanding of AD [42, 55, 56].
Supplementary Information
Additional file 1: Supplemental Methods – Details on how we collected the GWAS summary statistics and how the statistical analyses were performed. Figure S1. ADAM10 locus – LocusZoom plots of the pleiotropic signals and the MINDY2 eQTL signal at the ADAM10 locus. Figure S2. ADAMTS4 locus – LocusZoom plots of the pleiotropic signals and NDUFS2 eQTL signal at the ADAMTS4 locus. Figure S3. T2D at ACE locus – LocusZoom plots of the T2D signals at the ACE locus. Figure S4. DOC2A locus – LocusZoom plots of the pleiotropic signals and FAM57B and DOC2A eQTL signal at the DOC2A locus. Figure S5. SPPL2A locus – LocusZoom plots of the pleiotropic signals and SPPL2A eQTL signal at the SPPL2A locus. Figure S6. CCNT2 locus – LocusZoom plots of the pleiotropic signals and CCNT2 eQTL signal at the CCNT2 locus. Supplementary Table 1. Bivariate normal estimates for the SNP Z-scores of each bivariate GWAS. Supplementary Table 2. Number of SNPs that passed each filter for the AD-centric analysis. Supplementary Table 3. Number of SNPs that passed each filter for the locus discovery analysis. Supplementary Table 4. Single-tissue eQTLs for rs4308 downloaded from GTExPortal. Supplementary Table 5. Single-tissue eQTLs for rs442495 downloaded from GTExPortal. Supplementary Table 6. Single-tissue eQTLs for rs4575098 downloaded from GTExPortal. Supplementary Table 7. Single-tissue eQTLs for rs10496731 downloaded from GTExPortal. Supplementary Table 9. Single-tissue eQTLs for rs12595082 downloaded from GTExPortal. Supplementary Table 10. List of approximate conditional analyses. Supplementary Table 11. AD-centric bivariate analysis single-tissue-eQTL results. Supplemental Table 13. Human Splice Finder 3 results for rs144867634. Supplemental Table 14. AVISPA results on rs144867634 A allele. Supplemental Table 15. AVISPA results on rs144867634 G allele.
Additional file 2:. Supplemental Table 8. Single-tissue eQTLs for rs11642612 downloaded from GTExPortal.
Additional file 3:. Supplemental Table 12. Locus discovery analysis single-tissue-eQTL results.
Acknowledgements
We want to thank Tiffany R. Bellomo and Jason E. Miller for sharing their medical and phenotypic knowledge.
The VA Million Veteran Program:
Department of Systems Pharmacology and Translational Therapeutics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA, 16Iowa City VA Health Care System, Iowa City, IA, USA, 17VA North Texas Health Care System, Dallas, TX, USA, 18VA Puget Sound Health Care System, Seattle, WA, USA, 19Portland VA Medical Center, Portland, OR, USA, 20VA Connecticut Healthcare System, West Haven, CT, USA, 21Southeast Louisiana Veterans Health Care System, New Orleans, LA, USA, 22Birmingham VA Medical Center, Birmingham, AL, USA, 23VA Southern Nevada Healthcare System, North Las Vegas, NV, USA, 24VA Loma Linda Healthcare System, Loma Linda, CA, USA, 25Miami VA Health Care System, Miami, FL, USA, 26VA Eastern Kansas Health Care System, Leavenworth, KS, USA, 27John D. Dingell VA Medical Center, Detroit, MI, USA, 28Fayetteville VA Medical Center, Fayetteville, AR, USA, 29Richmond VA Medical Center, Richmond, VA, USA, 30Sioux Falls VA Health Care System, Sioux Falls, SD, USA, 