Abstract
Considering the importance of evidence on interventions to tackle mental health problems in healthcare workers (HCWs) during pandemics, we conducted a systematic review, aiming to identify and summarize the implemented interventions to deal with mental health issues of HCWs during infectious disease outbreaks and report their effectiveness. Web of Science, PubMed, Cochrane, Scopus, CINAHL and PsycInfo electronic databases were searched until October 2nd, 2020. Primary-data articles, describing any implemented interventions and their effectiveness were considered pertinent. Studies were screened according to the inclusion/exclusion criteria and subsequently data extraction was performed. Twenty-four articles, referring to SARS, Ebola, Influenza AH1N1 and COVID-19 were included. Interventions addressing mental health issues in HCWs during pandemics/epidemics were grouped into four categories: 1) informational support (training, guidelines, prevention programs), 2) instrumental support (personal protective equipment, protection protocols); 3) organizational support (manpower allocation, working hours, re-organization of facilities/structures, provision of rest areas); 4) emotional and psychological support (psychoeducation and training, mental health support team, peer-support and counselling, therapy, digital platforms and tele-support). These results might be helpful for researchers, stakeholders, and policymakers to develop evidence-based sustainable interventions and guidelines, aiming to prevent or reduce the immediate and long-term effect of pandemics on mental health status of HCWs.
Keywords: Mental health, Healthcare workers, Pandemic, Epidemic, Interventions
1. Introduction
COVID-19, known as an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), is manifesting several indirect effects, many of which are not known yet, in particular those concerning healthcare workers (HCWs) at the forefront of patient care (Maxwell et al., 2020).
World Health Organization (WHO) declared COVID-19 a global pandemic on March 11, 2020 (Cucinotta and Vanelli, 2020) and up to February 3, 2021, there have been 103, 201, 340 confirmed cases and 2,237,636 deaths (“WHO Coronavirus Disease (COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard,” n. d.). Upon the arrival of the pandemic, health systems were overwhelmed by the impossibility to effectively respond to the needs of the multitude of infected patients, mainly due to the high virulence and contagiousness of SARS-CoV2 and the sudden onset of severe symptoms (Christopher et al., 2020).
HCWs, working under pressure, with prolonged work shifts encountered several ethical dilemmas and saw many of their colleagues lose the battle to SARS-CoV2 (Robert et al., 2020). An international survey on COVID-19 management strategies showed that in many countries, HCWs did not have sufficient access to adequate supplies at the beginning of the pandemic and that their healthcare organizations had been slow to apply measures of infection prevention and control (Tartaglia et al., 2020).
Along with the poor supply of personal protective equipment (PPE), they had to deal with the lack of trained personnel, the fear of being infected and becoming a possible infecting vehicle for their families and patients, and frustration over loss of life (Wu et al., 2009).
HCWs could not see their families and friends, so they could not count on their emotional support to get through these difficult times. All these factors undermined the physical and mental well-being of frontline HCWs (Zaka et al., 2020).
Evidence from the previous pandemics or epidemics suggests that during a disease outbreak HCWs experience several mental health issues, which besides affecting their health and professional performance at the moment, may also have long-term negative effects (Maunder et al., 2003; Serrano-Ripoll et al., 2020; Wu et al., 2009).
HCWs represent a high-risk group for experiencing mental health issues (Maben and Bridges, 2020). Mental health disorders of HCWs encountered during previous epidemics included anxiety, depression, exhaustion, post-traumatic stress disorder (O'Sullivan et al., 2007), insomnia, relationship difficulties, behavioral changes (such as anger or substance use) (Waterman et al., 2018), burnout and anticonservative ideas (Maben and Bridges, 2020). During the COVID-19 pandemic, the prevalence of anxiety among HCWs varied from 7% (5%–9%) in Singapore to 57% (52%–63%) in Italy, while the prevalence of depression ranged between 9% (7%–12%) in Singapore and 51% (48%–53%) in China (Luo et al., 2020).
HCWs’ well-being is important not only for them and their families, but it also has an enormous impact on the quality of assistance to the patients, having a crucial role in the whole healthcare system (Maben and Bridges, 2020).
But if coping with the pandemic has been challenging for healthcare systems, dealing with the mental health of HCWs seems to be even harder. Little attention and time are given to mental health issues of HCWs. Published literature focuses mainly on the impact of pandemics on the mental state of HCWs and less on implemented interventions and their effectiveness to overcome these conditions (Luo et al., 2020; Serrano-Ripoll et al., 2020).
Considering the importance of evidence regarding interventions to tackle mental health problems in HCWs during pandemics, we conducted a systematic review, aiming to identify and summarize the implemented interventions to deal with mental health issues of HCWs during infectious disease outbreaks, and report their effectiveness.
2. Materials and methods
This systematic review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009) (Supplementary File 1).
The protocol of this systematic review was registered to PROSPERO, registration number CRD42020196383 (Zace et al., 2020).
2.1. Research question and definitions
To address our objective, a specific research question was structured using the Population, Interventions, Comparison, Outcomes, and Study designs (PI/ECOST) criteria as follows:
-
-
Population: Health care workers (HCWs)
-
-
Intervention or Exposure: We considered as exposure the current and previous infectious disease outbreaks that have caused pandemics or epidemics and have put an extra burden on the healthcare systems of different countries
-
-
Comparison: Not Applicable
-
-
Outcome: Implemented interventions or strategies which could have a direct or indirect impact on the mental health of healthcare workers during infectious disease outbreaks.
-
-
Study designs: Any study design reporting primary data
-
-
Time: Any timeframe
For the purpose of our systematic review, we referred to following definitions:
HCWs are intended as any person working in Healthcare System, inside or outside the hospital, such as physicians, nurses, technicians, general practitioners or administrative staff. Mental health includes emotional, psychological, and social well-being. It affects how people think, feel, act, and how they relate to others. It also helps determine how stress is handled. Intervention is defined as any act taken at a structure/facility or higher level to prevent negative outcomes or improve mental health of HCWs. The primary outcome of this systematic review is to describe the interventions that have been implemented to tackle mental health issues in HCWs during infectious disease outbreaks. Our secondary outcome includes the measures of these interventions’ efficacy.
2.2. Search strategy
Electronic search: The research was conducted on Web of Science, PubMed, Cochrane, Scopus, CINAHL and PsycInfo electronic databases looking for pertinent articles. A search string was built for PubMed consisting of Medical Subject Headings (MeSH) terms and free text words. The Boolean operators were used to combine keywords such as “Mental Health”, “occupational stress”, “mental hygiene”, “stress”, “healthcare worker”, “intervention”, “action”, “initiative”, “strategy” “Pandemics”, “Epidemics”, “Disease Outbreaks”. Afterwards, this search string was adapted for use in the other electronic databases (Supplementary File 2). The search was restricted to articles published in English, without any further restrictions and was first performed on June 6th, 2020 for all databases. However, we decided to update our search until October 2nd, 2020, since several pertinent articles were published meanwhile.
Other resources: The reference lists of the included studies were hand searched to look for additional articles. To ensure we did not miss any pertinent articles, we pulled several review articles reporting mental health of HCWs during infectious disease outbreaks and reviewed their references.
2.3. Study selection and inclusion/exclusion criteria
Qualitative studies reporting experiences and describing any implemented intervention targeting mental health of HCWs, and quantitative studies reporting the effectiveness of interventions on mental health of HCWs during infectious disease outbreaks, were considered pertinent. We included articles that described resilience and how to help HCWs to improve their ability to react to stressful situations. Only peer-reviewed articles, with no time limits, were included.
We excluded articles reporting personal activities or personal coping mechanisms of HCWs to face infectious disease outbreaks, as well as articles that reported interventions to address mental health issues of infected HCWs. Furthermore, we excluded articles that performed baseline evaluation of the mental health status of HCWs without intervention, and articles, which were not primarily designed to report an implemented intervention on mental health. Lastly, we excluded articles that did not report primary data, such as systematic reviews, narrative reviews, opinions, short communications, perspectives, or letters to editors.
All articles retrieved from the search strategy were imported to Mendeley and duplicates were removed. The remaining articles were uploaded to Rayyan (Qatar Computing Research Institute) software. The first screening based on title and abstract was completed independently by a minimum of two of the following authors: DZ, IH, AO, AMV. In a second step, articles with full texts available were carefully reviewed by a minimum of two researchers (DZ, IH AO, AMV) and disagreements were resolved by consensus. Corresponding authors were contacted in case the full texts of any articles were not available online.
2.4. Data extraction and synthesis
Data extraction was performed by four researchers who worked in groups. A dedicated data extraction form was used retrieving the following information for each eligible study: (1) Study identification: first author, title, publication year; (2) Study characteristics: country, design, infectious disease; (3) Population characteristics: sample size and type, occupation, sex, age; (4) Implemented intervention characteristics: intervention type; duration, setting, mental health indicators evaluated, psychometric instruments/tools utilized to evaluate mental health indicators; (5) Measure of effectiveness of the interventions.
