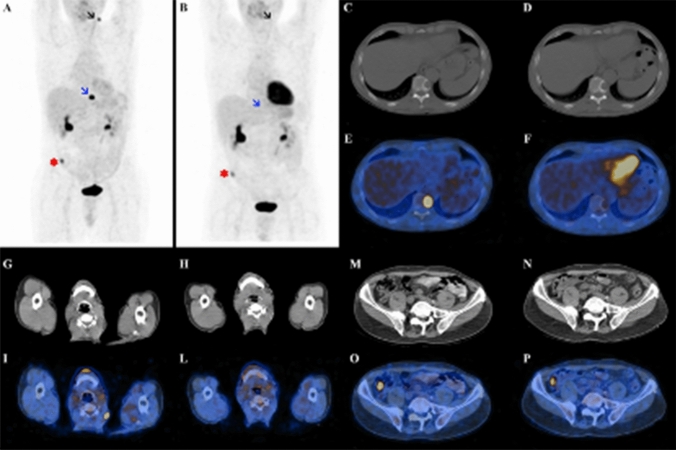
Fig. 5.
Case presentation of a 68-year-old male patient with metastatic PTC. He underwent total thyroidectomy (pT3mN1bMx) and two consecutive RAI treatments (cumulative activity 11.1 GBq). After the second RAI treatment, 18F-FDG PET/CT demonstrated three FDG-avid lesions: a left cervical lymph node (black arrow on a image; see also g and i), a lytic bone lesion in D10 (blue arrow on a image; see also c and e) and a focal intestinal uptake (asterisk on a image; see also m and o). So, the patient underwent a cervical lymphadenectomy that confirmed the thyroid origin of the lesion, and a Cyberknife radiosurgery of the D10 bone lesion (24 Gy). The subsequent follow-up 18F-FDG PET/CT scan demonstrated a complete metabolic response of the D10 bone lesion (blue arrow on b image; see also f), even if its radiological aspect was unchanged on CT (d); moreover, no further pathological radiotracer uptake was detected in the left cervical region (black arrow on b image; see also h and l). The focal intestinal uptake was stable (asterisk on b image; see also n and p) and was diagnosed as an adenomatous polyp at the subsequent polypectomy. The 18F-FDG PET/CT findings were further validated by the concomitant reduction of serum Tg levels. PTC papillary thyroid cancer, RAI radioactive iodine, 18F-FDG PET/CT 18F-fluorodeoxyglucose positron emission tomography/computed tomography, Tg thyroglobulin