Abstract
The current cross-sectional study aimed to explore the relationship between work stressors and mental health in frontline nurses exposed to COVID-19. Participants were recruited from 16 general hospitals in Anhui province from February 2020 to March 2020. The general sociodemographic questionnaire, Nurse Job Stressors Scale, Simplified Coping Style Questionnaire, NEO Five-Factor Inventory, Perceived Social Support Scale, and Kessler Psychological Distress Scale were used in this study. Based on 723 valid questionnaires retrieved (100%), the total mean scores of work stressors and mental health of frontline nurses were (94.38 ± 23.42) and (22.81 ± 7.16), respectively. The results of the structural equation model showed that work stressors had an indirect positive effect (β = 0.484, P < 0.01), social support had a direct negative effect (β = −0.934, P < 0.01), personality traits had a direct positive effect (β = 0.209, P < 0.01), and positive coping style had both direct positive (β = 0.246, P < 0.01) and indirect negative effects (β = −0.873, P < 0.01) on frontline nurses’ mental health. In conclusion, nursing staff can reinforce positive influences by accepting social support, adopting positive coping methods, and weakening negative influences factors to reduce or buffer their negative mental states and further reduce work stress.
Keywords: COVID-19, Caregiver, Job, Mental Health, Psychic suffering, Stress, Work psychology
Résumé
Cette étude transversale vise à explorer la relation entre les facteurs de stress au travail et la santé mentale des infirmières de première ligne exposées au COVID-19. Les participants ont été recrutés dans 16 hôpitaux généraux de la province d’Anhui de février à mars 2020. Cette étude a utilisé des questionnaires sociodémographiques généraux, des échelles de stress professionnels des infirmières, des questionnaires simplifiés sur le style d’adaptation, des échelles à cinq facteurs NEO, des échelles de soutien social perçu et des échelles de détresse psychologique Kessler. Selon les 723 questionnaires valides récupérés (100 %), les scores moyens totaux des facteurs de stress au travail et de santé mentale des infirmières de première ligne sont respectivement de (94,38 ± 23,42) et (22,81 ± 7,16). Les résultats du modèle d’équation structurelle montrent que les facteurs de stress au travail ont un impact positif indirect sur la santé mentale des infirmières de première ligne (β = 0,484, p < 0,01), et que le soutien social a un impact négatif direct sur la santé mentale des infirmières de première ligne (β = −0,934, p < 0,01), les traits de personnalité ont un impact positif direct sur la santé mentale des infirmières de première ligne (β = 0,209, p < 0,01), et les styles d’adaptation positifs ont un impact positif direct sur la santé mentale des infirmières de première ligne (β = 0,246, p < 0,01) et un impact négatif indirectement (β = −0,873, p < 0,01). En résumé, les infirmières de première ligne peuvent réduire ou amortir leur état mental négatif en acceptant le soutien social, en adoptant des styles d’adaptation positifs et en affaiblissant les facteurs d’influence négatifs, afin de réduire la pression au travail.
Mots clés: Covid-19, Psychologie du travail, Santé mentale, Soignant, Souffrance psychique, Stress, Travail
1. Introduction
Since the end of December 2019, pneumonia caused by a new coronavirus (COVID-19) infection has been discovered in Wuhan, Hubei, China and throughout the whole country. To date, the origin of COVID-19 is still unknown. On January 31, 2020, WHO officially recognized the epidemic as an infectious public health emergency of international concern on the basis of on-the-spot investigation in China. The frontline nurses were those who directly participated in clinical activities of treating or providing care to patients with positive COVID-19. As we all know, with increasing number of confirmed and suspected cases of COVID-19, overwhelming workload, lacking personal protection equipment, and feelings of being inadequately supported may contribute to the mental burden of these frontline nurses [13] and cause a series of psychological stress reactions in frontline nurses, including anxiety, depression, insomnia, and fear [10].
Psychological stress is a state of psychological tension resulting from an imbalance between subjects’ objective demands and coping abilities under certain environmental stimuli. A study showed that 85.37% of clinical frontline supporting nurses had adverse emotional reactions, including somatization (21.9%), compulsive symptoms (14.6%), interpersonal sensitivity (26.8%), depression (4.8%), anxiety (39.0%), and fear (51.2%) [26]. Mei's study showed a poor sleeping quality in frontline nurses exposed to new coronavirus pneumonia, and anxiety and high-stress load were risk factors for nurses’ sleeping quality [17]. Frontline medical personnel had not only sleeping disorders but also psychological and stress disorders [20]. A study showed that frontline nurses in Sichuan province had anxiety in response to the epidemic, but the level of anxiety is lower than the national norm [8]. Most nurses had a milder stress response to the crisis stress of the epidemic, with mild impairment in cognition, emotion, and behavior. The epidemic may vary from region to region, leading to slightly different findings.
