Figure 2.
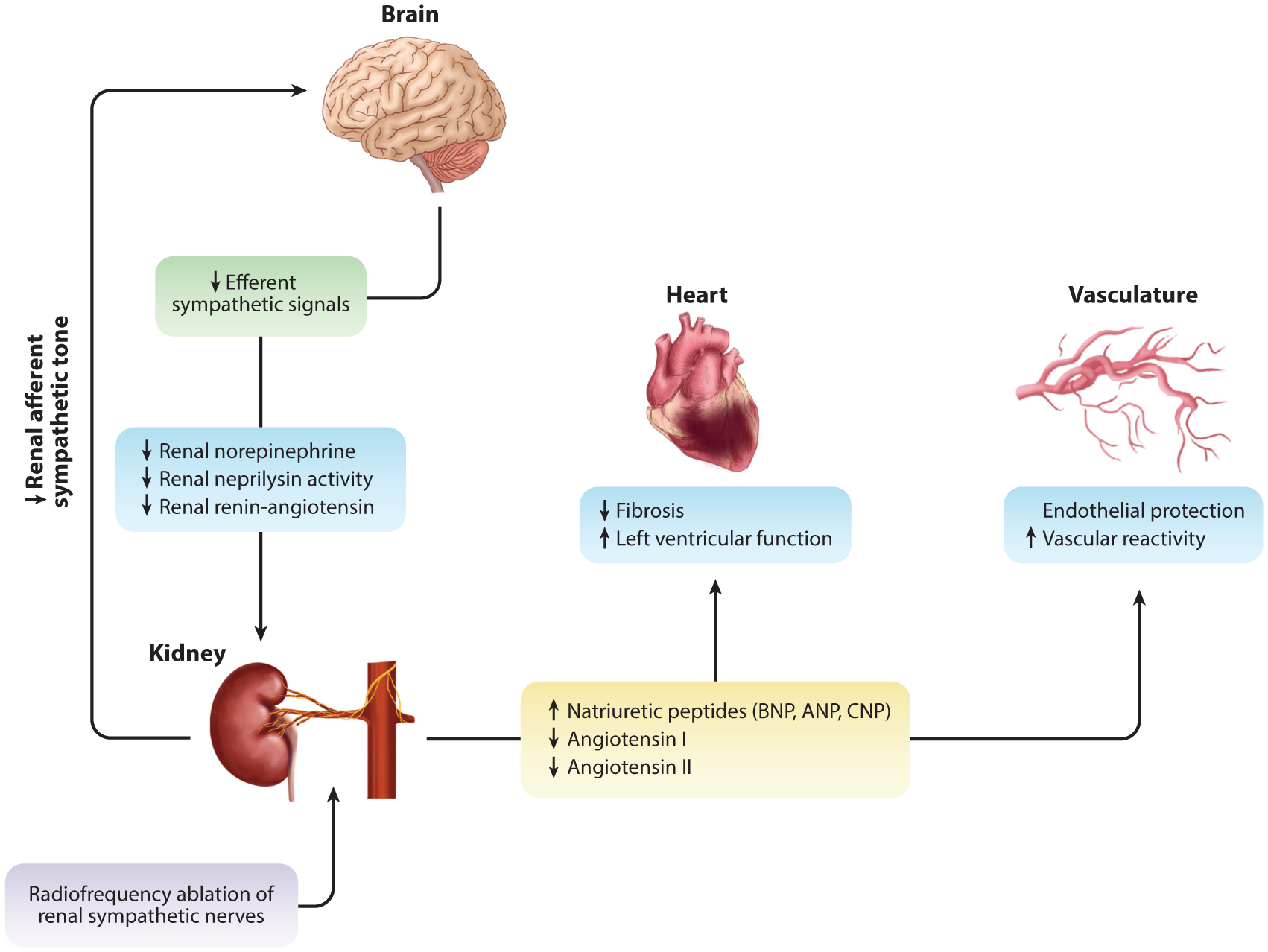
The effects of renal sympathetic nerve ablation in HFrEF. With chronic overactivation observed in heart failure, renal afferent input into the central nervous system plays an integral role in efferent output. Through renal sympathetic nerve ablation (purple box), preclinical data suggest a reduction in efferent signaling to the kidney (green box) through a reduction in renal norepinephrine and concurrent reduction in renal neprilysin activity and attenuation renin-angiotensin system activation (blue boxes). This leads to reduced renal fibrosis and improved function (17, 18). Neprilysin inhibition promotes sustained exposure to natriuretic peptides in circulation, and reduced efferent sympathetic signal inhibits renin production and downstream circulating levels of angiotensin I and II (yellow box). Improved natriuretic peptide exposure and reduced angiotensin I and II lead to reduced cardiac fibrosis and improved function. Further cardiovascular protection is afforded to the vasculature, whereby there is improved vascular reactivity to classical vasodilators [i.e., bradykinin, substance P (endothelial-dependent), and sodium nitroprusside (endothelial-independent)] (blue boxes). Abbreviations: ANP, atrial natriuretic peptide; BNP, B-type natriuretic peptide; C-type natriuretic peptide; HRrEF, heart failure with a reduced ejection fraction.
