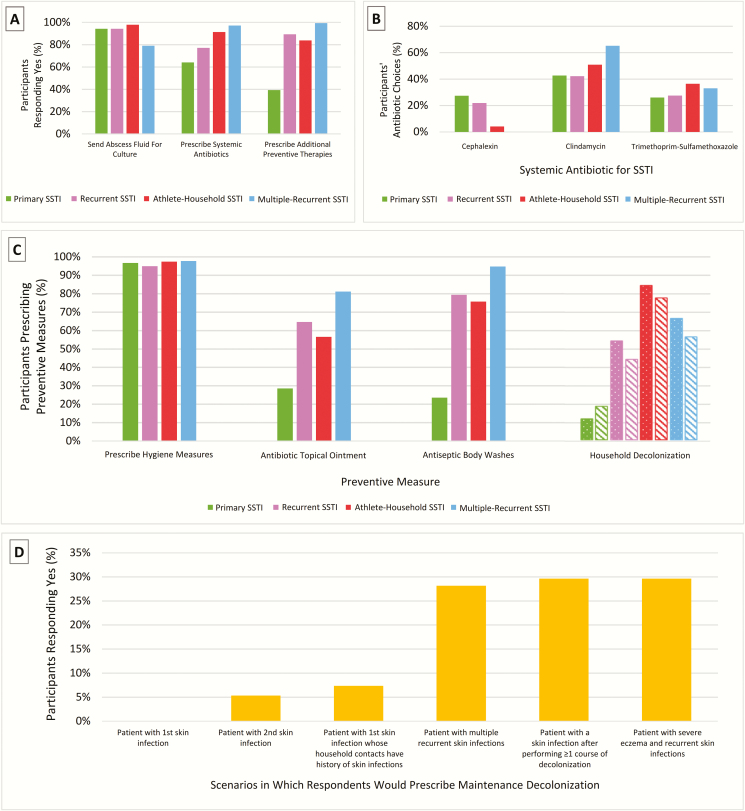
Figure 1.
A, Acute skin and soft tissue infection (SSTI) management respondents indicating “yes” by scenario (primary SSTI, recurrent SSTI, athlete-household SSTI, multiple-recurrent SSTI) to the questions “Would you send the abscess drainage fluid to the clinical microbiology laboratory for culture and antibiotic susceptibility testing?”; “Would you prescribe a systemic antibiotic (intravenous, intramuscular, oral) for this patient?”; and “Would you prescribe any additional management measures to prevent recurrent abscesses (eg, hygiene measures, topical antimicrobials) for this patient?” B, Systemic antibiotic selection for acute SSTI. The 3 most frequently prescribed antibiotics across all scenarios were clindamycin (51%), trimethoprim-sulfamethoxazole (31%), and cephalexin (12%). Amoxicillin, amoxicillin-clavulanate, doxycycline, and linezolid accounted for <5% of responses. C, Index patient and household contact preventive measures. For respondents stating that they would recommend additional measures to prevent recurrent SSTI, specific preventive measures are demonstrated by scenario. Solid bars indicate that the response is applied to the index patient. Patterned bars indicate household contacts: Dots indicate topical antibiotic, and stripes indicate antiseptic body washes. D, Scenario(s) for which respondents would prescribe maintenance decolonization. Respondents were more likely to prescribe maintenance decolonization for patients presenting with multiple, recurrent skin infections, patients presenting with a skin infection after previously performing at least one course of decolonization measures, and patients with severe eczema and recurrent skin infections.