Abstract
COVID-19 has become a nationwide public health crisis in the United States and the number of COVID-19 cases is different by U.S. counties. Also, previous studies have reported that neighborhood contexts have an influence on health outcomes. Therefore, the objective of this study was to examine the association between neighborhood contexts and cumulative number of confirmed COVID-19 cases (per 100,000) in U.S. counties. Cumulative number of COVID-19 cases gained from USA FACTS and variables related to neighborhood contexts gained from the 2018 5-Year American Community Survey at the county level. Data were analyzed using spatial autoregressive models. According to the present results, firstly, larger population, high poverty rate, higher % of bachelor's degree, higher % of no health insurance, higher employment rate, higher % of manufacturing jobs, higher % of primary industry jobs, higher % of commute by drove alone, higher % of foreign born, higher % of Hispanic, and higher % of Black are positively associated with higher cumulative number of COVID-19 cases. Secondly, higher income, higher % of cash assistance recipient, higher % of SNAP recipient, higher unemployment rate, higher % of commute by walked, higher % of Asian, and higher % of senior citizen are negatively associated with higher cumulative number of COVID-19 cases. In conclusion, there exist geographical differences in cumulative number of COVID-19 cases in U.S. counties, which is influenced by various neighborhood contexts. Hence, these findings emphasize the need to take various neighborhood contexts into account when planning COVID-19 prevention.
Keywords: COVID-19, Spatial analysis, Neighborhood contexts, U.S. counties
1. Introduction
Coronavirus disease 2019 (COVID-19) is a highly contagious respiratory disease, which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (CDC 2020a). The COVID-19 virus is more infectious than other corona viruses such as SARS and MERS even though it is less severe (CDC, 2020a). The COVID-19 virus is a person to person transmitted disease that spreads mainly through respiratory droplet and saliva of infected people (CDC, 2020b). The United States have one of the most cumulative confirmed cases of COVID-19 in the world. Cumulative confirmed COVID-19 case totals for the United States was 8,202,847 through October 20, 2020 (USA FACTS, 2020). Although COVID-19 virus has spread across the United States, the number of COVID-19 cases is different by counties (USA FACTS, 2020). Neighborhood contexts and regional characteristics might lead to geographical difference in the number of COVID-19 cases.
Previous studies have reported that poor neighborhood contexts particularly those characterized by disadvantaged socioeconomic status are associated with increased body mass index and mortality (Andersen et al., 2018; Frank et al., 2006; Wong et al., 2018). Also, residential segregation has a negative effect on health status among ethnic minorities (Greer et al., 2011; White and Borrell, 2011). This is guided by the social cognitive model of reciprocal determinism which suggests that environmental factors have an influence on individuals, groups, and their behaviors (Glanz et al., 2008). It means that geographical differences in health behavior caused by various environmental factors could cause dissimilar health outcomes in accordance with geographical areas. In this regard, some research studies have reported that the neighborhood context in which people live is associated with different health outcomes (Bleich et al., 2010; Gaskin et al., 2009; LaVeist et al., 2008; LaViest et al., 2009; Thorpe et al., 2013).
Moreover, previous research studies have reported that poor neighborhood contexts particularly those characterized by social vulnerability, minorities, and low socioeconomic status are associated with increased risk of COVID-19 (Khazanchi et al., 2020; van Holm et al., 2020; Yancy, 2020). However, these studies are based on the initial outbreak of COVID-19 that may underestimate cases of COVID-19 in some counties. In addition, these studies did not deal with occupational variables. Neighborhood contexts are classified by occupational composition (Clarke et al., 2013) that a certain type of occupational variable can lead to higher number of COVID-19 cases. Also, other related studies have focused mainly on the concepts and techniques of GIS (Mollalo et al., 2020; Sun et al., 2020). More research is needed, therefore, to reexamine the association between various neighborhood contexts including occupational variables and the number of COVID-19 cases from public health and social perspectives. Thus, the objective of this study was to examine the association between neighborhood contexts and cumulative number of confirmed COVID-19 cases (per 100,000) in 3136 U.S. counties through October 20, 2020.
2. Methods
2.1. Data
This study is designed to analyze cumulative number of confirmed COVID-19 cases as on time period with pre-existing cross-sectional neighborhood contexts in the United States.