31VA San Diego Healthcare System, San Diego, CA, USA, 32Edward Hines Jr. VA Medical Center, Hines, IL, USA, 33Fargo VA Health Care System, Fargo, ND, USA, 34Ralph H. Johnson VA Medical Center, Charleston, SC, USA, 35Cincinnati VA Medical Center, Cincinnati, OH, USA, 36VA Tennessee Valley Healthcare System, Nashville, TN, USA, 37VA Sierra Nevada Health Care System, Reno, NV, USA, 38W.G. (Bill) Hefner VA Medical Center, Salisbury, NC, USA, 39Hampton VA Medical Center, Hampton, VA, USA, 40Eastern Oklahoma VA Health Care System, Muskogee, OK, USA, 41VA Northeast Ohio Healthcare System, Cleveland, OH, USA, 42Philadelphia VA Medical Center, Philadelphia, PA, USA, 43VA Health Care Upstate New York, Albany, NY, USA, 44VA Boston Healthcare System, Boston, MA, USA, 45Louisville VA Medical Center, Louisville, KY, USA, 46Richard Roudebush VA Medical Center, Indianapolis, IN, USA, 47Washington DC VA Medical Center, Washington, D.C., USA, 48James A. Haley Veterans Hospital, Tampa, FL, USA, 49Columbia VA Health Care System, Columbia, SC, USA, 50Central Western Massachusetts Healthcare System, Leeds, MA, USA, 51Bay Pines VA Healthcare System, Bay Pines, FL, USA, 52Southern Arizona VA Health Care System, Tucson, AZ, USA, 53VA Salt Lake City Health Care System, Salt Lake City, UT, USA, 54James H. Quillen VA Medical Center, Johnson City, TN, USA, 55VA Long Beach Healthcare System, Long Beach, CA, USA, 56Minneapolis VA Health Care System, Minneapolis, MN, USA, 57Michael E. DeBakey VA Medical Center, Houston, TX, USA, 58Salem VA Medical Center, Salem, VA, USA, 59Manchester VA Medical Center, Manchester, NH, USA, 60St. Louis VA Health Care System, St. Louis, MO, USA, 61White River Junction VA Medical Center, White River Junction, VT, USA, 62VA Pacific Islands Health Care System, Honolulu, HI, USA, 63Syracuse VA Medical Center, Syracuse, NY, USA, 64Providence VA Medical Center, Providence, RI, USA, 65VA New York Harbor Healthcare System, New York, NY, USA, 66VA Pittsburgh Health Care System, Pittsburgh, PA, USA, 67North Florida / South Georgia Veterans Health System, Gainesville, FL, USA, 68VA Maine Healthcare System, Augusta, ME, USA, 69William S. Middleton Memorial Veterans Hospital, Madison, WI, USA, 70Overton Brooks VA Medical Center, Shreveport, LA, USA, 71New Mexico VA Health Care System, Albuquerque, NM, USA, 72VA Greater Los Angeles Health Care System, Los Angeles, CA, USA, 73Edith Nourse Rogers Memorial VA Hospital, Bedford, MA, USA, 74Clement J. Zablocki VA Medical Center, Milwaukee, WI, USA, 75San Francisco VA Health Care System, San Francisco, CA, USA, 76VA Western New York Healthcare System, Buffalo, NY, USA, 77Northport VA Medical Center, Northport, NY, USA, 78Raymond G. Murphy VA Medical Center, Albuquerque, NM, USA, 79Durham VA Medical Center, Durham, NC, USA, 80Canandaigua VA Medical Center, Canandaigua, NY, USA, 81Phoenix VA Health Care System, Phoenix, AZ, USA, 82South Texas Veterans Health Care System, San Antonio, TX, USA, 83Brigham Women’s Hospital, Boston, MA, USA, 84Harvard Medical School, Boston, MA, USA, 85Atlanta VA Medical Center, Decatur, GA, USA, 86Emory University Rollins School of Public Health, Atlanta, GA, USA, 87Emory University School of Medicine, Atlanta, GA, USA.
