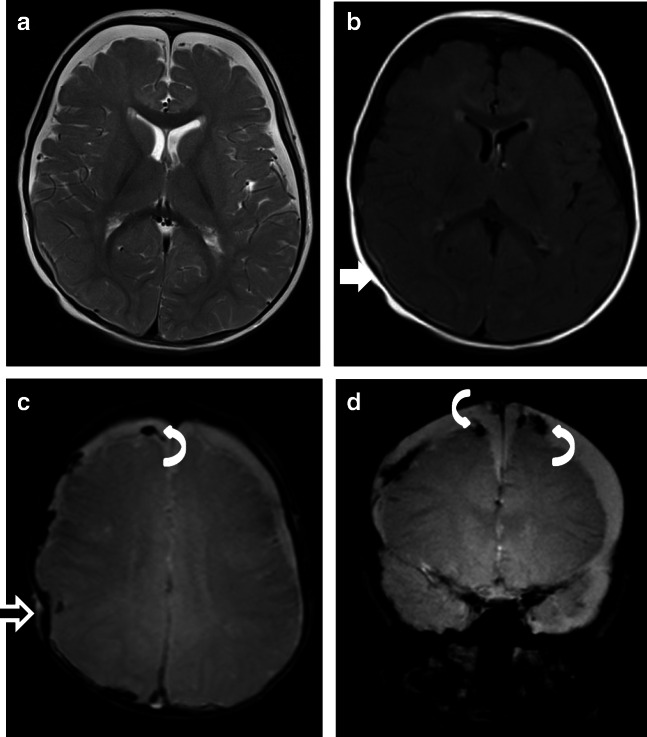
Fig. 5.
Case “NAHT3.” 1 year old. a T2w. b FLAIR. c T2*. d T2* (not available for the neuro and non-neuroradiologists). Anamnesis (not available for the neuro/radiologists): MVA. Toddler on the mother’s lap and not buckled in. MRI findings: acute SDH. Axial T2 shows bilateral SDHs along the hemispheres (a), with the sedimentation of the blood in the dependent portion of the hematoma (b, white straight arrow) indicating that the SDH is from a more recent injury. In addition, the child had SAH, impression fracture of the calvarium (c, black straight arrow), and multiple avulsed and thrombosed cortical veins (c and d). SDH with an interhemispheric high convexity or posterior fossa location and associated thrombosed cortical veins are highly associated with pAHT. In addition, the association with impression fracture made it very difficult to differentiate NAHT from pAHT with impact. The mechanical forces during shaking and a fast acceleration-deceleration injury (toddler in mother’s lap during a car accident) are similar and might explain the MRI mimics. This case emphasizes that the presence of ruptured bridging veins is NOT pathognomonic for pAHT and can happen in cases of severe NAHT. Both groups were very uncertain in this case; 2 neuroradiologists and 2 non-neuroradiologists were not able to rule out pAHT; 1 neuroradiologist and 1 non-neuroradiologist assumed pAHT to be the correct diagnosis