Data synthesis was carried out using Excel spreadsheets. Firstly, for each included article we created notes on the interventions implemented and associated characteristics. Subsequently, we coded each type of intervention and based on these, we grouped the interventions into four main categories: 1) informational support, 2) instrumental support, 3) organizational support and 4) emotional and psychological support. Each article was summarized and described according to variables such as targeted population (occupation, age, sex), type of intervention, setting, duration, and, when available, the effectiveness of the intervention.
Most articles did not report sufficient information regarding population, setting, tools used to assess mental health and targeted mental health indicators, so it was not possible to perform a quantitative analysis. Articles with quantitative data on the effectiveness of the implemented intervention, presented high heterogeneity in assessment measures, tools used to assess mental health and different indicators of mental health. Hence, it was not possible to perform a quantitative analysis of the effectiveness of each intervention on HCWs’ mental health.
2.5. Quality assessment
When appropriate, two researchers (AO, AMV) independently conducted the methodological quality assessment, based on the study designs. Disagreements were resolved by discussion with a third researcher (DZ). For the before-after study designs, we used the “Study Quality Assessment Tools” of the National Heart, Lung and Blood Institute (NIH, n.d.). This tool evaluates twelve criteria and based on the number of criteria satisfied classifies studies in good, fair, or poor. For the other included articles, the Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI) was used to assess the methodological quality (Moola et al., 2020). This tool offers the possibility to appraise the methodological quality of articles based on the satisfaction or not of several specific criteria for each study design. To summarize the overall evidence quality, we grouped the articles into three categories: good (studies met at least 75% of the quality criteria), moderate (studies met between 50% and 74% of the quality criteria) and poor (studies met less than 50% of the quality criteria) methodological quality.
3. Results
3.1. Search results
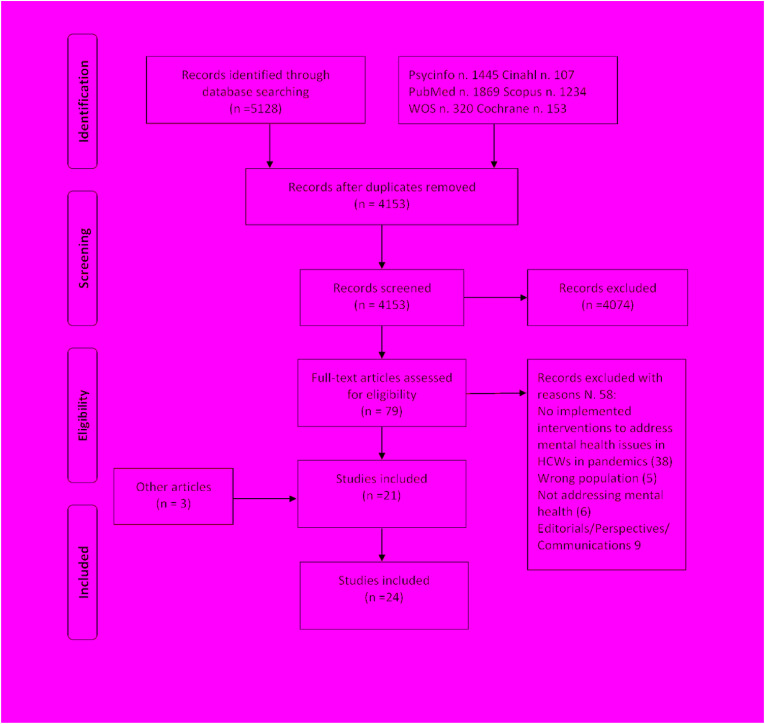
Our search strategy produced a total of 5128 articles from all the databases. After the screening process, 21 articles (Aiello et al., 2011; Albott et al., 2020; Bansal et al., 2020; Blake et al., 2020; Buselli et al., 2020; Cai et al., 2020; Chen et al., 2006; Cheng et al., 2020; Cheung et al., 2020; Cole et al., 2020; Donnelly et al., 2020; Feinstein et al., 2020; Gonzalez et al., 2020; Hong et al., 2020; Maunder et al., 2003, 2010; Ping et al., 2020; Schreiber et al., 2019; Sockalingam et al., 2020; Waterman et al., 2018; Zhou et al., 2020) were eligible to be included in the systematic review (Fig. 1 ). Through the hand-search of the latter, three additional articles (Geoffroy et al., 2020; Giordano et al., 2020; Khee et al., 2004) were identified and included.
Fig. 1.
Flow chart of the screening and selection process in the systematic review according to PRISMA flow diagram.
3.2. Characteristics of the included studies
Most of the included articles reported interventions implemented in China (20.8%) (Cai et al., 2020; Cheng et al., 2020; Cheung et al., 2020; Hong et al., 2020; Zhou et al., 2020) and Canada (16.7%) (Aiello et al., 2011; Maunder et al., 2003, 2010; Sockalingam et al., 2020), followed by USA (Albott et al., 2020; Feinstein et al., 2020; Gonzalez et al., 2020) and UK (Blake et al., 2020; Cole et al., 2020; Donnelly et al., 2020) (12.6%, respectively). The rest of the articles referred to Italy (Buselli et al., 2020; Giordano et al., 2020) and Africa (Schreiber et al., 2019; Waterman et al., 2018) (8.4%, respectively), and Taiwan (Chen et al., 2006), Singapore (Khee et al., 2004), Malaysia (Ping et al., 2020), France (Geoffroy et al., 2020), Spain (Mira et al., 2020) (4.1%, respectively).
One third of the articles had a cross-sectional design (33.35%) (Aiello et al., 2011; Blake et al., 2020; Buselli et al., 2020; Cheung et al., 2020; Geoffroy et al., 2020; Hong et al., 2020; Maunder et al., 2003; Sockalingam et al., 2020), followed by a before-after design (20.8%) (Chen et al., 2006; Cheng et al., 2020; Giordano et al., 2020; Maunder et al., 2010; Zhou et al., 2020), cohort (8.4%) (Cai et al., 2020; Waterman et al., 2018) and qualitative (4.1%) (Khee et al., 2004) design. Meanwhile, 33.35% of articles did not have a specific study design (Albott et al., 2020; Cole et al., 2020; Donnelly et al., 2020; Feinstein et al., 2020; Gonzalez et al., 2020; Mira et al., 2020; Ping et al., 2020; Schreiber et al., 2019), since they just described the interventions implemented, and were classified as narrative descriptions. As for the infectious disease outbreaks, the vast majority of articles referred to COVID-19 pandemics (70.7%) (Albott et al., 2020; Blake et al., 2020; Buselli et al., 2020; Cai et al., 2020; Cheng et al., 2020; Cheung et al., 2020; Cole et al., 2020; Donnelly et al., 2020; Feinstein et al., 2020; Geoffroy et al., 2020; Giordano et al., 2020; Gonzalez et al., 2020; Hong et al., 2020; Mira et al., 2020; Ping et al., 2020; Sockalingam et al., 2020; Zhou et al., 2020), 12.5% to SARS (Chen et al., 2006; Khee et al., 2004; Maunder et al., 2003), and 8.4% to Ebola (Schreiber et al., 2019; Waterman et al., 2018) and Influenza A H1N1 (Aiello et al., 2011; Maunder et al., 2010), respectively. When reported, the sample size ranged from 25 nurses in a pilot study in Malaysia (Ping et al., 2020), to 10,240 staff members in a cross-sectional study in China (Hong et al., 2020) during COVID-19. The age of participants ranged from a minimum of 16 years old (Waterman et al., 2018) to 66 years old (Buselli et al., 2020). The majority of the articles included all staff members, with 12.5% conducted only among nurses (Cai et al., 2020; Chen et al., 2006; Zhou et al., 2020). All articles, except one conducted in Sierra Leone during Ebola outbreak, had included a vast majority of female HCWs, ranging from 64.7% (Giordano et al., 2020) to 100% (Zhou et al., 2020) (Table 1 ).
Table 1.
