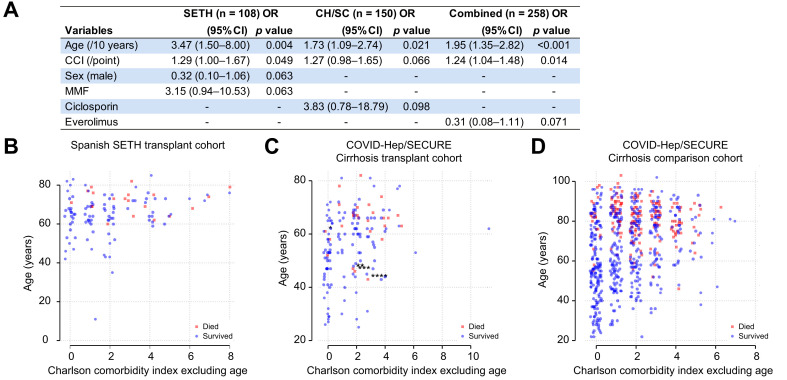
Fig. 1.
Associations between age and comorbidity with death following SARS-CoV-2 infection in liver transplant patients.
(A) Outcomes of multivariable logistic regression with backwards stepwise selection for retention in the model at p <0.1 with death as the dependent variable and the following independent variables: age, sex, Charlson comorbidity index (CCI; without age), hypertension, and baseline tacrolimus, ciclosporin, mycophenolate mofetil (MMF), everolimus, and corticosteroid use. SETH = cohort described by Colmenero et al; CH/SC = COVID-Hep/SECURE-Cirrhosis; combined represents the 2 cohorts combined. Within the SETH cohort, factors remaining significantly associated with death were age (odds ratio [OR] 3.47/10 years; 95% CI 1.50–8.00; p = 0.004) and CCI without age (1.29/point; 95% CI 1.00–1.67; p = 0.049). Within the COVID-Hep/SECURE-Cirrhosis cohort only age (OR 1.73/10 years; 95% CI 1.09–2.74; p = 0.02) remained significant. Within the combined cohort, age (1.95/10 years; 1.35–2.82; p <0.001) and CCI (OR 1.24; 95% CI 1.04–1.48; p = 0.014) remained significant. (B–D) Plots of age in years against CCI adjusted to exclude age and split by whether patients survived (blue circles) or died (red squares) following SARS-CoV-2 infection in (B) Spanish SETH cohort (n = 108 with complete data); (C) COVID-Hep/SECURE-Cirrhosis international cohort (n = 150); (D) COVID-Hep/SECURE-Cirrhosis comparison non-LT cohort from a single UK hospital network (n = 627). A single Spanish patient from the COVID-Hep/SECURE-Cirrhosis registries who could potentially have been included in the Spanish SETH registry was not included in the analysis. Asterisks for patients who died with CCI <3 (including points for age) in panel B denote additional at-risk cofactors: ∗concurrent influenza; ∗∗second liver transplant; ∗∗∗recurrent primary sclerosing cholangitis with jaundice at baseline; ∗∗∗∗baseline jaundice of unknown cause. Horizontal jitter has been added to the X axis. (This figure appears in color on the web.)