Abstract
Introduction
Tailgut cysts (TGC) are rare congenital retrorectal lesions deriving from vestiges of the hindgut. The risk of malignant transformation is relatively high. Thus early diagnosis and a complete removal of the mass are of paramount importance. We present a case of successful robotic exeresis of a large TGC adenocarcinoma.
Presentation of case
A healthy 35-year-old woman was found to have a retrorectal TGC with suspected malignant transformation. The patient underwent complete robotic resection of the mass and pathology confirmed a TGC adenocarcinoma. The patient’s post-operative course was unremarkable. At 24 months, the patient has not experienced any recurrence nor complained functional disorders.
Discussion
The current case highlights the importance of TGC as a differential diagnosis of presacral masses, underscoring that malignant transformation can occur and may result in mortality and morbidity if radical surgery is not performed.
Diagnosing TGC adenocarcinoma can be challenging because of its relatively low incidence. Biopsy is not recommended while magnetic resonance imaging (MRI) is indispensable in the evaluation of this lesion as the presence of intracystic vegetations could indicate a malignant transformation.
Surgery is the mainstay of treatment and minimally invasive techniques have the potential to minimize morbidity and enhance recovery. Amongst these, the robotic approach can make the dissection of large lesions easier, reducing their manipulation and preventing nerve injuries.
Conclusion
Robot-assisted resection of a TGC adenocarcinoma is safe and feasible. This approach can be particularly useful in the pelvis providing acceptable functional and oncological outcomes.
Keywords: Retrorectal, Tailgut cyst, Robotic surgery, Minimally invasive surgery, Malignancy, Case report
1. Introduction
Tailgut cysts (TGCs) are rare congenital retrorectal lesions arising from remnants of the hindgut with a predominance in female gender [1]. These lesions present diagnostic and management challenges. Complete surgical excision is always required to establish the diagnosis and to prevent complications including infections, fistulas and malignant transformations.
The choice of surgical approach is made according to the size and the degree of proximal extension of the cyst, its relationship with the surrounding structures and the suspect of malignancy, necessitating en-bloc resection. If the upper extension of the mass is above the level of S3, an anterior or a combined approach is usually preferred [2]. In recent years minimally invasive techniques, mostly laparoscopic [3], have been applied for the anterior excision of retrorectal tumors previously approached via laparotomy.
We report a case of robotic removal of a large TGC with suspected malignant transformation treated in a tertiary referral center, underlining the advantages of the robotic platform in terms of technical feasibility, functional results and oncological outcomes.
The case was reported according to the Surgical CAse Report (SCARE) criteria [4].
2. Presentation of case
A healthy 35-year-old female with BMI 26.2 reported progressively worsening pelvic pain, constipation and tenesmus. On digital examination, a large soft mass was perceived on the posterior rectal wall, fixed to the posterior plane with lower margin at 4 cm from the anal verge. The upper edge wasn’t detectable by the examiner’s finger. Rigid proctoscopy confirmed a posterior prominence of the mid-lower rectum, covered by intact smooth mucosa.
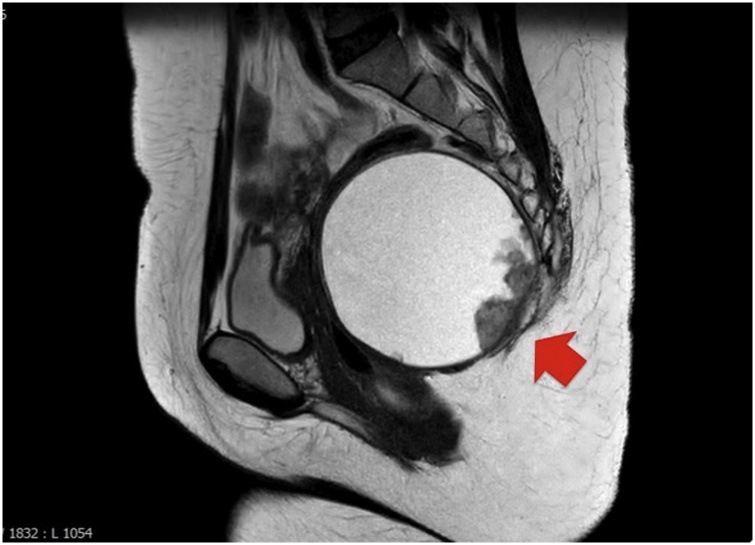
Magnetic resonance imaging (MRI) revealed a bulky unilocular 100 × 95 × 98 mm cyst with a thin wall in the retrorectal space, extending up to the body of S2. Posteriorly, the lesion was strongly attached to the sacro-coccygeal vertebral plane, whose aspect remained regular, whereas anteriorly it caused a marked rectal displacement and compression. The cyst appeared with low to intermediate T1 signal intensity. Fig. 1 shows T2-weighted images of the enhanced cyst with some internal low-density irregular thickening on the posterior wall. In T1-weighted contrast images these vegetations present a moderate signal density (Fig. 2).