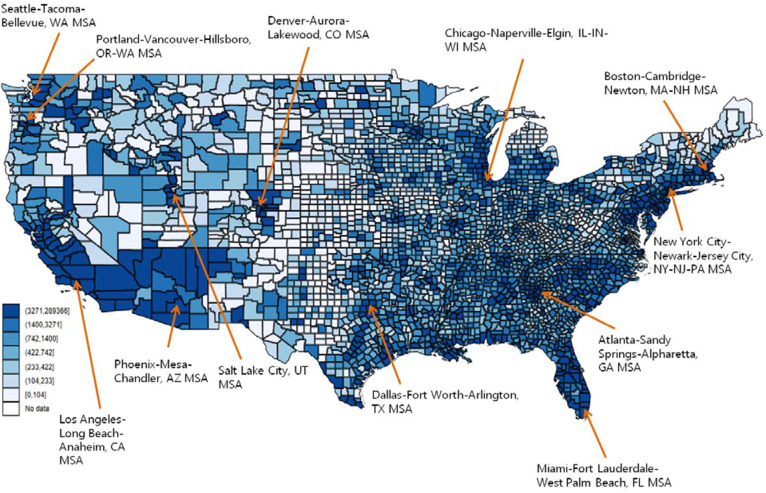
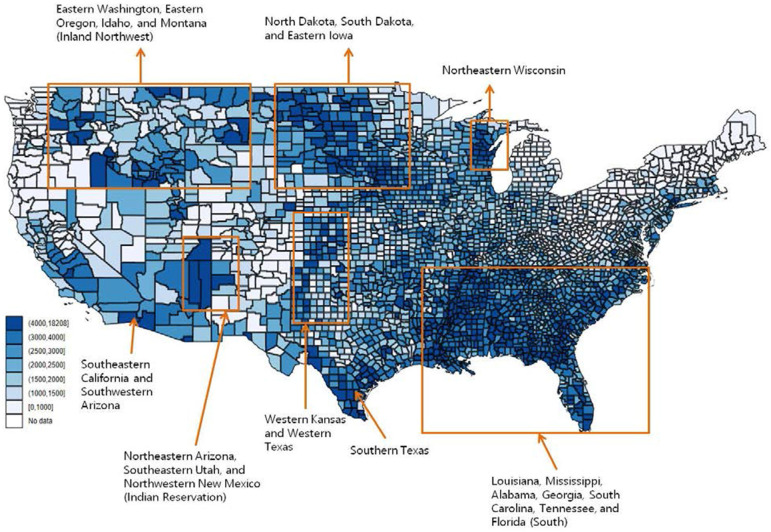
To analyze how neighborhood contexts influence the number of confirmed COVID-19 cases, firstly, the number of confirmed COVID-19 cases in the United States gained from USA FACTS (USA FACTS, 2020). A dependent variable is cumulative number of confirmed COVID-19 cases at the county level in the United States. USA FACTS publishes data each day, so, I used cumulative number of confirmed COVID-19 cases through October 20, 2020. A dependent variable transformed to per capita figure (per 100,000 residents) because the number of confirmed COVID-19 cases is greatly influenced by the number of residents in a county level. Cumulative cases are mapped as shown in Fig. 2 and cumulative cases per capita are mapped as shown in Fig. 3. The highest number of COVID-19 cases is concentrated in the urbanized counties in Fig. 2 whereas the highest number of COVID-19 cases per capita is concentrated in rural counties such as Southeastern California, Southwestern Arizona, Inland Northwest (Eastern Washington, Eastern Oregon, Montana), North Dakota, South Dakota, Eastern Iowa, Indian Reservation (Northeastern Arizona, Southeastern Utah, and Northwestern New Mexico), Western Kansas, Western Texas, Southern Texas, Northeastern Wisconsin, and South (Louisiana, Mississippi, Alabama, Georgia, South Carolina, Tennessee, and Florida) in Fig. 3.
Fig. 2.
Mainland United States map of cumulative number of confirmed cases of COVID-19 by county level through October 20, 2020.
Fig. 3.
Mainland United States map of cumulative number of confirmed cases of COVID-19 (per 100,000) by county level through October 20, 2020.
Secondly, variables related to neighborhood contexts gained from the 2018 5-Year American Community Survey at the county level (American Community Survey (ACS), 2020). These variables are categorized into seven aspects based on dataset such as population, socioeconomic status (median household income, % of poverty, % of bachelor's degree, % of no health insurance, % of cash assistance recipient, % of SNAP recipient, % of unemployment, % of employment), occupations (% of manufacturing, % of service, % of agriculture, forestry, fishing, hunting, and mining, and % of armed forces), Types of commute (public transportation, drove alone, and walked), minorities (% of foreign born, % of Asian, % of Hispanic, and % of Black), % of senior citizen (over 65), and % of male. This study did not require approval from the institutional review board because the datasets are secondary data that does not include personal information.