Characteristics of the twenty-four articles included in the systematic review.
| First Author, Year | Study design | Sample type | Country | Disease | Sample size | Occupation | Sex | Age, years old | Quality assessment criteria satisfied (%) |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al., 2006 | Before-after | Voluntary response sample | Taiwan | SARS | 116 | Nurses | F: 98.3% M: 1.7% | 31 +-10.8 | 58.3 |
| Aiello et al., 2011 | Cross sectional | Convenience sample | Canada | Influenza A H1N1 | 1,250 | All staff | NA | NA | 75 |
| Waterman et al., 2018 | Cohort study | Voluntary response sample | Sierra Leone | Ebola | 3,273 | All staff | F: 19.6% M: 45.7% not specified: 34.7% |
29.46+-7.40 (16–63) | 63 |
| Schreiber et al., 2019 | Narrative description | Convenience sample | West Africa | Ebola | 45 | All staff | NA | 25–60 | NA |
| Blake et al., 2020 | Cross sectional | Convenience sample | UK | COVID-19 | 55 | All staff | NA | NA | 75 |
| Maunder et al., 2003 | Cross sectional | Convenience sample | Canada | SARS | NA | All staff | NA | NA | 50 |
| Maunder et al., 2010 | Before-after | Convenience sample | Canada | Influenza A H1N1 | 158 | All staff | F: 81% M:19% | NA | 66.6 |
| Khee et al., 2004 | Qualitative | Convenience sample | Singapore | SARS | 188 | All staff | NA | NA | 60 |
| Geoffroy et al., 2020 | Cross sectional | Voluntary response sample | France | COVID-19 | 149 | All staff | F: 86% M:14% | 32.7+-11 (19–56) | 75 |
| Buselli et al., 2020 | Cross sectional | Voluntary response sample | Italy | COVID-19 | 106 | All staff | F: 74.5% M: 25.5% | 50 +- 9.9 (28–66) | 75 |
| (Cai et al., 2020) | Cohort study | Convenience sample | China | COVID-19 | 1,330 | Nurses | F: 97% M: 3% | 18–25: 22.8%; 26–30: 34.6%; 30–40: 28.3%; >40: 14.3% |
54.5 |
| Zhou et al., 2020 | Before-after | Convenience sample | China | COVID-19 | 71 | Nurses | F: 100% | 20–30: 49.3%; 31–40: 45.07% >41: 4.23% |
41.6 |
| Sockalingam et al., 2020 | Cross sectional | Voluntary response sample | Canada | COVID-19 | 426 | All staff | NA | NA | 50 |
| Gonzalez et al., 2020 | Narrative description | Convenience sample | USA | COVID-19 | NA | All staff | NA | NA | NA |
| Donnelly et al., 2020 | Narrative description | Convenience sample | UK | COVID-19 | NA | All staff | NA | NA | NA |
| Ping et al., 2020 | Narrative description | Convenience sample | Malaysia | COVID-19 | 25 nurses (pilot) | Nurses | NA | NA | NA |
| Cheung et al., 2020 | Cross sectional | Convenience sample | China | COVID-19 | 1,415 | All staff | F: 66% M: 34% | NA | 75 |
| Albott et al., 2020 | Narrative description | Convenience sample | USA | COVID-19 | NA | All staff | NA | NA | NA |
| Cole et al., 2020 | Narrative description | Convenience sample | UK | COVID-19 | NA | All staff | NA | NA | NA |
| Feinstein et al., 2020 | Narrative description | Convenience sample | USA | COVID-19 | NA | All staff | NA | NA | NA |
| Cheng et al., 2020 | Before-after | Convenience sample | China | COVID-19 | 155 | All staff (doctors, nurses administrative) | F: 68.4% M: 31.6% | Mean age 35 | 58.3 |
| Giordano et al., 2020 | Before-after | Convenience sample | Italy | COVID-19 | 34 | Doctors, nurses | F: 64.7% M: 35.3% | 31.8 +- SD = 8.33 (22–59) | 75 |
| Hong et al., 2020 | Cross sectional | Convenience sample | China | COVID-19 | 10,240 | All staff (doctors, nurses, laboratory technician) | F: 75.5% M: 24·5% | Median age 30 (27-36) | 75 |
| Mira et al., 2020 | Narrative description | Voluntary response sample | Spain | COVID-19 | 68,913 visits | All staff | NA | NA | NA |
Abbreviations: NA- Not applicable; F- female; M- male; SD- standard deviation; UK-United Kingdom; USA-United States Of America.
3.3. Methodological quality of the included studies
The quality assessment process of the studies that had a specific study design (66.65%) showed that 43.75% had a good quality (satisfied 75% or more of the methodological quality criteria), 50% had a moderate quality and the rest (6.25%) had poor quality (Table 1).
3.4. Interventions to address mental health issues of HCWs during infectious disease outbreaks
Considering their content (Table 2 ), interventions implemented to address mental health issues in HCWs during pandemics/epidemics were grouped into four categories: informational support, instrumental support; organizational support; emotional and psychological support.
Table 2.
Interventions implemented to address mental health issues of HCWs during different infectious disease outbreaks and their effectiveness.
| Study, year | Intervention | Disease | Setting | Duration | Mental health indicators (or factors) targeted | Psychometric instruments/Tools used | Efficacy measurement |
|---|---|---|---|---|---|---|---|
| Chen et al., 2006 |
|
SARS | largest SARS designated treatment hospital in Taiwan | 3 months | Anxiety, Depression, Sleep Quality | Zung's self-rating anxiety scale; Zung's self-rating depression scale, Pittsburgh sleep quality index |
2 weeks, 1 month and 3 months after the implementation, anxiety, depression and sleep quality were significantly better: Anxiety: (z = −2:68; p = 0.075); (z = −4:45; p < 0.0001); (z = −6.58; p < 0.0001. Depression: (z = −4:58; p < 0.0001); (z = −4:80; p < 0.0001); (z-6:37; p < 0.0001). Seep quality (z = −2:79; p < 0.0053) (z = −3:14; p = 0.0017) (z = −3:37; p = 0.0008). |
| Aiello et al., 2011 | Resilience training on:
|
Influenza A H1N1 | Mount Sinai Hospital | 5 months | Stress, interpersonal isolation, perceived mistrust, fear, concern for family health, social isolation, support barriers. | A five-point Likert scale to evaluate the statements of the participants in a post-session feedback surveys. | Before the intervention, 35% of the staff did not feel prepared to deal confidently with the pandemic After the intervention, 76% felt more confident |
| Waterman et al., 2018 | A group-based intervention, delivered by peers: Phase 1: 2-h workshop on Psychological First Aid. Phase 2: 2-h workshop on psycho-education, coping strategies Phase 3: low-intensity CBT programme on behavioral activation, minimising avoidance, problem solving and coping with anxiety. |
Ebola | Six Ebola Treatment Centres in Sierra Leone |
November 2014–July/August 2016 | Stress, sleep, anxiety, depression, relationship difficulties, behavioral changes (such as anger or substance use) and post-trau-matic stress disorder | Post-Traumatic Stress Checklist – Civilian version; Perceived Stress Scale; Insomnia Severity Index; Generalised Anxiety Disorder 7; Patient Health Questionnaire 9; Relationship Questionnaire Dimensions of Anger Reaction, Alcohol Use Disorders Identification Test-C. |
From phase 1 to end of phase 3, the items on Wellbeing Screening Measure significantly improved: stress (F (3, 51) = 7.89; p < 0.01); depression (F (3, 84) = 11.68; p < 0.01); anxiety (F (3, 78) = 3.40; p < 0.05); behaviouur (F (3, 84) = 6.08; p < 0.01); relationships (F (3, 69) = 3.72; p < 0.05). There were no significant differences in sleep. |
| Schreiber et al., 2019 | A PsySTART tool:
|
Ebola | West Africa Ebola Treatment Centres | 2 months | Post-Traumatic Stress Disorder, Depression. | Anticipate, Plan, and Deter Responder Risk and Resilience model; PsySTART-R self-triage system. | NA |
| Blake et al., 2020 | A digital learning package on:
|
COVID-19 | Hospital | February and March 2020 | Long-term stressors risks | Dedicated questionnaire | 82% have used the information provided in their activities, 100% anticipated they would use it in the future. |
| Maunder et al., 2003 |
|
SARS | Mount Sinai Hospital | March 2003 | Anxiety, Sleep Quality, isolation issues | NA | NA |
| Maunder et al., 2010 |
Computer-assisted resilience training: Relaxation skills with audio modules |
Influenza A H1N1 | Mount Sinai Hospital | September 2008 to January 2009 | Confidence in support and training, pandemic-related self-efficacy, coping style and interpersonal problems | Dedicated questionnaire |
Confidence in support and training: Md 1.1 p < 0.001; Interpersonal problems: Self-centered −0.1 p = 0.01 Cold-distant −0.1 p = 0.10; Socially inhibited −0.2 p = 0.001; Nonassertive −0.2 p = 0.001; Self-sacrificing −0.2 p < 0.001; Overly accommodating −0.2 p < 0.001; Intrusive-needy −0.1 p = 0.003 Total problems −3.7 p < 0.001. Ways of coping: Problem-solving −0.1 p = 0.95 Seeking support −0.1 p = 0.40 Escape-avoidance −0.1 p = 0.06 |
| Khee et al., 2004 | Group session therapies | SARS | Hospital | March-May 2020 | Emotions externalization | NA | NA |
| (Geoffroy et al., 2020) | A psychological assistance hotline:
|
COVID-19 | Assistance Publique –Ho^pitaux de Paris, | 26 days | Anxiety, worry, exhaustion, trauma reactivation insomnia, anger depression, psychotic symptoms | NA | NA |
| Buselli et al., 2020 |
|
COVID-19 | Hospital | Starting March 25th, 2020 | Depression, Anxiety | The Beck Depression Inventory- II; The State-Trait Anxiety Inventory; The Trait Anxiety Scale |
