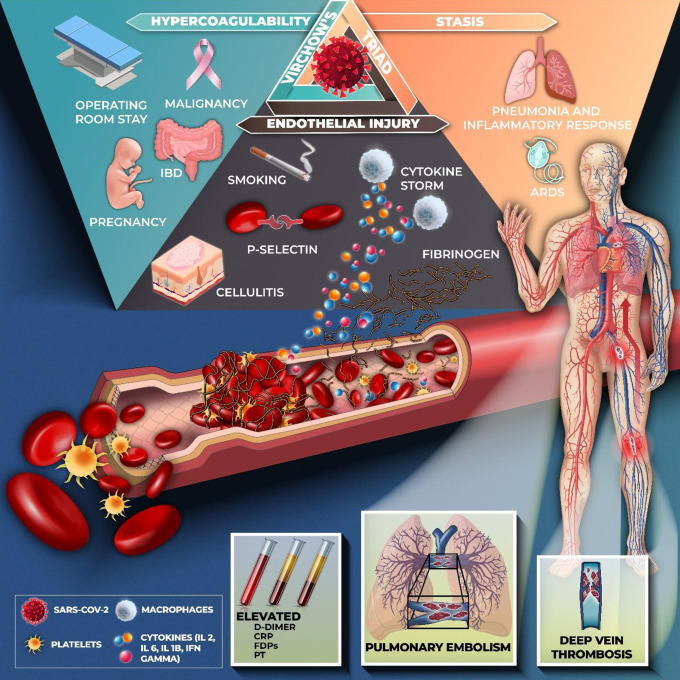
Figure 6.
Postulated pathophysiology of venous thromboembolism and Covid-19. SARS-CoV2 gains entry into the host cell via the ACE-2 receptor which causes inflammation and cytokine storm associated with the release of interleukin-2 (IL-2), interleukin-6 (IL-6), interleukin-10 (IL-10), and tumor necrosis factor-alpha (TNF-α) are released. As a response to viral infection, there is endothelial injury and thrombin formation contributing to a hypercoagulable state. Stasis in critically ill patients with pneumonia and ARDS further contributes to the formation of emboli. Hence, Virchow’s triad drives the development of thrombosis. Down regulation of fibrinolytic and anti-coagulation pathways leads to an increased risk of VTE. Hemostatic abnormalities including elevated levels of d-dimer, C-reactive protein (CRP), fibrin degradation products (FDPs) and prothrombin time (PT) suggesting an underlying coagulopathy process and a high burden of thrombosis.