Fig. 1.
Sagittal T2-weighted image of the pelvis showing a large well demarcated high-signal intensity cyst with small-sized hypointense masses on the posterior part of the lesion (arrow).
Fig. 2.
T1-weighted contrast image showing irregular masses on the posterior wall of the cyst (arrow) with intermediate signal intensity. A wall thickening can also be seen at the level of the masses.
The serum levels of carcinoembryonic antigen (CEA) and carbohydrate antigen 19–9 (CA 19–9) were also within normal ranges.
A preoperative diagnosis of retrorectal TGC with suspected malignant transformation was made. Other cystic lesions in this location, such as epidermoid or dermoid cyst, rectal duplication cyst, anterior meningocele, and cystic lymphangioma were also taken into consideration. On the basis of these findings, after a multidisciplinary consultation, the patient was offered a robot-assisted (da Vinci® Si™ System) anterior exeresis of the mass.
2.1. Operative technique
Thromboprophylaxis and cephazoline 2 g i.v. plus metronidazole 500 mg i.v. were administered 12 h and one hour before the surgery, respectively. A thoracic epidural catheter for postoperative pain control was inserted.
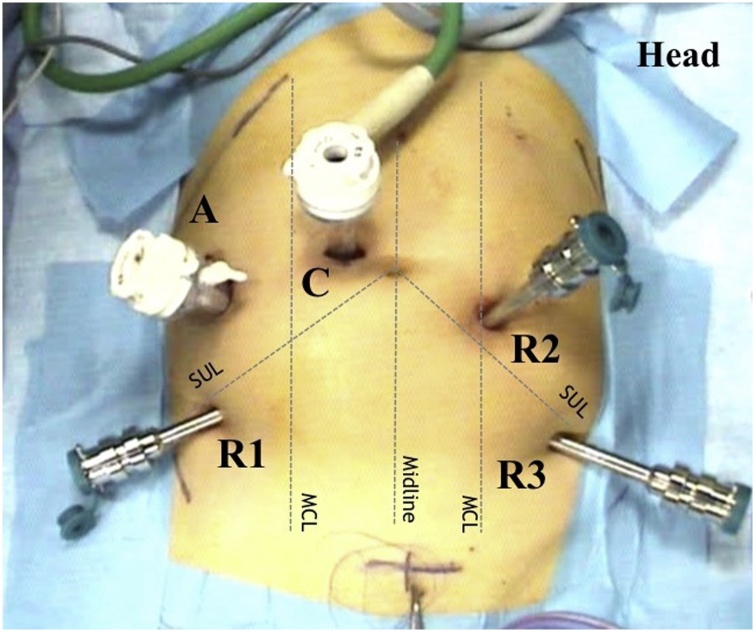
Following general anesthesia, the patient was placed supine in a modified Lloyd Davies position. A 12 mmHg pneumoperitoneum was achieved with a Veress needle. A 12 mm laparoscopic trocar for the 30° down endoscope was inserted through a right para-umbelical incision. Three robotic trocars were placed in a semi-circular line with the concavity facing the pelvis and a 12 mm laparoscopic trocar for the assistant was positioned in right flank (Fig. 3). Exploratory laparoscopy evidenced the rectum and the mesorectum raised by the retrorectal mass (Fig. 4).
Fig. 3.
da Vinci® Si™ port layout. SUL, spino umbilical line; MCL, midclavicular line; C, camera port; A, assistant port; R1, robotic arm#1; R2, robotic arm#2; R3, robotic arm#3.
Fig. 4.