NA |
| Cai et al., 2020 |
|
COVID-19 | Renmin Hospital of Wuhan University | January 29-February 28 | Anxiety, Depression, Insomnia, Post-Traumatic Stress Disorder | Generalised Anxiety Disorder Questionnaire; Patient Health Questionnaire; Insomnia Severity Index; Impact of Events Scale-Revised. |
Value of online psychological information (Yes vs No) in:
|
| Zhou et al., 2020 | Personalized emergency training in:
|
COVID-19 | Emergency isolation wards of COVID-19 | January 24, 2020 to February 28, 2020 | Anxiety, Depression | Comparison before and after the training:
|
The training improved the rescue ability of nurses and effectively avoid the occurrence of cross infection; Psychological conditions before and after:
|
| Sockalingam et al., 2020 | ECHO Ontario Mental Health Program:
|
COVID-19 | Hospital | March 2020 | NA | A 10-question survey of participants' perceived risk of COVID-19 and a five-item self-efficacy measure. | NA |
| Gonzalez et al., 2020 |
|
COVID-19 | Hospital | 7 weeks | Post-Traumatic Stress Disorder | Employee Assistance Program | Within 7 weeks of opening, the respite area has had over 10,000 visits. Employees interviewed noted positive experiences that have contributed to their sense of well-being |
| Donnelly et al., 2020 |
|
COVID-19 | Hospital | NA | Stress | PICU Peer Support team | NA |
| Ping et al., 2020 | The ultra-brief psychological interventions:
|
COVID-19 | Hospital | NA | Stress, Anxiety | UBPI | NA |
| Cheung et al., 2020 | Standardized scenario-based simulation training materials | COVID-19 | Hospital | February 05, 2020 to March 18, 2020 | Personal Strength including: i) assertiveness, ii) mental preparedness, iii) self-efficacy, iv) internal locus of control, v) internal locus of responsibility. | Validated questionnaires measured on a 5-point Likert scale. | All domains of personal strengths were scored 4.24 or above and statistically significantly increased when comparing with reference population (p < 0.001). |
| Albott et al., 2020 | The intervention is organized into 3 levels of support:
|
COVID-19 | Hospital | NA | Stress, anxiety | NA | NA; to be conducted |
| Cole et al., 2020 | Homerton Covid Psychological Support - An online portal to receive self- or signposted referrals. 3 phases: Phase 1: ‘screening and psychological first aid’; Phase 2: CBT-based interventions; Phase 3: a ‘screen and treat’ approach, for HCW with persistent difficulties after phase 1 and 2 |
COVID-19 | Hospital | NA | Distress and any mental health problem | Patient Health Questionnaire-9, the Generalised Anxiety Disorder-7, the Work and Social Adjustment Scale, The Traumatic Screening Questionnaire |
NA; to be conducted |
| Feinstein et al., 2020 | The Healthcare Worker Mental Health COVID-19 Hotline, providing crisis counselling | COVID-19 | Hospital | NA | NA | NA | NA |
| Cheng et al., 2020 |
Psychological health support scheme: Five modules, including:
|
COVID-19 | Hospital | 6 weeks | Daily measurement of mood (referred to as a psychometer); positive self-feedback and self-affirmation | The psychometer module: an online, anonymously completed daily mood questionnaire, which includes:
|
The average number of gains reported by HCWs increased rapidly from a starting point of 0.75 to above 1.0 with the implementation of the intervention programme. HCW team maintained an overall positive outlook with a Daily Mood Index mainly between 7 and 9 out of 10 for nearly 6 weeks of continuous working. |
| Giordano et al., 2020 |
|
COVID-19 | Designated Coronavirus Unit of the University Hospital of Bari |
5 weeks | Stress, anxiety, sadness, fear, tiredness, worry | MusicTeamCare-Q1 to investigate the effects of receptive MT intervention to reduce stress and improve wellbeing |
The differences between T0 and T1 in the intensity of indicators:
sadness (t = 6,432, df = 20, p < 0,05), fear (t = 9,735, df = 20, p < 0,05) and worry (t = 5,056, df = 20, p < 0,05).
and worry (t = 6,190, df = 20, p < 0,05)
|
| Hong et al., 2020 |
|
COVID-19 | Hospital | February 6 to March 28, 2020 | Stress | Chinese versions of the Impact of Event Scale-Revised, and the Sources of Stress Questionnaire | NA |
| Mira et al., 2020 | A digital tool called “Be + against COVID”, providing support resources |
COVID-19 | Online Platform: Website and a mobile App | Ongoing From March 2020 | Any mental health issue | “Self-assessment on the ability to cope the COVID-19 crisis,” presented a 10-question test that tried to assess whether the HCWs were overwhelmed. |
NA |
Abbreviations: CBT- Congnitive Behavioral Therapy; HCWs- health care workers; NA- Not applicable; Mean difference (Md) SAS : self rating anxiety scale; SDS- self rating depression scale- Mean difference; SAS- self rating anxiety scale; SDS- self rating depression scale.
Information support on the pandemic/epidemic was defined as any intervention designed to provide appropriate dissemination of information to HCWs regarding the disease, diagnosis, treatment, and prevention. Instrumental support mechanisms were defined as interventions aimed to protect workers from physical exposure to infectious disease and provide training on PPE's use and disinfection. Organizational support was defined as any intervention aimed to change resources, the working environment, work tasks and/or working hours/methods.
Finally, emotional and psychological interventions were those targeting specifically and directly the emotions and psychological status of HCWs.
3.4.1. Informational support
Knowledge regarding the infection causing the pandemic and its prevention was deemed important for the mental health of HCWs during SARS, in Taiwan (Chen et al., 2006) and Canada, (Aiello et al., 2011; Maunder et al., 2003, Maunder et al., 2010), so in-service trainings were reported as a way to reduce their worries. These trainings included: intensive SARS protection training basic knowledge (Chen et al., 2006; Maunder et al., 2003); masks' removal and disinfection process (Chen et al., 2006); SARS survival guide for medical personnel (Chen et al., 2006); procedures for entering rooms with SARS patients; promotion of SARS protection and isolation; procedures for wearing protective equipment (Chen et al., 2006; Maunder et al., 2010); and hospital SARS infection control (Chen et al., 2006). The Mount Saint Hospital in Canada sent a daily joint email message to all staff, updating SARS information, outlining procedural changes, and providing information about the numbers of patients with SARS, number of staff in quarantine and staff admitted to hospital for treatment (Maunder et al., 2003). Implementing training for the staff and providing information on diagnosis and treatment guidelines, as well as hospital infection guidelines, were considered important in helping mental health of HCWs, also during COVID-19 pandemics, in China and Canada (Cheung et al., 2020; Hong et al., 2020; Sockalingam et al., 2020; Zhou et al., 2020). In Spain, a digital tool called “Be + against COVID” provided an online platform for HCWs to identify and refute unfounded rumours and incorrect information as a way to help mental health of HCWs (Mira et al., 2020).
3.4.2. Equipment and supplies
Several articles reported that the provision of PPEs influences the mental health of HCWs. In Taiwan, gathering sufficient protective equipment and providing training for wearing and removing them, were part of the SARS prevention plan, which had an impact on HCWs’ self-reported levels of anxiety and depression and on sleep quality (Chen et al., 2006). During COVID-19, two Chinese studies have reported how their hospitals have paid special attention to sufficient protection conditions for their staff (Cai et al., 2020; Hong et al., 2020). In a COVID-19 designated clinic in China, HCWs received before rotation training, protective devices, supervision of protection procedures, standardized protection process, which aimed to decrease the worry about their own health and that of their families (Hong et al., 2020). The “Be + against COVID” resources platform in Spain involved professionals in audio-visual messages to broadcast information on guidelines, such as safe removal of PPEs (Mira et al., 2020).
3.4.3. Organizational support
Planning during a pandemic was considered crucial for the mental health of HCWs by several articles. During SARS, a hospital in Canada, implemented a command centre, paying attention to good leadership and teamwork (Maunder et al., 2003). The establishment of a Psychosocial Pandemic Committee (PPC) was also a component of Influenza AH1N1 pandemic planning (Aiello et al., 2011). Pandemic planning needs to promote informative leadership, transparency, realism, and positive messages, as well as deal with the volume of delayed health care activities to support HCWs’ mental health (Mira et al., 2020).