Abbreviations
- AD
Alzheimer’s disease
- BMI
Body mass index
- BFP
Body fat percentage
- CHD
Coronary heart disease
- DBP
Diastolic blood pressure
- eQTL
Expression quantitative trait loci
- GTEx
Genotype-Tissue Expression
- GWAS
Genome-wide association study
- HDL
High-density lipoproteins
- LDL
Low-density lipoproteins
- SBP
Systolic blood pressure
- SNP
Single-nucleotide polymorphism
- T2D
Type II diabetes
- TC
Total cholesterol
- TG
Triglycerides
- WHRadjBMI
Waist-hip ratio adjusted for BMI
Authors’ contributions
WB performed, analyzed, and interpreted the multi-trait GWAS and eQTL colocalization results and contributed to writing and editing the manuscript. KS aided in multi-trait GWAS analyses and interpretation and edited the manuscript. AJ performed and interpreted the splicing alteration analyses on the DOCK4 locus and edited the manuscript. SD, DK, KC, PT, and TA contributed to the collection of MVP lipid data as well as writing and editing the manuscript. MD contributed to writing and editing the manuscript and overseeing the project. BV contributed to writing and editing the manuscript, overseeing the project, and conceived of the project. The author(s) read and approved the final manuscript.
Funding
This research is based on data from the Million Veteran Program, Office of Research and Development, Veterans Health Administration, and was supported by the Department of Veterans Affairs Office of R&D award I01-BX003362 (to P.S.T. and K.M.C) and IK2-CX001780 (to S.M.D). This publication does not represent the views of the Department of Veteran Affairs or the United States Government. This work was supported by the American Heart Association (20PRE35120109 to W.P.B.), the National Institutes of Health (DK101478 to B.F.V. and P50GM115318-01 to M.D.R.), and a Linda Pechenik Montague Investigator Award (to B.F.V.).
Availability of data and materials
The software supporting the conclusions of this article are available here:
All code is available under a GNU Public License v3 license:
Language: R (requires version 3.5 or later).
The bivariate GWAS code generated during this study are available at AD_and_Cardiometabolic_Trait_Bivariate_Scans https://github.com/wpbone06/AD_and_Cardiometabolic_Trait_Bivariate_Scans.
The eQTL colocalization code generated during this study are available at GTEx_v7_eQTL_colocalizer https://github.com/wpbone06/GTEx_v7_eQTL_colocalizer.
The datasets supporting the conclusions of this article are available here:
GWAS summary statistics data used in the paper are available at: AD data PMID:30617256 https://ctg.cncr.nl/software/summary_statistics, BFP data PMID:26833246 https://walker05.u.hpc.mssm.edu/, BMI data PMID: 30124842 https://portals.broadinstitute.org/collaboration/giant/index.php/GIANT_consortium_data_files#2018_GIANT_and_UK_BioBank_Meta_Analysis_for_Public_Release, CHD data PMID: 29212778 www.cardiomics.net, DBP data PMID: 30224653, HDL data PMID: 30275531, LDL data PMID: 30275531, SBP data PMID: 30224653, TC data PMID: 30275531, TG data PMID: 30275531, T2D data PMID: 30297969 http://diagram-consortium.org/downloads.html, WHRadjBMI data PMID: 30239722 https://zenodo.org/record/1251813#.XOxslYhKg2w
Access to the MVP lipids data can be obtained from dbGAP (phs001672.v4.p1, pha004828.1, pha004831.1, pha004837.1, pha004834.1) and GLGC European ancestry only data can be obtained at: http://csg.sph.umich.edu/willer/public/lipids/ or http://lipidgenetics.org/.
The GTEx eQTL data used in these analyses are available at: https://www.gtexportal.org/ and https://www.gtexportal.org/home/datasets .