The psychological stress response of frontline nurses in infectious public health emergencies is affected by various factors, including cognitive evaluation, coping styles, and social support [16]. Nurses who used coping styles to solve problems and actively ask for help usually have a higher score of overall mental health, whereas those who used avoidance coping styles were accompanied by coercion, depression, anxiety, and other symptoms [30]. In terms of the overall level of social support, as well as the endogenous and exogenous support from the family, the higher the level of social support of frontline medical personnel, the better their mental health status [24]. In a word, with the help of social support, nurses’ stress responses can be significantly reduced. Kakemam's study showed that psychological stress was more prominent on frontline nurses dealing with infectious public health incidents [11]. Stressors pass through intermediary factors such as individual cognitive evaluation, coping activities, and social support to further influence an individual's physical and mental health. According to Kakemam's study [11], overworking and caring and treating critically ill patients are the main stressors of frontline nurses. Wheeler et al. [23] found that nursing workload and working environment are the main stressors of frontline nurses. Coyne et al. [4] showed that higher social support is always accompanied by better mental and physical conditions and that maintaining a positive coping style can lead to less susceptibility to the effects of stressful events. However, whether the above factors are effective in predicting the psychological stress response of frontline nurses is unclear. In addition, whether these factors are correlated and how these factors act on the psychological stress response need to be explored.
Therefore, this study aimed to use the stress system model as a theoretical framework to systematically understand the stress states of frontline anti-epidemic personnel from three aspects, namely, stressors, cognitive evaluation, and stress responses, and then established a psychological stress model for analysis.
2. Methods
2.1. Research design
This was a cross-sectional study conducted in Anhui province, China from February 2020 to March 2020.
2.2. Hypothesized model
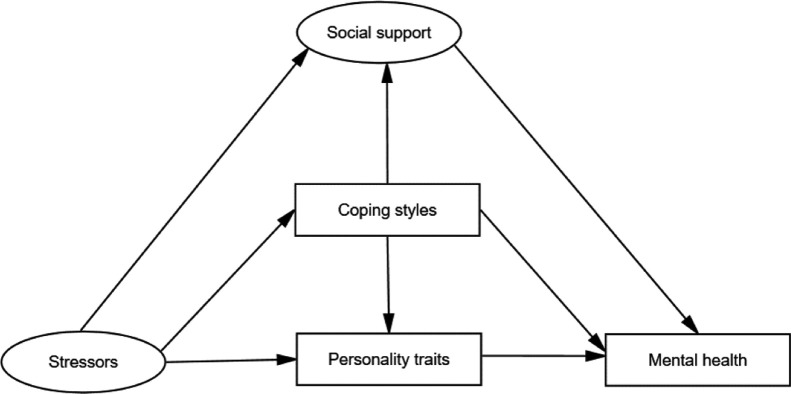
The hypothesized model of this study was derived from stressors-mediation mechanism-stress response. The model assumed that frontline nurses’ work stressors can predict their mental health through the mediation effects of social support, coping styles, and personality traits. Meanwhile, coping styles, social support, and personality traits can be direct predictors of mental health. With the help of this model, we can gain insights into the psychological states of frontline nurses and then take effective measures against poor psychological states. The hypothesized model was presented in Fig. 1 .
Fig. 1.
The hypothesized model.
2.3. Recruitment and data collection
A total of 723 frontline registered nurses were recruited from 16 general hospitals, Anhui province, China. All demographic data were collected using electronic questionnaires. The purpose of this study was explained to participants, and detailed instructions were listed to guide them in filling out the questionnaires. Two researchers collected the data and checked the electronic questionnaire system for IDs; relevant information; and feedback records, such as submission time, fill time, equipment, and IP address to ensure the accuracy of the exported data.
Individuals who hold a certificate of nurse qualification granted by the Ministry of Health PR China and have been working as a registered nurse in a hospital for at least one year were included.
2.4. Ethical considerations
All participants were fully informed about the research purpose and characteristics before they provided signed consent, and they were allowed to drop out the research at any time they desired. The research was anonymous, and confidentiality of information was definitely assured.
Ethical approval was granted from the Clinical Medical Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University (No: Quick-PJ 2020-08-13). This study conformed to the standards of the Declaration of Helsinki.
