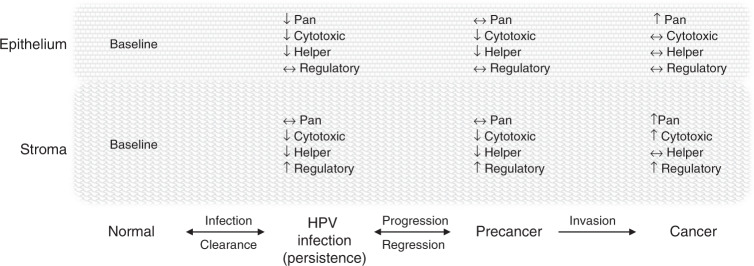
Fig. 3. Conceptual model of infiltrating T-cells in cervical carcinogenesis.
Normal cervical tissue is infiltrated by T-cells and T-cell subsets that respond to infection as part of the adaptive immune response. When HPV infection becomes established and is not immunologically cleared, it evades immune detection with reduced cytotoxic (CD8+) and helper (CD4+) T-cell infiltration in both the epithelium and adjacent stromal tissue. It is unclear whether regulatory (CD25+, FoxP3+) T-cell infiltration is affected but some evidence suggests it begins to increase. When HPV infections persist and progress to cervical precancer, pro-immune T-cell subsets continue to be suppressed and regulatory (inhibitory T-cells) amplified. If the lesion progresses to invasive cancer, a highly immunogenic state is reached with high levels of pan, cytotoxic, and helper T-cells in the surrounding stroma and to some extent in the tumour itself. Regulatory T-cells may be relatively high, resulting in a worse prognosis, or low, resulting in a better prognosis.