Ethics approval and consent to participate
For each of the studies, we used summary statistics for these analyses, approval by an institutional review committee was obtained, and all subjects gave informed consent, as documented in each original publication.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Benjamin F. Voight, Email: bvoight@pennmedicine.upenn.edu
The VA Million Veteran Program:
Zuhair K. Ballas, Sujata Bhushan, Edward J. Boyko, David M. Cohen, John Concato, Joseph I. Constans, Louis J. Dellitalia, Joseph M. Fayad, Ronald S. Fernando, Hermes J. Florez, Melinda A. Gaddy, Saib S. Gappy, Gretchen Gibson, Michael Godschalk, Jennifer A. Greco, Samir Gupta, Salvador Gutierrez, Kimberly D. Hammer, Mark B. Hamner, John B. Harley, Adriana M. Hung, Mostaqul Huq, Robin A. Hurley, Pran R. Iruvanti, Douglas J. Ivins, Frank J. Jacono, Darshana N. Jhala, Laurence S. Kaminsky, Scott Kinlay, Jon B. Klein, Suthat Liangpunsakul, Jack H. Lichy, Stephen M. Mastorides, Roy O. Mathew, Kristin M. Mattocks, Rachel McArdle, Paul N. Meyer, Laurence J. Meyer, Jonathan P. Moorman, Timothy R. Morgan, Maureen Murdoch, Xuan-Mai T. Nguyen, Olaoluwa O. Okusaga, Kris-Ann K. Oursler, Nora R. Ratcliffe, Michael I. Rauchman, R. Brooks Robey, George W. Ross, Richard J. Servatius, Satish C. Sharma, Scott E. Sherman, Elif Sonel, Peruvemba Sriram, Todd Stapley, Robert T. Striker, Neeraj Tandon, Gerardo Villareal, Agnes S. Wallbom, John M. Wells, Jeffrey C. Whittle, Mary A. Whooley, Junzhe Xu, Shing-Shing Yeh, Michaela Aslan, Jessica V. Brewer, Mary T. Brophy, Todd Connor, Dean P. Argyres, Nhan V. Do, Elizabeth R. Hauser, Donald E. Humphries, Luis E. Selva, Shahpoor Shayan, Brady Stephens, Stacey B. Whitbourne, Hongyu Zhao, Jennifer Moser, Jean C. Beckham, Jim L. Breeling, J. P. Casas Romero, Grant D. Huang, Rachel B. Ramoni, Sumitra Muralidhar, Samuel M. Aguayo, Sunil K. Ahuja, Saiju Pyarajan, Yan V. Sun, Kelly Cho, J. Michael Gaziano, Peter W. Wilson, and Christopher J. O’Donnell
References
- 1.Attems J, Jellinger KA. The overlap between vascular disease and Alzheimer’s disease - lessons from pathology. BMC Med. 2014;12(1):206. doi: 10.1186/s12916-014-0206-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santos CY, Snyder PJ, Wu W-C, Zhang M, Echeverria A, Alber J. Pathophysiologic relationship between Alzheimer’s disease, cerebrovascular disease, and cardiovascular risk: a review and synthesis. Alzheimer’s Dement Diagnosis, Assess Dis Monit. 2017;7:69–87. doi: 10.1016/j.dadm.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reitz C. Dyslipidemia and the risk of Alzheimer’s disease. Curr Atheroscler Rep. 2013;15(3):307. doi: 10.1007/s11883-012-0307-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broce IJ, Chin ·, Tan H, Fan CC, Jansen I, Savage JE, et al. Dissecting the genetic relationship between cardiovascular risk factors and Alzheimer’s disease. Acta Neuropathol. 2018;20. doi: 10.1007/s00401-018-1928-6. [cited 2019 Jan 8] [DOI] [PMC free article] [PubMed]
- 5.Treatments for Alzheimer’s Disease | BrightFocus Foundation. Available from: https://www.brightfocus.org/alzheimers/article/treatments-alzheimers-disease. [cited 2020 Feb 18]
- 6.Stearns FW. One hundred years of pleiotropy: a retrospective. Genetics. 2010;186:767–773. doi: 10.1534/genetics.110.122549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner GP, Zhang J. The pleiotropic structure of the genotype-phenotype map: The evolvability of complex organisms. Nat Rev Genet. 2011;12:204–213. doi: 10.1038/nrg2949. [DOI] [PubMed] [Google Scholar]