Intraoperative exposure of the retroperitoneal tumor (dashed line). Rectum is compressed and anteriorly displaced.
The patient was subsequently placed in a 15° Trendelenburg position with a 10° right tilt and the cart was docked from the lower left quadrant over the left hip, at approximately 45° to the patient.
The right pelvic peritoneum was incised at the sacral promontory and the rectum was mobilized. The mass was carefully dissected first from the presacral plane, next from the right and left pelvis, preserving the hypogastric nerves and the inferior hypogastric plexus, and finally from the mesorectum and rectum itself. Due to the large dimensions of the cyst and consequently to the increased risk of rupture, a partial decompression of the mass was carried out with the careful aspiration of about 300 cc of cloudy fluid, carefully avoiding spillage. Intraoperative cytological exam on the inner cystic liquid was negative for atypical cells.
Finally, the excision was continued down to the levator-ani muscular plane that was completely visualized and freed from the strong adhesions to the lesion. The fully intact cyst was then inserted into an endobag. The rectal integrity was assessed with an air leak test. A spiral drain was placed in the pelvis and the specimen was extracted through the enlarged assistant port site.
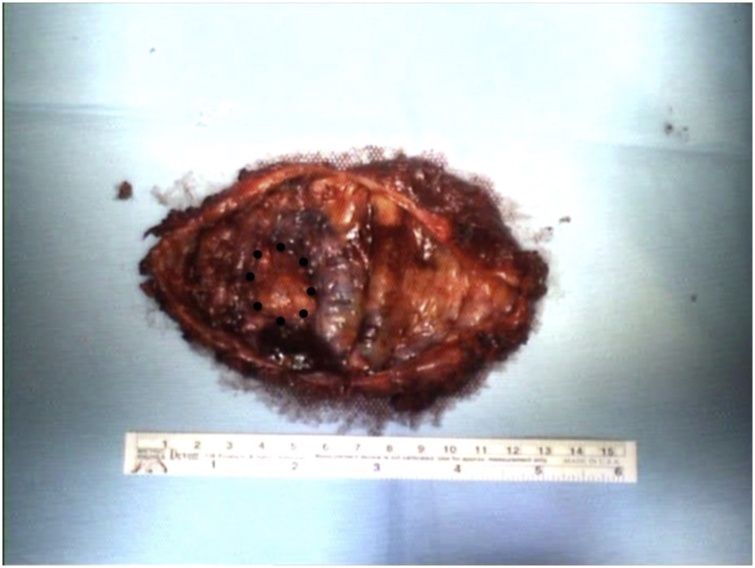
Total operative time was 214 min. After an uneventful postoperative course, the patient was discharged on post-operative day 4. Final pathology revealed a malignant neoplasm with a predominantly intestinal pattern of adenocarcinoma arising from a TGC (Fig. 5). Margins were negative and the liquid of the cyst was confirmed to be negative for atypical cells. Immunohistochemistry showed diffuse positivity for homeobox protein CDX2 (CDX2) and CEA, focal positivity for cytokeratin 20 (CK20) and rare positivity for cytokeratin 7 (CK7).
Fig. 5.
Gross appearance of opened resected specimen with internal vegetations (dotted line).
The case was discussed at a multidisciplinary consultation. Given the complete exeresis of the entire mass and the negative resection margins, a strict follow up program was proposed. At 24 months follow-up, the patient remains free of symptoms and no recurrence has been detected.
3. Discussion
We presented a case of successful robotic anterior removal of a retrorectal adenocarcinoma arising from a degenerated TGC. This approach allowed a complete exeresis of the mass with acceptable functional and mid term-oncological outcomes.
Although most TGCs have been reported to be benign, recent data suggest that the risk of malignant transformation is high (up to 26%) [5,6], the majority being adenocarcinomas, neuroendocrine tumors and squamous carcinomas [7]. Consequently, an early and accurate diagnosis plays a crucial role along with radical surgical resection. However, to date, both diagnosis and appropriate surgical strategy represent a great challenge.
The presence of symptoms mainly related to the compression such as constipation and rectal tenesmus might not be associated to malignancy [5] except for lower abdominal pain complaints [8]. Although little data support the use of cancer markers, a test for CEA and/or CA 19−9 is recommended in the suspect of TGC adenocarcinoma [5,9].