3. Measurements
3.1. Demographic Questionnaire
The self-designed demographic questionnaire included age, gender, marital status, educational background, years of working, departments, and the relevant content of the COVID-19 prevention work.
3.2. Kessler Psychological Distress Scale (Kessler 10)
Nurses’ mental health was measured with Kessler 10 [12], which has been widely used in international studies. The Kessler 10 contains 10 items: burnout, tension, helplessness, restlessness, lose calmness, without a quality rest, depression, low interest, low competence, and low value. Respondents answered on a Likert-type 5-point scale from 1 (Hardly) to 5 (All the time). The total scores of mental health was categorized as four levels: Good (10–15 points), Normal (16–21 points), Poor (22–29 points), and Bad (30–50 points). In this study, Cronbach's α of this scale was 0.92, which is acceptable.
3.3. Nurse Job Stressors Scale (NJSS)
The NJSS was revised by Li et al. [15] in 2000 based on the studies of Gray-Toft et al. [6] and Wheeler et al. [23]. The NJSS is a 35-item, 4-point Likert scale that measures nurses’ job stressors in five dimensions: problems in nursing profession and work, time allocation and workload, working environment and resources, caring for patients, and management and interpersonal relationships. Respondents answered on a Likert-type 4-point scale from 1 (No stress) to 4 (High stress). Problems in nursing profession and work dimension ranged from 7 to 28, time allocation and workload dimension ranged from 5 to 20, working environment and resources dimension ranged from 3 to 12, caring for patients’ dimension ranged from 10 to 40 and management and interpersonal relationships dimension ranged from 9 to 36, with increasing scores denoting high stress. Cronbach's α of this scale in Li's study was 0.98, which is acceptable.
3.4. Simplified Coping Style Questionnaire (SCSQ)
The SCSQ was revised by Xie et al. [25] in 1998 based on the Ways of Coping Questionnaire (Folkman) [29]. It contained 20 items that measured coping style in two dimensions: positive response and negative response. Respondents answered on a Likert-type 4-point scale from 0 (Don’t adopt) to 3 (Frequently adopt). Cronbach's α of this scale was 0.90, which shows high reliability and validity.
3.5. Perceived Social Support Scale (PSSS)
Nurses’ social support was measured with PSSS [1], which was translated by Jiang et al. [9] in 2001. The PSSS contains 12 items in three dimensions: family support, friends support and other support. Respondents answered on a Likert-type 7-point scale from 1 (Completely disagree) to 7 (Completely agree). Scores for each dimension ranged from 4 to 28, with increasing scores denoting high social support. Cronbach's α of this scale was 0.854, which was reliable and validated.
3.6. NEO Five-Factor Inventory (NEO-FFI)
The NEO-FFI developed by Costa and McCrae in 1992 [3] is a 60-item, 5-point Likert scale that measures nurses’ personality in five dimensions: Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness. Nurses responded on a Likert-type 5-point scale with responses from 1 (Completely disagree) to 5 (Completely agree). However, 27 items were reverse-scored, meaning that higher scores indicate lower psychological stress, interpersonal interaction, independent thinking, reliability and perseverance. The Cronbach's α values of Neuroticism, Extraversion, Openness, Agreeableness and Conscientiousness were 0.77, 0.78, 0.63, 0.72 and 0.74, respectively.
4. Data analysis
Statistical analysis was performed using IBM SPSS and AMOS 23.0® (IBM Corp, Armonk, NY, USA). All data were expressed as mean ± standard deviation unless otherwise specified. Correlation coefficients among nurses’ work stressors, coping styles, social support, personality traits, and mental health were calculated by Pearson correlation analysis. Covariance-based structural equation model (CB-SEM), using maximum likelihood estimation, and path analysis were employed to determine the interrelationships among work stressors, personality traits, coping styles, social support, and mental health. The following parameters were used to evaluate model fit: χ2/df ≤ 5, RMSEA < 0.08, GFI > 0.9, CFI > 0.9, AGFI > 0.9, and IFI > 0.9. The significance level was set at P < 0.05.
5. Results
5.1. Subjects’ General Sociodemographic Characteristics
As shown in Table 1 , the majority of frontline nurses were female (94.7%). More than 87% of the nurses were younger than 39 years old, and more than half were married with 64% having children. More than 77% of nurses had a bachelor's degree or higher as their advanced education. More than 66% of nurses had worked over 6 years, and more than 71% of nurses were ordinary nurses. Approximately 97.5% of nurses volunteered to participate in COVID-19 epidemic prevention; 44.5% of nurses were from other units and most currently work in fever clinics, diagnosis ward, and other units. More than 92% of nurses had received systematical training before participating in COVID-19 epidemic prevention, and 34% had work experiences in epidemic prevention. Approximately 0.4% of nurses had a family member with confirmed or suspected COVID-19 and still participated in epidemic prevention.