- 8.Hackinger S, Zeggini E. Statistical methods to detect pleiotropy in human complex traits. Open Biol. 2017;7(11):170125. doi: 10.1098/rsob.170125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jordan DM, Verbanck M, Do R. HOPS: A quantitative score reveals pervasive horizontal pleiotropy in human genetic variation is driven by extreme polygenicity of human traits and diseases. Genome Biol. 2019;20(1):222. doi: 10.1186/s13059-019-1844-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watanabe K, Stringer S, Frei O, Umićević Mirkov M, de Leeuw C, Polderman TJC, et al. A global overview of pleiotropy and genetic architecture in complex traits. Nat Genet. 2019;51(9):1339–1348. doi: 10.1038/s41588-019-0481-0. [DOI] [PubMed] [Google Scholar]
- 11.Bulik-Sullivan BK, Loh P-R, Finucane HK, Ripke S, Yang J, Patterson N, et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47(3):291–295. doi: 10.1038/ng.3211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7 Available from: https://elifesciences.org/articles/34408. [cited 2018 Aug 29] [DOI] [PMC free article] [PubMed]
- 13.Giambartolomei C, Vukcevic D, Schadt EE, Franke L, Hingorani AD, Wallace C, et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. Williams SM, editor. Plos Genet. 2014;10(5):e1004383. doi: 10.1371/journal.pgen.1004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hormozdiari F, van de Bunt M, Segrè AV, Li X, Joo JWJ, Bilow M, et al. Colocalization of GWAS and eQTL signals detects target genes. Am J Hum Genet. 2016;99(6):1245–1260. doi: 10.1016/j.ajhg.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solovieff N, Cotsapas C, Lee PH, Purcell SM, Smoller JW. Pleiotropy in complex traits: challenges and strategies. Nat Rev Genet. 2013;14:483–495. doi: 10.1038/nrg3461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao SD, Cai TT, Cappola TP, Margulies KB, Li H. Sparse simultaneous signal detection for identifying genetically controlled disease genes. J Am Stat Assoc. 2017;112(519):1032–1046. doi: 10.1080/01621459.2016.1270825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, et al. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51(3):404–413. doi: 10.1038/s41588-018-0311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harst P, van der Verweij N. Identification of 64 novel genetic loci provides an expanded view on the genetic architecture of coronary artery disease. Circ Res. 2018;122(3):433. doi: 10.1161/CIRCRESAHA.117.312086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahajan A, Taliun D, Thurner M, Robertson NR, Torres JM, Rayner NW, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet. 2018;50(11):1505–1513. doi: 10.1038/s41588-018-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50(10):1412–1425. doi: 10.1038/s41588-018-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, et al. Meta-analysis of genome-wide association studies for height and body mass index in ~700 000 individuals of European ancestry. Hum Mol Genet. 2018;27(20):3641–3649. doi: 10.1093/hmg/ddy271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sara PLL. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum Mol Genet. 2019;28(1):166–174. doi: 10.1093/hmg/ddy327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu Y, Day FR, Gustafsson S, Buchkovich ML, Na J, Bataille V, et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. Nat Commun. 2016;7:10495. doi: 10.1038/ncomms10495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klarin D, Damrauer SM, Cho K, Sun YV, Teslovich TM, Honerlaw J, et al. Genetics of blood lipids among ~300,000 multi-ethnic participants of the Million Veteran Program. Nat Genet. 2018;50(11):1514–1523. doi: 10.1038/s41588-018-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MAR, Bender D, et al. PLINK: A tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buniello A, MacArthur JAL, Cerezo M, Harris LW, Hayhurst J, Malangone C, et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 2019;47(D1):D1005–D1012. doi: 10.1093/nar/gky1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pruim RJ, Welch RP, Sanna S, Teslovich TM, Chines PS, Gliedt TP, et al. LocusZoom: regional visualization of genome-wide association scan results. In: Bioinformatics. Oxford England: Oxford University Press; 2011. p. 2336–2337. [DOI] [PMC free article] [PubMed]