A special attention was paid to manpower allocation during SARS, in Taiwan (Chen et al., 2006) and to adjustments of the working hours in a designated COVID-19 hospital in China (Hong et al., 2020). The latter provided also training, inspection and supervision for its staff (Hong et al., 2020).
Several hospitals had gone through the reorganization of healthcare facilities in order to ensure safer and healthier environments for HCWs. During SARS, hospitals in China provided general isolation rooms to handle procedures for SARS cases (Chen et al., 2006). During COVID-19, several hospitals reorganized their spaces to provide HCWs with rest areas (Donnelly et al., 2020; Gonzalez et al., 2020; Mira et al., 2020). In the USA, a 10-bed pediatric unit was converted to an employee rest area providing a place to rest, shower, receive emotional support, and reenergize with snacks and beverages and aromatherapy, soothing music and TV (Gonzalez et al., 2020). In UK, another hospital created a safe and supportive environment for staff to rest, have tea and eat, as well as a “Take a Minute” room with recliner chair, mental health resources, well-being information and pamphlets and links to psychology support (Donnelly et al., 2020). Furthermore, hospitals in Italy (Giordano et al., 2020) and China (Hong et al., 2020) supported HCWs by offering accommodation, to prevent the risk of contagion in their families. In a COVID-19 designated hospital in China, after 2–3 weeks of continuously working, HCWs were quarantined and convalesced in a vocational resort (Hong et al., 2020).
Mount Sinai Hospital in Canada organized a drop-in support centre with soothing music, snacks and psychiatric staff to help HCWs cope with the mental burden of SARS (Maunder et al., 2003).
3.4.4. Emotional and psychological interventions
3.4.4.1. Psychoeducation and training
Education and training about mental health symptoms were considered of utmost importance to maximize the HCWs' resilience through effective preparation during pandemics.
Occupational therapists at a Canadian hospital developed a pamphlet with the signs of anxiety and stress, and with information about support resources, that was distributed to every nursing unit that received patients with SARS (Maunder et al., 2003). At the same hospital, based on the experience learned from SARS, 156 HCWs received, during Influenza A H1N1, a computer-assisted resilience training, through mixed teaching modalities. Normal stress response, psychological first aid, coping approaches, active listening and personal resilience were addressed in several audio and video mini-lectures, printed fact sheets and onscreen notes. Relaxation skills were taught with audio modules and the gained knowledge was reinforced by quizzes and games (Maunder et al., 2010). In-attendance training on normal stress responses, stress symptoms and signs, anticipated stressors, effective coping strategies and the value of personal and organizational resilience (Aiello et al., 2011) was provided also during Influenza A H1N1 to 1250 Canadian healthcare workers. A resilience plan was used during Ebola to understand and manage psychological impact in HCWs. The training offered in the pre-incident period explains the nature and impact of stressors and provides images of a hospital disaster response, enabling participants to create individualized resilience plans (Schreiber et al., 2019). Posters with wellness tips and strategies for mental health protection for all the staff were used also during COVID-19 in Italy (Buselli et al., 2020) and USA (Gonzalez et al., 2020). Daily mood broadcast, with positive self-affirmation training was created based on the level of self-reporting emotions, and was sent every evening to the medical team online chat group to reinforce their self-affirmation during COVID-19 in China (Cheng et al., 2020).
3.4.4.2. Mental health support team, peer support and counselling
Mental health teams, consisting of psychiatrists, social workers, psychological counselors, or psychiatric nurses, have been established to psychologically support HCWs and to provide counselling according to their needs. A mental health team offered advices and support to the staff in Taiwan (Chen et al., 2006) and Canada (Maunder et al., 2003) during SARS, and group session therapy in Singapore (Khee et al., 2004). During COVID-19 pandemic, as well, several hospitals built up teams to support frontline HCWs. At hospital units in USA, an occupational, physical therapist offered de-stress exercises (Gonzalez et al., 2020), whereas in another hospital a mental health consultant attended unit meetings to understand HCWs activities and concerns and provided additional individual support (Albott et al., 2020). In the latter, peer-group psychological support, in the form of a daily 1-h themed chat group, enabled HCWs to share their emotions and experiences (Albott et al., 2020). A Critical Care Peer-Support Network launched weekly Friday Zoom sessions for “coffee and a chat” in UK and laminated wall poster with positive messages (Donnelly et al., 2020).
In China, a weekly Balint group activity, leaded by a psychiatrist, enabled HCWs to discuss about their emotions and share solutions; and an after-work support team offered assistance to HCWs and organized different after-work social activities (Cheng et al., 2020). Nurses received online counselling, along with on-site psychological support and mindfulness decompression (Zhou et al., 2020).
3.4.4.3. Therapy and rehabilitation
Cognitive Behavioral therapy (CBT) enables the participant to understand and change the destructive and disturbing emotions that have negative impacts on behavior. This therapy was offered during Ebola in Sierra Leone to HCWs experiencing anxiety and depression (Waterman et al., 2018), and to the entire staff during COVID-19 in France (Geoffroy et al., 2020) and Italy (Buselli et al., 2020). In Malaysia, during COVID-19, CBT therapy was part of a psychological intervention, including also acceptance and commitment therapy, dialectical behavioral therapy, motivational interviewing, and early intervention program (Ping et al., 2020). CBT was part of a three-phase intervention in UK, that aimed at facilitating the HCWs’ recognition of coping strategies and resilience factors (Cole et al., 2020). Another type of therapy, implemented in Italy was music therapy, that contained three playlists: 1) “breathing playlist” to favor relaxation and reduce anxiety and stress; 2) “energy playlist” to recover energy and support concentration; and 3) “serenity playlist” to release tension and instill calm and peace of mind (Giordano et al., 2020).
3.4.4.4. Digital platform and tele-support
Several digital platforms and support lines have been created during pandemics aiming to provide psychological support and resources that might protect the psychological well-being and prevent injuries of frontline HCWs.
To prevent and address the stress reactions of HCWs, a digital platform, named “Be + against COVID, was developed and was freely accessible. This platform was composed of a website and a mobile app, in three languages: English, Spanish and Portuguese. The website contents included resources, presented as documents, infographics, and videos, useful for HCWs to overcome stress reactions. A mental health hotline was offered providing support by specialized personnel and referral to individual additional counselling. A self-reporting 10-questions test was included to assess acute stress and based on the results recommendations and guidelines were proposed. The app was structured in three modules: 1) “advices and recommendations”; 2) “self-assessment on the ability to cope the COVID-19 crisis,” and 3) visit the website (Mira et al., 2020). Another mobile-web-based application called “PsySTART-Responder Self Triage System” prompted HCWs to complete a daily self-assessment during Ebola, provided confidential feedback and encouraged the use of a personal resilience plan (Schreiber et al., 2019).
A digital learning package was developed in UK focusing on psychological impacts of COVID-19, psychologically supportive teams, communication, social support, self-care, and emotions management, providing coping approaches and information regarding the resources (Blake et al., 2020).
Psychological telephone hotline was available during COVID-19 in France providing assistance by identifying the symptoms, offering adequate responses and referring to additional psychological support if needed, like CBT or specialized psychiatric consultation (Geoffroy et al., 2020).
In USA, COVID-19 mental health counselling was offered to HCWs by a “24 h/7 Mental Health COVID-19 Hotline” (Feinstein et al., 2020) and to both, HCWs and their families by a “Centralized Support Helpline” (Gonzalez et al., 2020). A confidential telephone support line was also offered to all hospital staff during SARS in Canada, particularly for those in quarantine, creating an informal network of phone support (Maunder et al., 2003).
Tele-education programs focusing on mindfulness exercise, COVID-19 information resources, case-based discussion on stress management skills, and reflection exercises were also provided weekly in Canada (Sockalingam et al., 2020).
3.5. Efficacy of interventions
Even though all the articles included in the systematic review reported implemented interventions, only seven articles (29%) provided data on their effectiveness. Two weeks, one month and three months after the implementation of a SARS prevention program in Mount Sinai Hospital, anxiety, depression, and sleep quality among HCWs were significantly better (Chen et al., 2006). A Computer-assisted resilience training implemented in this hospital during influenza A H1N1 was successful in improving confidence in support and training (Before and after intervention Mean difference = 1.1 p < 0.001); pandemic self-efficacy (Before and after intervention Mean difference = 5.1 p < 0.001); and ways of coping and interpersonal problems (Before and after intervention Mean difference = −3.7 p < 0.001) (Maunder et al., 2010). At the same hospital, a higher proportion of participants (76% vs 35%) felt more confident to cope with the influenza A H1N1 pandemic after a resilience training on influenza information, normal stress responses, anticipated stressors, reinforces principles of coping and the value of organizational and personal resilience (Aiello et al., 2011).