Table 1.
Subjects’ general sociodemographic characteristics (n = 723).
| n | % | |
|---|---|---|
| Sex | ||
| Male | 38 | 5.3 |
| Female | 685 | 94.7 |
| Age | ||
| 18–29 years | 285 | 39.4 |
| 30–39 years | 350 | 48.4 |
| 40–49 years | 70 | 9.7 |
| ≥ 50 years | 18 | 2.5 |
| Marital status | ||
| Single | 218 | 30.2 |
| Married | 497 | 68.7 |
| Divorced or widowed | 8 | 1.1 |
| Educational background | ||
| Associate's degree or below | 157 | 21.7 |
| Bachelor's degree | 561 | 77.6 |
| Master's degree or above | 5 | 0.7 |
| Years of working | ||
| ≤ 3 years | 119 | 16.5 |
| 3–6 years | 123 | 17.0 |
| 6–9 years | 155 | 21.4 |
| > 9 years | 326 | 45.1 |
| Technical titles | ||
| Ordinary nurse | 518 | 71.6 |
| Clinical instructor | 87 | 12.0 |
| Head of nursing team | 51 | 7.1 |
| Head nurse | 67 | 9.3 |
| Number of children | ||
| None | 258 | 35.7 |
| 1 | 348 | 48.1 |
| ≥ 2 | 117 | 16.1 |
| Volunteered to participate in COVID-19 epidemic prevention | ||
| Yes | 705 | 97.5 |
| No | 18 | 2.5 |
| Current workplaces | ||
| Fever clinics | 183 | 25.3 |
| Emergency department | 53 | 7.3 |
| Radiology department | 5 | 0.7 |
| Observation ward | 74 | 10.2 |
| Diagnosis ward | 150 | 20.7 |
| Other units | 258 | 35.7 |
| Supported personnel from other units | ||
| Yes | 322 | 44.5 |
| No | 401 | 55.5 |
| Received training before participating in COVID-19 epidemic prevention | ||
| Yes | 672 | 92.9 |
| No | 51 | 7.1 |
| Had work experiences in epidemic prevention | ||
| Yes | 246 | 34.0 |
| No | 477 | 66.0 |
| Had a family member with confirmed or suspected COVID-19 | ||
| Yes | 3 | 0.4 |
| No | 720 | 99.6 |
5.2. Scores of work stressors, personality traits, coping styles, social support, and mental health in frontline nurses
The total score of work stressors was (94.38 ± 23.42), of which the nursing profession and work score was (21.07 ± 5.43), the time allocation and workload score was (15.86 ± 4.38), the working environment and resources score was (8.01 ± 2.93), the caring for patients score was (29.83 ± 7.44), and the management and interpersonal relationships score was (19.62 ± 7.19). The total score of personality traits was (155.56 ± 15.86), of which the neuroticism score was (24.22 ± 7.37), the conscientiousness score was (35.10 ± 5.90), the agreeableness score was (37.52 ± 5.22), the openness score was (30.89 ± 6.30), and the extraversion score was (27.83 ± 6.38). The scores of positive coping style and negative coping style were (24.98 ± 6.42) and (9.68 ± 4.16), respectively. The total score of social support was (64.30 ± 11.91), of which the family support score was (22.17 ± 4.56), the friends support score was (21.59 ± 4.26), and the other support score were (20.54 ± 4.42). The mental health score was (22.81 ± 7.16).
5.3. Correlation coefficients among work stressor, personality traits, coping styles, social support, and mental health
A correlation matrix was prepared before testing the model (Table 2 ). The main correlation analysis showed that significant correlations were present among three factors of social support, five factors of work stressors, two factors of coping ways, five factors of personality traits, and mental health (P < 0.01). However, no significant correlations were found among friends support, openness, extraversion, personality traits, and negative coping (P > 0.05).
Table 2.