- 28.Carithers LJ, Ardlie K, Barcus M, Branton PA, Britton A, Buia SA, et al. A Novel Approach to High-Quality Postmortem Tissue Procurement: The GTEx Project. Biopreserv Biobank [Internet]. 2015;13(5):311–9. Available from: http://www.liebertpub.com/doi/10.1089/bio.2015.0032. [cited 2019 Sep 9] [DOI] [PMC free article] [PubMed]
- 29.Yang J, Lee SH, Goddard ME, Visscher PM. GCTA: a tool for genome-wide complex trait analysis. Am J Hum Genet. 2011;88(1):76–82. doi: 10.1016/j.ajhg.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Altshuler DM, Durbin RM, Abecasis GR, Bentley DR, Chakravarti A, Clark AG, et al. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491(7422):56–65. doi: 10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kunkle BW, Grenier-Boley B, Sims R, Bis JC, Damotte V, Naj AC, et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat Genet. 2019;51(3):414–430. doi: 10.1038/s41588-019-0358-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lehmann DJ, Cortina-Borja M, Warden DR, Smith AD, Sleegers K, Prince JA, et al. Large meta-analysis establishes the ACE insertion-deletion polymorphism as a marker of Alzheimer’s disease. Am J Epidemiol. 2005;162(4):305–317. doi: 10.1093/aje/kwi202. [DOI] [PubMed] [Google Scholar]
- 33.Miners JS, Ashby E, Baig S, Harrison R, Tayler H, Speedy E, et al. Angiotensin-converting enzyme levels and activity in Alzheimer’s disease: differences in brain and CSF ACE and association with ACE1 genotypes. Am J Transl Res. 2009;1(2):163–177. [PMC free article] [PubMed] [Google Scholar]
- 34.Walker VM, Kehoe PG, Martin RM, Davies NM. Repurposing antihypertensive drugs for the prevention of Alzheimer’s disease: a Mendelian randomization study. Int J Epidemiol 2019 ; Available from: http://www.ncbi.nlm.nih.gov/pubmed/31335937. [cited 2020 May 12] [DOI] [PMC free article] [PubMed]
- 35.Kehoe PG, Russ C, McIlroy S, Williams H, Holmans P, Holmes C, et al. Variation in DCP1, encoding ACE, is associated with susceptibility to Alzheimer disease [2] Nat Genet. 1999;21:71–72. doi: 10.1038/5009. [DOI] [PubMed] [Google Scholar]
- 36.Wen X, Luca F, Pique-Regi R. Cross-population joint analysis of eQTLs: fine mapping and functional annotation. Gibson G, editor. Plos Genet. 2015;11(4):e1005176. doi: 10.1371/journal.pgen.1005176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Giambartolomei C, Zhenli Liu J, Zhang W, Hauberg M, Shi H, Boocock J, et al. A Bayesian framework for multiple trait colocalization from summary association statistics. Berger B, editor. Bioinformatics. 2018;34(15):2538–2545. doi: 10.1093/bioinformatics/bty147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bellenguez C, Küçükali F, Jansen I, Andrade V, Morenau-Grau S, Amin N, et al. Large meta-analysis of genome-wide association studies expands knowledge of the genetic etiology of Alzheimer’s disease and highlights potential translational opportunities. medRxiv. 2020
- 39.Jochemsen HM, Teunissen CE, Ashby EL, Van Der Flier WM, Jones RE, Geerlings MI, et al. The association of angiotensin-converting enzyme with biomarkers for Alzheimer’s disease. Alzheimers Res Ther. 2014;6(3):27. doi: 10.1186/alzrt257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu S, Ando F, Fujita Y, Liu J, Maeda T, Shen X, et al. A clinical dose of angiotensin-converting enzyme (ACE) inhibitor and heterozygous ACE deletion exacerbate Alzheimer’s disease pathology in mice. J Biol Chem. 2019;294(25):9760–9770. doi: 10.1074/jbc.RA118.006420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heneka MT, Golenbock DT, Latz E. Innate immunity in Alzheimer’s disease. Nat Immunol. 2015;16:229–36. doi: 10.1038/ni.3102. [DOI] [PubMed] [Google Scholar]