A group-based intervention based on psycho-education and simple CBT principles, delivered by peers in Six Ebola Treatment Centres in Sierra Leon resulted efficient in improving stress (F (3, 51) = 7.89; p < 0.01), depression (F (3, 84) = 11.68; p < 0.01), anxiety (F (3, 78) = 3.40; p < 0.05), behavior (F (3, 84) = 6.08; p < 0.01) and relationships (F (3, 69) = 3.72; p < 0.05) among HCWs, while there were no significant differences in sleep (Waterman et al., 2018).
The online psychological information, offered by Renmin Hospital of Wuhan University during COVID-19, improved insomnia [Yes vs No OR = 1.507 (1.162–1.955)], Post-traumatic stress disorder (PTSD) [Yes vs No OR = 1.556 (1.155–2.097)] and anxiety [Yes vs No OR = 1.325 (1.020–1.721)], while the sufficient protection conditions had a positive impact on PTSD (Cai et al., 2020).
Personalized training including COVID-19 diagnosis and treatment guidelines, hospital infection guidelines, diagnosis and treatment plan, operation of common medical protective equipment, online and on-site psychological counselling and mindfulness decompression among nurses working in emergency isolation wards of COVID-19 in China was found efficient in improving the rescue ability of nurses and avoiding the occurrence of cross infection. The Self-Rating Anxiety Scale score decreased after training (p = 0.019), while there was no statistical difference in Self-Rating Depression Scale (p = 0.306) (Zhou et al., 2020).
A scenario-based simulation training implemented in a hospital in China during COVID-19 significantly increased Personal Strength of HCWs including: assertiveness, mental preparedness, self-efficacy, internal locus of control, and internal locus of responsibility [all scored 4.24 in Likert scale 1–5 (p < 0.001)] (Cheung et al., 2020).
Music Therapy, offered to the staff of a designated Coronavirus Unit of the University Hospital of Bari, Italy through three different playlists (Breathing Playlist, Energy Playlist and Serenity Playlist) improved their mental health status. The Breathing Playlist significantly decreased the intensity of perceived sadness (t = 6,432, df = 20, p < 0,05), fear (t = 9,735, df = 20, p < 0,05) tiredness (t = 7,695, df = 20, p < 0,05), and worry between T0 and T1 (t = 5,056, df = 20, p < 0,05). The Energy Playlist significantly decreased tiredness (t = 4,873, df = 20, p < 0,05), sadness (t = 8,545, df = 20, p < 0,05), fear (t = 6,419, df = 20, p < 0,05), and worry (t = 6,190, df = 20, p < 0,05), while the Serenity Playlist had a positive impact on sadness (t = 4,614, df = 11, p = 0,001), fright (t = 7,707, df = 11, p = 0,000), and worry (t = 2,956, df = 11, p = 0,013) (Giordano et al., 2020).
The psychological health support scheme during COVID-19 in China, which included a daily measurement of mood, a daily mood broadcast with positive affirmation, an online peer-group activity, Balint groups and an after-work support team, enabled the staff to have an overall positive outlook. They reported a daily mood index between 7 and 9 out of 10, for six weeks of continuous work. The average number of self-reports of life-related gains (gain-work, gain-life and gain-physiology) increased rapidly from 0.75 to above 1.0 and were significantly associated to the daily mood index, which reflects the effectiveness of the intervention programme (β = 0.452; p < 0.01) (Cheng et al., 2020).
4. Discussion
This systematic review aimed to identify and summarize the interventions implemented during infectious disease outbreaks to deal with mental health issues of HCWs and report their effectiveness. We identified twenty-four articles which described interventions implemented by different healthcare structures/facilities, to prevent or reduce mental health problems of HCWs during SARS, Ebola, Influenza A H1N1 and COVID-19. The identified interventions concerned four main categories: 1) informational support, 2) instrumental support; 3) organizational support; and 4) emotional and psychological interventions. However, only 37.5% of the included articles reported data on the effectiveness of the implemented interventions. Most articles described the experience of high-income countries, with regard to COVID-19, and addressed all healthcare staff.
While the psycho-emotional interventions targeted directly specific mental symptoms such as stress, depression, PTSD, anxiety, behavioral changes or psychotic symptoms, the interventions reported in the other three categories (informational, instrumental, and organizational) targeted perceived mistrust, fear, confidence in support and training, pandemic-related self-efficacy, personal strength, tiredness or worry, which could be intermediate psychological factors for well-being and mental health. Creating feelings of safety, providing reliable and timely information, along with organizational support have been previously acknowledged in literature as ways to improve the resilience and well-being of HCWs, with the final aim of protecting their mental health (Huey and Palaganas, 2020).
The organizational-level interventions, promoting leadership and teamwork (Maunder et al., 2003) and paying special attention to manpower allocation (Chen et al., 2006), adjustments of the working hours (Hong et al., 2020), have been reported as interventions that ensure safer and healthier environments, help the staff feel better and calmer and promote mental health wellbeing among HCWs (Gray et al., 2019). Organizational interventions to improve HCWs’ mental health were also reported by a Cochrane review, which concludes that changing work schedules can reduce stress, but other organizational interventions have no clear effects (Marine et al., 2006). The importance of interventions targeting organizational structures to prevent or reduce negative mental health impacts on healthcare workers during the COVID-19 pandemic was also acknowledged by a rapid systematic review (Muller et al., 2020), published while our systematic review was ongoing. This rapid review addressed a variety of outcomes, including six studies that reported the implementation of interventions to prevent or reduce mental health problems during COVID-19 pandemic. The authors argue that a focus on individual risk and resilience factors alone, without considering system-level factors, could hinder the discovery of underlying organizational faults, which could be important target for impactful interventions (Muller et al., 2020). We add to this work the results of studies conducted during other infectious disease outbreaks, which could provide valuable insights and lessons to address this issue during the current pandemic.
Providing sufficient PPEs to HCWs reduced the levels of anxiety and depression and improved sleep quality (Chen et al., 2006) and decreased the worry about their own health and that of their families (Hong et al., 2020). In line with this, many staff members of the Second Xiangya Hospital of Central South University stated that they did not need a psychologist but needed more rest without interruption and enough protective supplies. Clear communication of directives/precautionary measures were seen by HCWs themselves as fundamental factors to help reduce mental health problems (Chan and Chan, 2004), reporting that the more they learned about the disease the safer they felt among each other and to be near their families (Feinstein et al., 2020).
Psycho-emotional interventions, including psychological education and training (Aiello et al., 2011; Buselli et al., 2020; Maunder et al., 2003, 2010; Schreiber et al., 2019), therapy (Buselli et al., 2020; Cole et al., 2020; Geoffroy et al., 2020; Ping et al., 2020; Waterman et al., 2018), counselling, team and peer support (Albott et al., 2020; Chen et al., 2006; Gonzalez et al., 2020; Khee et al., 2004; Maunder et al., 2003; Zhou et al., 2020), offered in attendance or through online platforms, deemed important to foster the HCWs resilience during pandemics/epidemics. Our findings are in line with the literature, that identified resilience workshops, group problem solving, cognitive behavioral training, mindfulness training and their combination, as the main psycho-emotional education interventions to develop resilience among HCWs (Huey and Palaganas, 2020; Rogers, 2016). Another systematic review and meta-analysis showed that mindfulness-based interventions have the potential to reduce stress among HCWs (Burton et al., 2017). However, there is no evidence on therapeutical interventions based on dynamic interpersonal techniques. Colleague sessions have been reported to create a sense of personal wellbeing and mutual learning, through sharing with others, which helps HCWs become aware of their emotions and accept them (Feinstein et al., 2020). Nevertheless, the implementation of psychological intervention services may face barriers, as medical staff may be unwilling to participate. This has been reported during COVID-19 pandemic in China where front-line nurses refused any psychological help and stated that they did not have any problems, even though they showed excitability, irritability, unwillingness to rest, and signs of psychological distress (Chen et al., 2020).
The large burden of mental illness, often exacerbated by stigma and discrimination, may delay help-seeking also among HCWs (Clement et al., 2015). Furthermore, the prevalence of new psychiatric symptoms manifesting in hospital workers during infectious disease outbreaks, could be underestimated because of the absence of standardized evaluation (Sockalingam et al., 2020). Considering that, designing and implementing interventions that expect HCWs to ask for help may not be much effective. In this regard, the support systems initiated by higher levels could play a crucial role in recognising the individual struggles and providing a timely response.