Correlation analysis between Work stressors, Personality traits, Coping styles, Social support and Mental health (n = 723, r).
| Mental health | Social support | Family support | Friends support | Other support | Positive coping | Negative coping | Neuroticism | Conscientiousness | Agreeableness | Open ness | Extraversion | Personality traits | WS 1 | WS 2 | WS 3 | WS 4 | WS 5 | Work stressors | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental health | 1.000 | ||||||||||||||||||
| Social support | −0.445** | 1.000 | |||||||||||||||||
| Family support | −0.365** | 0.865** | 1.000 | ||||||||||||||||
| Friends support | −0.401** | 0.918** | 0.713** | 1.000 | |||||||||||||||
| Other support | −0.442** | 0.910** | 0.660** | 0.794** | 1.000 | ||||||||||||||
| Positive coping | −0.382** | 0.598** | 0.498** | 0.577** | 0.550** | 1.000 | |||||||||||||
| Negative coping | 0.261** | −0.115** | −0.118** | −0.062* | −0.132** | 0.110** | 1.000 | ||||||||||||
| Neuroticism | 0.583** | −0.469** | −0.404** | −0.412** | −0.452** | −0.385** | 0.349** | 1.000 | |||||||||||
| Conscientiousness | −0.345** | 0.459** | 0.405** | 0.422** | 0.437** | 0.438** | −0.209** | −0.448** | 1.000 | ||||||||||
| Agreeableness | −0.331** | 0.511** | 0.454** | 0.480** | 0.471** | 0.395** | −0.223** | −0.438** | 0.616** | 1.000 | |||||||||
| Openness | −0.288** | 0.412** | 0.337** | 0.389** | 0.396** | 0.506** | −0.019* | −0.273** | 0.516** | 0.360** | 1.000 | ||||||||
| Extraversion | −0.325** | 0.394** | 0.368** | 0.344** | 0.368** | 0.414** | 0.002* | −0.329** | 0.292** | 0.231** | 0.551** | 1.000 | |||||||
| Personality traits | −0.225** | 0.460** | 0.414** | 0.428** | 0.427** | 0.479** | −0.005* | −0.121** | 0.690** | 0.606** | 0.795** | 0.633** | 1.000 | ||||||
| WS 1 | 0.332** | −0.327** | −0.235** | −0.275** | −0.366** | −0.223** | 0.123** | 0.315** | −0.202** | −0.246** | −0.087* | −0.162** | −0.111** | 1.000 | |||||
| WS 2 | 0.397** | −0.336** | −0.216** | −0.292** | −0.382** | −0.273** | 0.167** | 0.361** | −0.240** | −0.234** | −0.173** | −0.234** | −0.163** | 0.680** | 1.000 | ||||
| WS 3 | 0.370** | −0.333** | −0.274** | −0.295** | −0.328** | −0.178** | 0.194** | 0.338** | −0.202** | −0.237** | −0.120** | −0.191** | −0.133** | 0.501** | 0.591** | 1.000 | |||
| WS 4 | 0.429** | −0.404** | −0.321** | −0.353** | −0.418** | −0.277** | 0.202** | 0.439** | −0.309** | −0.327** | −0.196** | −0.272** | −0.215** | 0.580** | 0.653** | 0.642** | 1.000 | ||
| WS 5 | 0.450** | −0.505** | −0.401** | −0.446** | −0.527** | −0.316** | 0.265** | 0.436** | −0.384** | −.391** | −0.200** | −0.221** | −0.248** | 0.571** | 0.583** | 0.599** | 0.728** | 1.000 | |
| Work stressors | 0.477** | −0.470** | −0.354** | −0.410** | −0.500** | −0.315** | 0.235** | 0.461** | −0.339** | −0.360** | −0.188** | −0.253** | −0.215** | 0.781** | 0.805** | 0.746** | 0.883** | 0.877** | 1.000 |
WS 1 = nursing profession and work problems, WS 2 = time allocation and workload problems, WS 3 = working environment and resources problems, WS 4 = caring for patients problems, WS 5 = management and interpersonal relationship problems.
P > 0.05.
P < 0.01.
5.4. Test of final model and parameter estimates
The model fits the data well (χ2/df = 4.656 < 5, RMSEA = 0.071 < 0.08, GFI = 0.969 > 0.9, AGFI = 0.925 > 0.9, IFI = 0.978 > 0.9, and CFI = 0.978 > 0.9). A fully adjusted model was also tested, and the effects among variables were consistent with the hypothesized model.