- 43.Neubauer B, Schrankl J, Steppan D, Neubauer K, Sequeira-Lopez ML, Pan L, et al. Angiotensin II short-loop feedback: Is there a role of Ang II for the regulation of the renin system in vivo? Hypertension. 2018;71(6):1075–1082. doi: 10.1161/HYPERTENSIONAHA.117.10357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chévez-Gutiérrez L, Bammens L, Benilova I, Vandersteen A, Benurwar M, Borgers M, et al. The mechanism of γ-Secretase dysfunction in familial Alzheimer disease. EMBO J. 2012;31(10):2261–2274. doi: 10.1038/emboj.2012.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Broholm C, Olsson AH, Perfilyev A, Hansen NS, Schrölkamp M, Strasko KS, et al. Epigenetic programming of adipose-derived stem cells in low birthweight individuals. Diabetologia. 2016;59(12):2664–2673. doi: 10.1007/s00125-016-4099-9. [DOI] [PubMed] [Google Scholar]
- 46.Wu WJ, Yu X, Li WZ, Guo L, Liu LD, Wang LC, et al. HSV-1 stimulation-related protein HSRG1 inhibits viral gene transcriptional elongation by interacting with Cyclin T2. Sci China Life Sci. 2011;54(4):359–365. doi: 10.1007/s11427-011-4160-3. [DOI] [PubMed] [Google Scholar]
- 47.Piacentini R, De Chiara G, Domenica DLP, Ripoli C, Marcocci ME, Garaci E, et al. HSV-1 and Alzheimer’s disease: more than a hypothesis. Front Pharmacol. 2014;5:97. doi: 10.3389/fphar.2014.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wozniak M, Mee AP, Itzhaki RF. Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. J Pathol. 2009;217(1):131–138. doi: 10.1002/path.2449. [DOI] [PubMed] [Google Scholar]
- 49.Chen Q, Kimura H, Schubert D. A novel mechanism for the regulation of amyloid precursor protein metabolism. J Cell Biol. 2002;158(1):79–89. doi: 10.1083/jcb.200110151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shi L. Dock protein family in brain development and neurological disease. Commun Integr Biol. 2013;6(6):e26839. doi: 10.4161/cib.26839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Srinivasan K, Friedman BA, Larson JL, Lauffer BE, Goldstein LD, Appling LL, et al. Untangling the brain’s neuroinflammatory and neurodegenerative transcriptional responses. Nat Commun. 2016;7(1):11295. doi: 10.1038/ncomms11295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carithers LJ, Ardlie K, Barcus M, Branton PA, Britton A, Buia SA, et al. A novel approach to high-quality postmortem tissue procurement: The GTEx Project. Biopreserv Biobank. 2015;13(5):311–319. doi: 10.1089/bio.2015.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Park J, Shrestha R, Qiu C, Kondo A, Huang S, Werth M, et al. Single-cell transcriptomics of the mouse kidney reveals potential cellular targets of kidney disease. Science. 2018;360(6390):758–763. doi: 10.1126/science.aar2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ravona-Springer R, Davidson M, Noy S. Is the distinction between Alzheimer’s disease and vascular dementia possible and relevant? Dialogues Clin Neurosci. 2003;5(1):7–15. doi: 10.31887/DCNS.2003.5.1/rravonaspringer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thome AD, Faridar A, Beers DR, Thonhoff JR, Zhao W, Wen S, et al. Functional alterations of myeloid cells during the course of Alzheimer’s disease. Mol Neurodegener. 2018;13(1):61. doi: 10.1186/s13024-018-0293-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Frost GR, Jonas LA, Li YM. Friend, foe or both? Immune activity in Alzheimer’s disease. Front Aging Neurosci. 