Interventions at the facility or higher levels could be an important resource for HCWs’ mental health, who in fact identify multiple support systems, including their hospitals, colleagues, families, friends, and society. With logistical support from their hospital and peer support and encouragement among colleagues, HCWs report a sense of safety and feel they are not alone (Liu et al., 2020). These interventions should include all departments, not only frontline HCWs, considering the numerous non-frontline workers that were affected by the COVID-19 pandemic (Sockalingam et al., 2020). Moreover, these interventions should be able to identify and support at-risk HCWs who may be predisposed to stress reactions because of lower initial resilience, inadequate or inappropriate coping, or exposure to atypically high levels of risk (Zhou et al., 2020). When choosing the adequate intervention, barriers and facilitators should be considered. Based on a recently published Cochrane review factors that could hinder the implementation of these interventions include frontline workers, or the organizations in which they worked, not being fully aware of what they needed to support their mental well-being; and a lack of equipment, staff time or skills needed for an intervention. On the other hand, factors that could facilitate their implementation include: interventions that could be adapted for local needs; having effective communication, both formally and socially; and having positive, safe and supportive learning environments for frontline workers (Pollock et al., 2020).
Among the included articles, only 37.5% reported the efficacy of the implemented interventions on HCWs’ mental health. Given the limited number of articles on the effectiveness of all the interventions it was not possible to quantitatively analyse it. Furthermore, most articles described bundle interventions, so it was not possible to identify the single intervention that was successful in preventing or reducing mental health problems among HCWs during infectious disease outbreaks. Considering that there is a lack of high-quality, well-designed studies, this systematic review highlights the need for further research that evaluate the effectiveness of different interventions implemented to prevent or reduce mental health problems in HCWs during infectious disease outbreaks. Given that the majority of studies were conducted in high-income countries, future articles should also address the interventions in low-and-middle-income countries, which might be influenced by economic and socio-cultural factors. Another gap in the research evidence, identified by our systematic review, is the lack of randomized controlled trials, which if conducted properly could provide important results on the effectiveness of the interventions. Moreover, facilitators and barriers to the implementation of these interventions should be identified and considered in the pandemic planning process. There is the need to evaluate the interventions provided in usual care, in order to understand whether these interventions could be applicable also during epidemics/pandemics outbreak.
The results of this systematic review should be considered in the light of some limitations. First, it may not be generalizable, considering the fact that these interventions may be context-specific and may vary on the country's economic, social and cultural background as well as healthcare system (Tartaglia et al., 2020). Furthermore, included articles enrolled convenience samples or voluntary response samples which could be a font of bias. A publication bias may be present, since we only included peer-reviewed articles published in English. Furthermore, considering the load of articles published on the current pandemic it is possible that we might have missed a certain number of articles. Among the included articles, 33.35% did not have a specific study design so their methodological quality could not be assessed. Of those, 87.5% addressed COVID-19 pandemic which is supported by the fact that during this pandemic many studies have been rapidly published, sometimes pushed through peer-review, hence having low methodological quality.
Despite the limitations, this systematic review adds important information to the evidence published so far on the mental health of HCWs during infectious disease outbreaks and provides data that could be timely used, in a moment when HCWs’ mental health management appears to be challenging. Our search strategy, aimed to be as comprehensive as possible, encompassing six different databases, including PsycInfo, for psychological articles, and Cinhal for nurses-related articles, and further extended to reference hand search. Another strength of our review was the broad inclusion criteria for healthcare workers and different infectious disease outbreaks.
The mental health impact on HCWs, during epidemics/pandemics and after, is complex and should be addressed in a sustained way by all governments and healthcare systems, which should design and implement intervention strategies to mitigate its impact in a collaborative and interdisciplinary manner. These interventions should be multi-factorial, considering the four categories reported in our work. Providing information in a timely and correct way, providing sufficient equipment, adjustments of the working hours, manpower allocation and reorganization of healthcare facilities to ensure safer and healthier environments seem to be imperative for the mental health of HCWs. Mental health response of HCWs and the healthcare system capability to appropriately address their needs should be recognized, and an intervention plan should be integrated within the pandemic surveillance program. Data hereby reported might be helpful for the researchers, stakeholders and policymakers for the development of evidence-based sustainable interventions and guidelines, aiming to prevent or reduce the immediate and long-term effect of infectious disease outbreaks on mental health status of all HCWs. Furthermore, the gaps in knowledge identified by this systematic review may lead to targeted and more quickly initiated future research, focusing on RCTs that evaluate the effectiveness of different interventions, considering facilitators and barriers that affect their implementation, in different economic, social and cultural contexts, to address mental health problems of HCWs during infectious disease outbreaks.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
MLDP: Conceptualization, Writing – original draft, Writing – review & editing, conceptualized and designed the work, A first manuscript version was drafted by, critically reviewed the final version. DZ: Conceptualization, Writing – original draft, Writing – review & editing, conceptualized and designed the work, contributed to search strategy, screening and selection process and data extraction, A first manuscript version was drafted by, critically reviewed the final version, conducted data interpretation. IH: Writing – original draft, Writing – review & editing, contributed to search strategy, screening and selection process and data extraction, A first manuscript version was drafted by, critically reviewed the final version, conducted data interpretation. AO: Writing – original draft, Writing – review & editing, contributed to search strategy, screening and selection process and data extraction, A first manuscript version was drafted by, critically reviewed the final version. AV: Writing – original draft, Writing – review & editing, contributed to search strategy, screening and selection process and data extraction, A first manuscript version was drafted by, critically reviewed the final version. LJ: Writing – original draft, Writing – review & editing, A first manuscript version was drafted by, critically reviewed the final version. All authors have read and agreed to the published version of the manuscript.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
Authors would like to thank Ludovica Silvetti for the technical support during the search process.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.02.019.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aiello A., Young-Eun Khayeri M., Raja S., Peladeau N., Romano D., Leszcz M., Maunder R.G., Rose M., Adam M.A., Pain C., Moore A., Savage D., Bernard Schulman R. Resilience training for hospital workers in anticipation of an influenza pandemic. J. Continuing Educ. Health Prof. 2011;31:15–20. doi: 10.1002/chp.20096. [DOI] [PubMed] [Google Scholar]
- Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle buddies: rapid deployment of a psychological resilience intervention for health care workers during the COVID-19 pandemic. Anesth. Analg. 2020:43–54. doi: 10.1213/ANE.0000000000004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bansal P., Bingemann T.A., Greenhawt M., Mosnaim G., Nanda A., Oppenheimer J., Sharma H., Stukus D., Shaker M. Clinician wellness during the COVID-19 pandemic: extraordinary times and unusual challenges for the allergist/immunologist. J. Allergy Clin. Immunol. Pract. 2020 doi: 10.1016/j.jaip.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake H., Bermingham F., Johnson G., Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int. J. Environ. Res. Publ. Health. 2020;17:2997. doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton A., Burgess C., Dean S., Koutsopoulou G.Z., Hugh-Jones S. Stress Heal; 2017. How Effective Are Mindfulness-Based Interventions for Reducing Stress Among Healthcare Professionals? A Systematic Review and Meta-Analysis. [DOI] [PubMed] [Google Scholar]
- Buselli R., Baldanzi S., Corsi M., Chiumiento M., Del Lupo E., Carmassi C., Dell'Osso L., Cristaudo A. Psychological care of health workers during the COVID-19 outbreak in Italy: preliminary report of an occupational health department (AOUP) responsible for monitoring hospital staff condition. Sustainability. 2020;12:5039. doi: 10.3390/su12125039. [DOI] [Google Scholar]