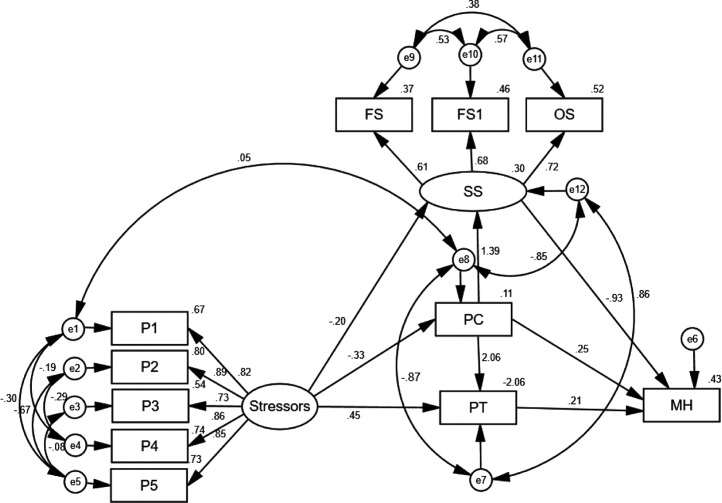
Based on the theoretical framework of stress (stressors-mediation mechanism-stress response), a structural equation model of the relationship between work stressors and mental health in frontline nurses was developed using e1-e13 as indicators of measurement errors. Work stressors were used as an exogenous variable, whereas personality traits, positive coping, social support, and mental health were used as endogenous variables. The final model is presented in Fig. 2 .
Fig. 2.
The final model of work stressors, personality traits, positive coping, social support, and mental health in front-line nurses.
The effect decomposition among work stressors, social support, positive coping, and personality traits on mental health is shown in Table 3 . The results of CB-SEM showed that work stressors had an indirect positive effect (β = 0.484, P < 0.01), social support had a direct negative effect (β = −0.934, P < 0.01), personality traits had a direct positive effect (β = 0.209, P < 0.01) and positive coping style had both direct positive (β = 0.246, P < 0.01) and indirect negative effects (β = −0.873, P < 0.01) on frontline nurses’ mental health.
Table 3.
Effect decomposition among variables in the fitted model (β).
| Dependent variable | Effect decomposition | Independent variable |
|||
|---|---|---|---|---|---|
| Work stressors | Social support | Positive coping | Personality traits | ||
| Mental health | Direct effect | 0 | −0.934 | 0.246 | 0.209 |
| Indirect effect | 0.484 | 0 | −0.873 | 0 | |
| Total effect | 0.484 | −0.934 | −0.626 | 0.209 | |
6. Discussion
Infectious public health events usually have the characteristics of high complexity, low predictability, and large-scale impacts. The COVID-19 epidemic, an unknown, unexpected, and devastating disease, is the most extensive to afflict humanity in a century and poses a grave threat to human life and health. There is no doubt that medical workers play an important role and make great sacrifices in fighting this new virus. In addition, medical workers bear psychological stress in the face of this epidemic. Therefore, we need to understand the mental health state of frontline nurses fighting COVID-19, analyze its influencing factors, and further provide a basis for intervening mental health of frontline nurses.
In general, the mental health of frontline nurses in this study was at a poor level. The prevalence of psychological problems in frontline nurses was 57.8%, which was much higher than in the general population (22%) [28]. Tam et al. [21] showed that the prevalence of depression was 45% in clinical nurses during the period of SARS in 2003, indicating that the epidemic had caused severe mental health problems in nurses. We found that the overall average work pressure in frontline nurses was at a medium level, which is consistent with the findings of Nickell et al. [19]. The difference is that the dimension with the highest pressure source score in this study is caring for patients. COVID-19, which is caused by a new coronavirus infection, mainly transmitted through the respiratory tract and close contact. This disease causes pulmonary inflammation. Frontline nurses worked directly with suspected or confirmed patients and suffered from enormous psychological pressure even if taking precautions in advance. At the same time, wearing a protective suit with other protective equipment at work increases the physical exertion of frontline nurses, which could lead to decreased physical fitness, affect physical and mental health, and tend to cause anxiety and stress [27]. In addition, frontline nurses care for patients for a long time and the working environment is closed, which also increases the risk of transmission of the virus. Most frontline nurses are also worried about transmitting the virus to their family members. Under this pressure, most nurses may suffer from physical and mental health problems without effective adjustment [23]. All these findings suggest that we should pay great attention to the work pressure and mental states of frontline nurses while fighting COVID-19 and timely identify the crux of psychological problems. If necessary, we should also provide psychological crisis intervention to promote nurses’ mental health.
As an uncontrollable objective factor, work stressors can have an impact on nurses’ mental health. The structural equation model of this study showed that work stressors played a role in mental health through the intermediary role of path relationships such as positive coping, personality traits, and social support. This study also found that the above intermediary variables played an important role in the process between work stressors and mental health, verifying the theoretical model of the process of psychological stress: the source-mediating mechanism- theoretical framework of stress response [9]. It suggested that frontline nurses could adjust intermediary variables, such as self-efficacy and coping style to reduce the adverse effects of work stressors on anxiety and depression by taking effective interventions.