Computed tomography scan and MRI represent the most helpful preoperative diagnostic tools especially for the differentiation between malignant and benign lesions. Cross sectional MRI might be considered superior to CT in the preoperative assessment of retrorectal tumours with an accuracy up to 95% [8]. In the current case, TGC presents as a cystic lesion with low signal intensity in T1-weighted images and high signal intensity in T2-weighted images. An enhancement of internal vegetations or calcification after intravenous injection of contrast media [7] raises the suspicion of malignancy.
Some controversy exists about the role of biopsies in suspected malignant TGCs. Indeed, most authors suggest that it should not be attempted (unless the mass is surgically unresectable at presentation) due to risks of tumor seeding and infection. Moreover, biopsy tissue is often not extensive enough to show all the histological features necessary to confirm the diagnosis [8,10]. Thus, as in the current case, a preoperative biopsy was not performed and the complete excision of the lesion was chosen for diagnosis and definitive treatment.
The type of surgical procedure depends on the level of the lesion, its size and the relationship with surrounding structures. According to the preoperative imaging tumors below S3 level should be approached posteriorly (Kraske [11]) or with a trans perineal approach. Lesions above S3 benefit from an anterior trans-abdominal approach or a combined anteroposterior approach [6]. Irrespective of the type of the access, TGCs should be entirely removed with adequate margins of the lesion and preventing injuries to surrounding structures [10].
Recently, there is growing evidence that laparoscopy for the abdominal approach might be safe and technically feasible for experienced hands, even in case of large retrorectal tumors [12] with surgical and oncological outcomes not inferior to the open technique [3]. However, a narrow pelvis and large dimensions could exacerbate technical difficulty and might lead to conversion [13]. Furthermore, vaginal, rectal and nerve injuries have been reported in laparoscopic case series [14,15].
The robotic system, thanks to its undoubted technical advantages, can allow better visualization, stability and easier dissection of the cyst, reducing the risk of pelvic injuries and making repair easier. In addition, since the removal of the whole cyst is paramount in preventing recurrence [6,16], we believe that the robotic platform, allowing for excellent exposure, precise maneuverability and improved dexterity with wristed instruments, can reduce the risk of lesion rupture [17].
Indeed, in the case presented, the large lesion was safely dissected away from the rectum and down to the levator-ani muscular plane without injuring the mass, surrounding organs and nerves. An intact R0 resection was carried out minimizing the risk of recurrence. Our findings are consistent with those shown in the few other case reports [3,13,[18], [19], [20]] but to the best of our knowledge, this is the first reported application of robotics for the treatment of TGC adenocarcinoma.
4. Conclusion
Robot-assisted resection of TGC adenocarcinoma is safe and feasible. This approach facilitates pelvic exposure and can reduce tissue damages with acceptable functional and oncological outcomes.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study has been exempted from ethical approval at our institution, however, permission has been sought from the patient in question to present and publish this case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
None.
Guarantor
Maria Carmela Giuffrida.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Alessandra Marano: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Maria Carmela Giuffrida: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Chiara Peluso: Software, Data curation. Valentina Testa: Software, Data curation. Paolo Bosio: Resources. Felice Borghi: Supervision, Writing - review & editing.
