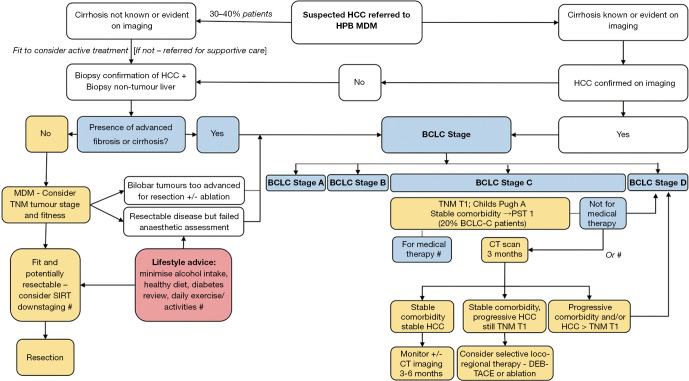
Figure 2.
HCC MDT care in a centre with high prevalence of metabolic syndrome and NAFLD. In Newcastle upon Tyne, UK, NAFLD is the commonest cause of HCC and over two thirds of patients have the metabolic syndrome irrespective of their underlying liver disease etiology. NAFLD patients are more likely to present in the absence of cirrhosis and require biopsy confirmation of their HCC and liver disease stage. The BCLC algorithm guides treatment strategies in cirrhotic patients and in non-cirrhotic patients, liver function may be better preserved and more radical surgical approaches may be appropriate in those that are fit enough. In NAFLD patients classed as BCLC-C, medical therapies may not be ideal (e.g., restricted mobility, renal or cardiac impairment). Selective TACE may be better tolerated and preferable to supportive care in some instances. This figure summaries the modified BCLC pathway (yellow boxes) directed by the Newcastle upon Tyne Hepatopancreatobiliary multidisciplinary team (HPB MDT), with # noting those areas where the evidence base is lacking and research or service improvement audits are necessary to inform future modifications to clinical practice. HPB, hepatobiliary; MDM, multidisciplinary meeting; HCC, hepatocellular carcinoma; BCLC, Barcelona Clinic for Liver Cancer; TNM, tumor node metastasis; ECOG-PS, Eastern Cooperative Oncology Group Performance Status; HCC, hepatocellular carcinoma; MDT, multidisciplinary team; SIRT, selective internal radiation therapy; DEB-TACE, drug-eluting bead transarterial chemoembolization; NAFLD, non-alcoholic fatty liver disease.