2019;11:337. doi: 10.3389/fnagi.2019.00337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Methods – Details on how we collected the GWAS summary statistics and how the statistical analyses were performed. Figure S1. ADAM10 locus – LocusZoom plots of the pleiotropic signals and the MINDY2 eQTL signal at the ADAM10 locus. Figure S2. ADAMTS4 locus – LocusZoom plots of the pleiotropic signals and NDUFS2 eQTL signal at the ADAMTS4 locus. Figure S3. T2D at ACE locus – LocusZoom plots of the T2D signals at the ACE locus. Figure S4. DOC2A locus – LocusZoom plots of the pleiotropic signals and FAM57B and DOC2A eQTL signal at the DOC2A locus. Figure S5. SPPL2A locus – LocusZoom plots of the pleiotropic signals and SPPL2A eQTL signal at the SPPL2A locus. Figure S6. CCNT2 locus – LocusZoom plots of the pleiotropic signals and CCNT2 eQTL signal at the CCNT2 locus. Supplementary Table 1. Bivariate normal estimates for the SNP Z-scores of each bivariate GWAS. Supplementary Table 2. Number of SNPs that passed each filter for the AD-centric analysis. Supplementary Table 3. Number of SNPs that passed each filter for the locus discovery analysis. Supplementary Table 4. Single-tissue eQTLs for rs4308 downloaded from GTExPortal. Supplementary Table 5. Single-tissue eQTLs for rs442495 downloaded from GTExPortal. Supplementary Table 6. Single-tissue eQTLs for rs4575098 downloaded from GTExPortal. Supplementary Table 7. Single-tissue eQTLs for rs10496731 downloaded from GTExPortal. Supplementary Table 9. Single-tissue eQTLs for rs12595082 downloaded from GTExPortal. Supplementary Table 10. List of approximate conditional analyses. Supplementary Table 11. AD-centric bivariate analysis single-tissue-eQTL results. Supplemental Table 13. Human Splice Finder 3 results for rs144867634. Supplemental Table 14. AVISPA results on rs144867634 A allele. Supplemental Table 15. AVISPA results on rs144867634 G allele.
Additional file 2:. Supplemental Table 8. Single-tissue eQTLs for rs11642612 downloaded from GTExPortal.
Additional file 3:. Supplemental Table 12. Locus discovery analysis single-tissue-eQTL results.
Data Availability Statement
The software supporting the conclusions of this article are available here:
All code is available under a GNU Public License v3 license:
Language: R (requires version 3.5 or later).
The bivariate GWAS code generated during this study are available at AD_and_Cardiometabolic_Trait_Bivariate_Scans https://github.com/wpbone06/AD_and_Cardiometabolic_Trait_Bivariate_Scans.
The eQTL colocalization code generated during this study are available at GTEx_v7_eQTL_colocalizer https://github.com/wpbone06/GTEx_v7_eQTL_colocalizer.
The datasets supporting the conclusions of this article are available here:
GWAS summary statistics data used in the paper are available at: AD data PMID:30617256 https://ctg.cncr.nl/software/summary_statistics, BFP data PMID:26833246 https://walker05.u.hpc.mssm.edu/, BMI data PMID: 30124842 https://portals.broadinstitute.org/collaboration/giant/index.php/GIANT_consortium_data_files#2018_GIANT_and_UK_BioBank_Meta_Analysis_for_Public_Release, CHD data PMID: 29212778 www.cardiomics.net, DBP data PMID: 30224653, HDL data PMID: 30275531, LDL data PMID: 30275531, SBP data PMID: 30224653, TC data PMID: 30275531, TG data PMID: 30275531, T2D data PMID: 30297969 http://diagram-consortium.org/downloads.html, WHRadjBMI data PMID: 30239722 https://zenodo.org/record/1251813#.XOxslYhKg2w
Access to the MVP lipids data can be obtained from dbGAP (phs001672.v4.p1, pha004828.1, pha004831.1, pha004837.1, pha004834.1) and GLGC European ancestry only data can be obtained at: http://csg.sph.umich.edu/willer/public/lipids/ or http://lipidgenetics.org/.
The GTEx eQTL data used in these analyses are available at: https://www.gtexportal.org/ and https://www.gtexportal.org/home/datasets .