- Cai Z., Cui Q., Liu Z., Li J., Gong X., Liu J., Wan Z., Yuan X., Li X., Chen C., Wang G. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J. Psychiatr. Res. 2020;131:132–137. doi: 10.1016/j.jpsychires.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.O.M., Chan Y.H. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. (Chic. Ill). 2004;54:190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43:215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng W., Zhang F., Liu Z., Zhang H., Lyu Y., Xu H., Hua Y., Gu J., Yang Z., Liu J. A psychological health support scheme for medical teams in COVID-19 outbreak and its effectiveness. Gen. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung V.K.-L., So E.H.-K., Ng G.W.-Y., So S.-S., Hung J.L.-K., Chia N.-H. Investigating effects of healthcare simulation on personal strengths and organizational impacts for healthcare workers during COVID-19 pandemic: a cross-sectional study. Integr. Med. Res. 2020;9:100476. doi: 10.1016/j.imr.2020.100476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopher D.J., Isaac B.T.J., Rupali P., Thangakunam B. Health-care preparedness and health-care worker protection in COVID-19 pandemic. Lung India. 2020;37:238–245. doi: 10.4103/lungindia.lungindia_189_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clement S., Schauman O., Graham T., Maggioni F., Evans-Lacko S., Bezborodovs N., Morgan C., Rüsch N., Brown J.S.L., Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015 doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- Cole C.L., Waterman S., Stott J., Saunders R., Buckman J.E.J., Pilling S., Wheatley J. Adapting IAPT services to support frontline NHS staff during the Covid-19 pandemic: the Homerton Covid Psychological Support (HCPS) pathway. Cognit. Behav. Ther. 2020;13:1–12. doi: 10.1017/S1754470X20000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020 doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly P.D., Davidson M., Dunlop N., McGale M., Milligan E., Worrall M., Wylie J., Kidson C. Well-being during coronavirus disease 2019: a PICU practical perspective. Pediatr. Crit. Care Med. 2020;21:E584–E586. doi: 10.1097/PCC.0000000000002434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein Robert E., Kotara S., Jones B., Shanor D., Nemeroff C.B. A health care workers mental health crisis line in the age of COVID‐19. Depress. Anxiety. 2020;37:822–826. doi: 10.1002/da.23073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffroy P.A., Le Goanvic V., Sabbagh O., Richoux C., Weinstein A., Dufayet G., Lejoyeux M. Psychological support system for hospital workers during the covid-19 outbreak: rapid design and implementation of the covid-psy hotline. Front. Psychiatr. 2020;11 doi: 10.3389/fpsyt.2020.00511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano F., Scarlata E., Baroni M., Gentile E., Puntillo F., Brienza N., Gesualdo L. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: a preliminary study. Arts Psychother. 2020;70:101688. doi: 10.1016/j.aip.2020.101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A., Cervoni C., Lochner M., Marangio J., Stanley C., Marriott S. Supporting health care workers during the COVID-19 pandemic: mental health support initiatives and lessons learned from an academic medical center. Psychol. Trauma Theory, Res. Pract. Policy. 2020;12 doi: 10.1037/tra0000893. [DOI] [PubMed] [Google Scholar]
- Gray P., Senabe S., Naicker N., Kgalamono S., Yassi A., Spiegel J.M. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: a realist review. Int. J. Environ. Res. Publ. Health. 2019 doi: 10.3390/ijerph16224396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong X., Cao J., Wei J., Duan Y., Zhao X., Jing J., Jiang Y., Geng W., Zhu H. The stress and psychological impact of the COVID-19 outbreak on medical workers at the fever clinic of a tertiary general hospital in beijing: a cross-sectional study. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3566244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huey C.W.T., Palaganas J.C. What are the factors affecting resilience in health professionals? A synthesis of systematic reviews. Med. Teach. 2020;42:550–560. doi: 10.1080/0142159X.2020.1714020. [DOI] [PubMed] [Google Scholar]
- Khee K.S., Lee L.B., Chai O.T., Loong C.K., Ming C.W., Kheng T.H. The psychological impact of SARS on health care providers. Crit. Care Shock. 2004 https://www.researchgate.net/publication/293583989_The_psychological_impact_of_SARS_on_health_care_providers [WWW Document] [Google Scholar]
- Liu ( Q, Yang J., Liu Q., Luo D., Wang X.Q., Phd Y., Yang B.X., Yang Jiong, Liu Qian, Luo Dan, Haase J.E., Guo Q., Wang Xiao Qin, Liu S., Xia L., Liu Z. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob. Heal. 2020;8:e790–e798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatr. Res. 2020 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maben J., Bridges J. Covid-19: supporting nurses' psychological and mental health. J. Clin. Nurs. 2020 doi: 10.1111/jocn.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marine A., Ruotsalainen J., Serra C., Verbeek J. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2006 doi: 10.1002/14651858.CD002892.pub2. [DOI] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ (Can. Med. Assoc. J.) 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Mae R., Vincent L., Peladeau N., Beduz M.A., Hunter J.J., Leszcz M. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv. Res. 2010;10 doi: 10.1186/1472-6963-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell D.N., Perl T.M., Cutrell J.B. “The art of war” in the era of coronavirus disease 2019 (COVID-19) Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mira J.J., Vicente M.A., Lopez-Pineda A., Carrillo I., Guilabert M., Fernández C., Pérez-Jover V., Delgado J.M., Pérez-Pérez P., Vargas A.C., Astier-Peña M.P., Martínez-García O.B., Marco-Gómez B., Bouzán C.A. Preventing and addressing the stress reactions of health care workers caring for patients with COVID-19: development of a digital platform (Be + against COVID) JMIR mHealth uHealth. 2020;8 doi: 10.2196/21692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetc R., Currie M., Lisy K., Qureshi R., Mattis P., Mu P.-F. JBI Manual for Evidence Synthesis. JBI; 2020. Chapter 7: systematic reviews of etiology and risk. [DOI] [Google Scholar]
- Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatr. Res. 2020 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nih, N., n.d. Study quality assessment tools [WWW Document]. URL https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed 11.16.2020).
- O'Sullivan T.L., Amaratunga C.A., Hardt J., Dow D., Phillips K.P., Corneil W. Are we ready? Evidence of support mechanisms for Canadian Health Care Workers in multi-jurisdictional emergency planning. Can. J. Public Health. 2007;98:358–363. doi: 10.1007/bf03405419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ping N.P.T., Shoesmith W.D., James S., Nor Hadi N.M., Yau E.K.B., Lin L.J. Ultra brief psychological interventions for covid-19 pandemic: introduction of a locally-adapted brief intervention for mental health and psychosocial support service. Malays. J. Med. Sci. 2020;27:51–56. doi: 10.21315/mjms2020.27.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock A., Campbell P., Cheyne J., Cowie J., Davis B., McCallum J., McGill K., Elders A., Hagen S., McClurg D., Torrens C., Maxwell M. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane database Syst. Rev. 2020;11 doi: 10.1002/14651858.CD013779. CD013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert R., Kentish-Barnes N., Boyer A., Laurent A., Azoulay E., Reignier J. Ethical dilemmas due to the Covid-19 pandemic. Ann. Intensive Care. 2020 doi: 10.1186/s13613-020-00702-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers D. Which educational interventions improve healthcare professionals' resilience? Med. Teach. 2016;38:1236–1241. doi: 10.1080/0142159X.2016.1210111. [DOI] [PubMed] [Google Scholar]
- Schreiber M., Cates D.S., Formanski S., King M. Military Medicine. Oxford University Press; 2019. Maximizing the resilience of healthcare workers in multi-hazard events: lessons from the 2014-2015 ebola response in Africa; pp. 114–120. [DOI] [PubMed] [Google Scholar]
- Serrano-Ripoll M.J., Meneses-Echavez J.F., Ricci-Cabello I., Fraile-Navarro D., Fiol-deRoque M.A., Pastor-Moreno G., Castro A., Ruiz-Pérez I., Zamanillo Campos R., Gonçalves-Bradley D.C. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J. Affect. Disord. 2020;277:347–357. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sockalingam S., Clarkin C., Serhal E., Pereira C., Crawford A. Responding to health care professionals' mental health needs during COVID-19 through the rapid implementation of project ECHO. J. Continuing Educ. Health Prof. 2020;40:211–214. doi: 10.1097/CEH.0000000000000311. [DOI] [PubMed] [Google Scholar]
- Tartaglia R., La Regina M., Tanzini M., Pomare C., Urwin R., Ellis L.A., Fineschi V., Venneri F., Seghieri C., Lachman P., Westbrook J., Braithwaite J. International survey of COVID-19 management strategies. Int. J. Qual. Health Care. 2020 doi: 10.1093/intqhc/mzaa139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterman S., Hunter E.C.M., Cole C.L., Evans L.J., Greenberg N., Rubin G.J., Beck A. Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. Int. J. Soc. Psychiatr. 2018;64:156–165. doi: 10.1177/0020764017752021. [DOI] [PubMed] [Google Scholar]
- Who Coronavirus Disease COVID-19) Dashboard | WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/ [WWW Document], n.d.
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zace D., Hoxhaj I., Orfino A., Viteritti A.M., Silvetti L., Di Pietro M.L. Mental health interventions in healthcare workers in infectious disease outbreak-A systematic review. Eur. J. Publ. Health. 2020 doi: 10.1093/eurpub/ckaa165.569. [WWW Document] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaka A., Shamloo S.E., Fiorente P., Tafuri A. COVID-19 pandemic as a watershed moment: a call for systematic psychological health care for frontline medical staff. J. Health Psychol. 2020 doi: 10.1177/1359105320925148. [DOI] [PubMed] [Google Scholar]
- Zhou M., Yuan F., Zhao X., Xi F., Wen X., Zeng L., Zeng W., Wu H., Zeng H., Zhao Z. Research on the individualized short‐term training model of nurses in emergency isolation wards during the outbreak of COVID‐19. Nurs. Open. 2020;7:1902–1908. doi: 10.1002/nop2.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.