Social support can buffer patients’ psychological stress and pressure, help patients improve their emotional experience, and then promote their physical and mental health [7], [22]. Cohen et al. [2] put forward a buffering effect model of social support regulating stress and found that social support can reduce individual perception and evaluation of stress events, as well as their emotional and physiological responses to stress, by providing individuals with positive emotional experiences. As mentioned before, positive social support could provide individuals with more available resources and help them improve positive emotional state. Social support is an important protective factor in regulating stress from the external environment. In this study, frontline nurses’ social support was negatively correlated with their mental health. The structural equation model validated that social support is an important influencing factor of nurses’ mental health. It not only had a direct positive effect on mental health but also acted as an intermediary variable and indirectly affected work stressors. The relationship between positive coping style and mental health proved that social support played an intermediary role in buffering protection while responding to stress [18]. Therefore, caregivers should guide and help patients to establish good interpersonal relationships; encourage them to strengthen communication with others; and reduce the experiences of anxiety and depression by increasing the support of family, friends, medical staff, and others.
Coping styles refer to the coping strategies or methods that individuals can adopt when confronted with different stressors. Different coping styles have different coping outcomes, with reduced or aggravated psychological stress response [14]. In this study, positive coping style was negatively correlated with mental health, whereas negative coping style was positively correlated with mental health. The level of mental health is related to the choice of stress coping styles. Positive coping style could promote the mental health of frontline nurses, whereas negative coping style can be detrimental to their mental health. In this structural equation model, the positive coping style had a direct positive impact on nurses’ mental health, and it could also exert an indirect effect on mental health through the intermediary role of social support. Dunkley et al. [5] stated that the positive coping style referred to adopting a positive attitude and actively seeking help from family and society to reduce nurses’ negative emotional experience. Therefore, hospital managers should focus on stimulating nurses’ potentially positive traits and encouraging them to adopt positive coping styles and social support to reduce adverse psychological levels.
7. Conclusion
In conclusion, our findings suggested that frontline nurses could take targeted measures of positive coping style and social support, such as strengthening the guidance of nursing knowledge and nursing skills to improve their positive coping ability. Moreover, family members and other social support systems should be mobilized to give nurses’ psychological and emotional support. Through these methods, frontline nurses’ mental health could be improved.
Authorship of all the authors
Shaohua Hu designed this study and wrote the final draft of paper; Ting Wang and Qianqian Zhang performed the study and analyzed the data, Qing Dai wrote the first draft of paper. Chaoqun Li and Hongye He recruited volunteers and collected electronic questionnaires. All authors critically reviewed the manuscript and approved the final version submitted for publication.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work was funded by COVID-19 epidemic Prevention and Control Project of Medical Humanities Research Center of Anhui Medical University (N0. YJSK202013).
Note
Shaohua Hu and Qing Dai contributed equally to this work.
Acknowledgements
We would like to thank all volunteers who participated in this study for their effort and time and those who made huge sacrifices in fighting the epidemic.
References
- 1.Blumenthal J., Burg M., Barefoot J. Social support, type A behavior, and coronary artery disease. Psychosom Med. 1987;49:331–340. doi: 10.1097/00006842-198707000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Cohen S., Wills T. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- 3.Costa P., McCrae R. FL: Psychological Assessment Resources; Odessa, Florida: 1992. Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory. [Google Scholar]
- 4.Coyne J., Downey G. Social factors and psychopathology:stress, social support and coping process. Annu Rev Psycho. 2017;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- 5.Dunkley D., Ma D., Lee I. Advancing complex explanatory conceptualization of daily negative and positive affect: trigger and maintenance coping action patterns. J Couns Psychol. 2014;61:93–109. doi: 10.1037/a0034673. [DOI] [PubMed] [Google Scholar]