2.2. Data analysis
Ordinary least squares (OLS) regression model is vulnerable to bias caused by potential spatial autocorrelation because it presupposes that all variables are independent which ignores potential spatial dependencies (Anselin, 1988; Conway et al., 2010). According to the primary law of geography, even though every spatial unit is linked to everything else, spatial units near to each other are more strongly linked (Anselin, 1988). To control potential bias related to spatial autocorrelation, therefore, spatial autoregressive models were used to analyze the association between neighborhood contexts and cumulative number of COVID-19 cases.
Firstly, the spatial lag model demonstrates that result in one spatial unit is linked to result in another spatial unit (Liu, 2020). The main function of this model is to remedy for spatial dependence by adopting a term for the impact of the spatially lagged Y on Y (Anselin et al., 1996; Conway et al., 2010). It means that the result variable in location a is affected by neighboring location b (Anselin et al., 1996; Conway et al., 2010). It can be summarized as follows:
Y: dependent variable.ρ: lag coefficient.W: spatial weight matrix.β: coefficient for a vector of neighborhood contexts.ε: error term.
Secondly, the spatial error model demonstrates that unobserved factors in one spatial unit are linked to unobserved factor in another spatial unit (Liu, 2020). It means that the error term in location a is affected by neighboring location b (Anselin et al., 1996; Conway et al., 2010). It can be summarized as follows:
Y: dependent variable.β: coefficient for a vector of neighborhood contexts.λ: coefficient.W: spatial weight matrix.ε: residual error matrix.v: the normal assumption for the error term.
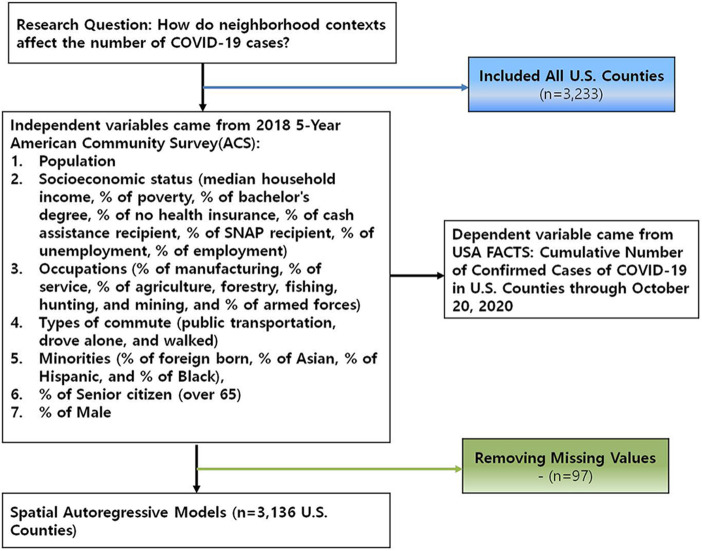
All statistical analyses were conducted using STATA (version 15.0, StataCorp LLC., College Station, TX). Study methods are summarized in sample flow chart (Fig. 1 ).
Fig. 1.
Sample flow chart.
3. Results
Table 1 shows the descriptive statistics. First, the average poverty rate in 3,136 U.S. counties is 11.24%. Second, the average percentage of bachelor’s degree in 3,136 U.S. counties is 14.01%. Third, the average percentage of no health insurance in 3,136 U.S. counties is 6.27%. Fourth, the average percentage of cash assistance recipient in 3,136 U.S. counties is 2.32%. Fifth, the average percentage of SNAP recipient in 3,136 U.S. counties is 13.24%. Sixth, the average unemployment rate in 3,136 U.S. counties is 3.26%. Seventh, the average employment rate in 3,136 U.S. counties is 54.92%. Eighth, the average percentage of manufacturing occupations in 3,136 U.S. counties is 12.30%. Ninth, the average percentage of service occupations in 3,136 U.S. counties is 18.03%. Tenth, the average percentage of agriculture, forestry, fishing, hunting, and mining occupations in 3,136 U.S. counties is 6.66%. Eleventh, the average percentage of armed forces in 3,136 U.S. counties is 0.29%. Twelfth, the average percentage of commute by public transportation in 3,136 U.S. counties is 0.92%. Thirteenth, the average percentage of commute by drove alone in 3,136 U.S. counties is 79.67%. Fourteenth, the average percentage of commute by walked in 3,136 U.S. counties is 1.19%. Fifteenth, the average percentage of foreign born in 3,136 U.S. counties is 4.72%. Sixteenth, the average percentage of Asian in 3,136 U.S. counties is 1.36%. Seventeenth, the average percentage of Hispanic in 3,136 U.S. counties is 9.24%. Eighteenth, the average percentage of Black in 3136 U.S. counties is 9.08%. Nineteenth, the average percentage of senior citizen (over 65) in 3136 U.S. counties is 18.37%. Twentieth, the average percentage of male in 3136 U.S. counties is 50.08%.