Acknowledgements
This article is part of a supplement entitled Case reports from Italian young surgeons, published with support from the Department of Surgical, Oncological and Oral Sciences - University of Palermo
References
- 1.Messick C.A., Hull T., Rosselli G., Kiran R.P. Lesions originating within the retrorectal space: a diverse group requiring individualized evaluation and surgery. J. Gastrointest. Surg. 2013;17:2143–2152. doi: 10.1007/s11605-013-2350-y. [DOI] [PubMed] [Google Scholar]
- 2.Li G.D., Chen K., Fu D., Ma X.J., Sun M.X., Sun W. Surgical strategy for presacral tumors: analysis of 33 cases. Chin. Med. J. (Engl.) 2011;124:4086–4091. [PubMed] [Google Scholar]
- 3.Mullaney T.G., Lightner A.L., Johnston M., Kelley S.R., Larson D.W., Dozois E.J. A systematic review of minimally invasive surgery for retrorectal tumors. Tech. Coloproctol. 2018;22:255–263. doi: 10.1007/s10151-018-1781-6. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;(60):132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Nicoll K., Bartrop C., Walsh S., Foster R., Duncan G., Payne C. Malignant transformation of tailgut cysts is significantly higher than previously reported: systematic review of cases in the literature. Colorectal Dis. 2019;21:869–878. doi: 10.1111/codi.14628. [DOI] [PubMed] [Google Scholar]
- 6.Akbulut S. Unusual cause of defecation disturbance: a presacral tailgut cyst. Eur. Rev. Med. Pharmacol. Sci. 2013;17:1688–1699. [PubMed] [Google Scholar]
- 7.Liang F., Li J., Yu K., Zhang K., Liu T., Li J. Tailgut cysts with malignant transformation: features, diagnosis, and treatment. Med. Sci. Monit. 2020;26:e919803. doi: 10.12659/MSM.919803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sagar A.J., Koshy A., Hyland R., Rotimi O., Sagar P.M. Preoperative assessment of retrorectal tumours. Br. J. Surg. 2014;101:573–577. doi: 10.1002/bjs.9413. [DOI] [PubMed] [Google Scholar]
- 9.Chhabra S., Wise S., Maloney-Patel N., Rezac C., Poplin E. Adenocarcinoma associated with tail gut cyst. J. Gastrointest. Oncol. 2013;4:97–100. doi: 10.3978/j.issn.2078-6891.2012.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li W., Li J., Yu K., Zhang K., Li J. Retrorectal adenocarcinoma arising from tailgut cysts: a rare case report. BMC Surg. 2019;19:180. doi: 10.1186/s12893-019-0639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Brien P.H. Kraske’s posterior approach to the rectum. Surg. Gynecol. Obstet. 1976;142:412–414. [PubMed] [Google Scholar]
- 12.Kwak H.D., Ju J.K. Laparoscopic resection of a huge retrorectal tumor. Ann. Coloproctol. 2020;36:54–57. doi: 10.3393/ac.2018.07.31.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eftaiha S.M., Kochar K., Pai A., Park J.J., Prasad L.M., Marecik S.J. Robot-assisted approach to a retrorectal lesion in an obese female. J. Vis. Surg. 2016;2:59. doi: 10.21037/jovs.2016.02.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakr A., Kim H.S., Han Y.D., Cho M.S., Hur H., Min B.S. Single-center experience of 24 cases of tailgut cyst. Ann. Coloproctol. 2019;35:268–274. doi: 10.3393/ac.2018.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nedelcu M., Andreica A., Skalli M., Pirlet I., Guillon F., Nocca D. Laparoscopic approach for retrorectal tumors. Surg. Endosc. 2013;27:4177–4183. doi: 10.1007/s00464-013-3017-1. [DOI] [PubMed] [Google Scholar]
- 16.Patsouras D., Pawa N., Osmani H., Phillips R.K. Management of tailgut cysts in a tertiary referral centre: a 10-year experience. Colorectal Dis. 2015;17:724–729. doi: 10.1111/codi.12919. [DOI] [PubMed] [Google Scholar]
- 17.Oh J.K., Yang M.S., Yoon D.H., Rha K.H., Kim K.N., Yi S. Robotic resection of huge presacral tumors: case series and comparison with an open resection. J. Spinal Disord. Tech. 2014;27:E151–154. doi: 10.1097/BSD.0b013e318299c5fd. [DOI] [PubMed] [Google Scholar]
- 18.Cataneo J., Cataldo T., Poylin V. Robotic excision of retrorectal mass. J. Gastrointest. Surg. 2018;22:1811–1813. doi: 10.1007/s11605-018-3838-2. [DOI] [PubMed] [Google Scholar]
- 19.Borsuk D.J., Studniarek A., Al-Khamis A., Kochar K., Park J.J., Marecik S.J. Robotic excision of a difficult retrorectal cyst - a video vignette. Colorectal Dis. 2020;22:226–227. doi: 10.1111/codi.14862. [DOI] [PubMed] [Google Scholar]
- 20.Wilhelm P., Jansen K., Rolinger J., Kirschniak A., Axt S., Johannink J. [First robotic assisted resection of a retrorectal tailgut cyst - video case report of a 27-year-Old female patient] Zentralbl. Chir. 2019;144:337–339. doi: 10.1055/a-0874-2584. [DOI] [PubMed] [Google Scholar]