- 6.Gray-Toft P., Anderson J. Stress among hospital staff: its causes and midwives. Br J Nurs. 1994;3:527–534. [Google Scholar]
- 7.Yildirim H., Isik K., Firat T.Y., Aylaz R. Determining the Correlation between social support and hopelessness of Syrian refugees living in Turkey. J Psychiatr Nurs Ment Health Serv. 2020;58:127–733. doi: 10.3928/02793695-20200506-04. [DOI] [PubMed] [Google Scholar]
- 8.Hu J. Central South University; 2010. Investigation of psychological status of medical staff and analysis of related factors during the outbreak of “Influenza H1N1”. [Google Scholar]
- 9.Jiang Q. Comprehension social support scale. China Behav Med Sci. 2001;10:41–42. [Google Scholar]
- 10.Wu J., Rong X., Chen F., Diao Y., Chen D., Jing X., Gong X. Vol. 34. 2020. pp. 558–562. (Investigation on sleep quality of first-line nurses in fighting against corona virus disease 2019 andits influencing factors). [Google Scholar]
- 11.Kakemam E., Kalhor R., Khakdel Z. Occupational stress and cognitive failure of nurses and associations with self-reported adverse events: a national cross-sectional survey. J Adv Nurs. 2019;75:3609–3618. doi: 10.1111/jan.14201. [DOI] [PubMed] [Google Scholar]
- 12.Kessler R., Mroczek D. Ann Arbor (MI), Survey Research Center of the Institute for Social Research; University of Michigan: 1994. Final version of our non-specific psychological distress scale. [Reprinted], [Google Scholar]
- 13.Lai J., Ma S., Hu S. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.LeeAnne B., Sherwin E., Leary W., Henderson A. Effect of illness representations and catastrophizing on quality of life in adults with irritable bowel syndrome. J Psychiatr Nurs Ment Health Serv. 2016;54:44–53. doi: 10.3928/02793695-20160803-01. [DOI] [PubMed] [Google Scholar]
- 15.Li X., Liu Y. Job stressors and burnout among staff nurses. Chinese Journal of Nursing. 2000 [Google Scholar]
- 16.Liu G., Luo Y., Gao G. Research on the mental health status and coping style of nurses nursing SARS patients. J Nurs. 2004;21:9–11. [Google Scholar]
- 17.Mei J.H., Z.Q.G.X. Psychological and sleep status analysis of medical staff in the infection of new coronavirus pneumonia. Medical Herald. 2020;39:345–349. [Google Scholar]
- 18.Mitchell I., Evans L., Rees T. Stressors, social support, and tests of the buffering hypothesis: effects on psychological responses of injured athletes. Br J Health Psychol. 2014;19:486–508. doi: 10.1111/bjhp.12046. [DOI] [PubMed] [Google Scholar]
- 19.Nickell L., Crighton E., Tracy C. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004;170:793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pu J., Li G., Cao L., Wu Y., Xu L. Investigation and analysis of the psychological status of clinical nurses in a teritary A hospital facing the novel coronavirus pneumonia. Chongqing Medicine. 2020;49:1–7. [Google Scholar]
- 21.Tam D., Lee S., Lee S. Impact of SARS on avian influenza pre-paredness in healthcare workers. Clin Epidemiol Study. 2007;35:320–325. doi: 10.1007/s15010-007-6353-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ward K., Shaw S., Chang M. Social support moderates the association between traumatic life events and depression among migrant and nonmigrant men in almaty, Kazakhstan. J Trauma Stress. 2018;31:698–707. doi: 10.1002/jts.22324. [DOI] [PubMed] [Google Scholar]
- 23.Wheeler H., Riding R. Occupational stress in general nurses and mid-wives. Br J Nurs. 1994;3:527–534. doi: 10.12968/bjon.1994.3.10.527. [DOI] [PubMed] [Google Scholar]
- 24.Xi X., Shi Z., Yao Y. Preliminary exploration of psychological crisis intervention strategies at the scene of public emergencies. Chinese J Health Manag. 2019;13:133–138. [Google Scholar]
- 25.Xie Y. A preliminary study on the reliability and validity of the Simple Coping Style Scale. Chinese J Clin Psychol. 1998;2:53–54. [Google Scholar]
- 26.Xu M.C.Z.Y. Mental status survey of the first batch of clinical frontline support nurses to fight against new coronavirus infection pneumonia. 2020;34:368–370. [Google Scholar]
- 27.Yang H., Dai L., Chen Q. A qualitative study on the psychological experience of the first batch of nurses to fight against the new coronavirus pneumonia. J Nurs Manag. 2020:1–4. [Google Scholar]
- 28.Yang X., Zhang L., Hua Q. Investigation of psychological status of SARS clinical nurses. Zhonghua Hu Li Za Zhi. 2004;11:69–71. [Google Scholar]
- 29.Zeidner M., Endler N. Wiley& Sons Ltd; 1996. Hanbook of coping: Theory, Research, Applications. [Google Scholar]
- 30.Zhang A., Wang Z. Investigation on the coping style and social support of nurses in SARS wards. 2005;2:28–31. [Google Scholar]