Table 1.
Descriptive statistics (n = 3136).
| Variables | Mean | SD | Min | Max |
|---|---|---|---|---|
| Confirmed cases of COVID-19 per 100,000(logged) | 7.569 | ±0.737 | 3.882 | 9.810 |
| Population(logged) | 10.278 | ±1.479 | 5.429 | 16.128 |
| Median household income(logged) | 9.322 | ±1.462 | 4.511 | 15.011 |
| % of poverty | 11.242 | ±5.654 | 0 | 52.1 |
| % of Bachelor's degree | 14.007 | ±5.628 | 2.2 | 48 |
| % of no health insurance | 6.268 | ±4.962 | 0 | 52.5 |
| % of cash assistance recipient | 2.323 | ±1.695 | 0 | 29 |
| % of SNAP recipient | 13.235 | ±6.519 | 0 | 59.9 |
| % of unemployment | 3.260 | ±1.457 | 0 | 16.5 |
| % of employment | 54.915 | ±8.348 | 12.8 | 79.8 |
| % of manufacturing occupations | 12.302 | ±7.171 | 0 | 51.7 |
| % of service occupations | 18.031 | ±3.629 | 5.9 | 43.6 |
| % of agriculture, forestry, fishing, hunting, and mining occupations | 6.661 | ±7.293 | 0 | 60.5 |
| % of armed forces | 0.285 | ±1.563 | 0 | 52 |
| % of commute by public transportation | 0.917 | ±3.077 | 0 | 61.4 |
| % of commute by drove alone | 79.671 | ±7.591 | 4.9 | 96.3 |
| % of commute by walked | 1.186 | ±1.539 | 0.1 | 43.6 |
| % of foreign born | 4.720 | ±5.706 | 0 | 53.3 |
| % of Asian | 1.364 | ±2.774 | 0 | 42.5 |
| % of Hispanic | 9.242 | ±13.756 | 0 | 99.1 |
| % of black | 9.075 | ±14.540 | 0 | 87.4 |
| % of over 65 | 18.370 | ±4.546 | 3.8 | 55.6 |
| % of male | 50.083 | ±2.368 | 42.1 | 79 |
Table 2 shows the results of OLS regression model and spatial autoregressive models of neighborhood contexts and cumulative number of COVID-19 cases. According to Akaike info criterion (OLS: 5797.872, Spatial Lag: 5559.466, Spatial Error: 4006.928), lower test statistic is the more appropriate model, which suggest utilizing the spatial lag model and spatial error model. The results of OLS regression model relatively similar to spatial lag model or spatial error model, but it produced reverse result at senior citizen (OLS: 0.040⁎, Spatial Lag: −0.010⁎, Spatial Error: −0.023⁎⁎).
Table 2.
| Variables | OLS (n = 3136) |
Spatial lag (n = 3136) |
Spatial error (n = 3136) |
|---|---|---|---|
| Coef. [standard error] | Coef. [standard error] | Coef. [standard error] | |
| Population(logged) | 0.774⁎⁎⁎ [0.181] | 0.741⁎⁎⁎ [0.180] | 0.435⁎⁎ [0.139] |
| Median household income(logged) | −0.762⁎⁎⁎ [0.181] | −0.759⁎⁎⁎ [0.179] | −0.363⁎⁎ [0.137] |
| % of poverty | 0.041⁎⁎⁎ [0.004] | 0.038⁎⁎⁎ [0.004] | 0.014⁎⁎⁎ [0.003] |
| % of Bachelor's degree | 0.007 [0.004] | 0.008⁎ [0.004] | 0.009⁎⁎ [0.003] |
| % of no health insurance | 0.018⁎⁎⁎ [0.003] | 0.017⁎⁎⁎ [0.003] | 0.006⁎ [0.003] |
| % of cash assistance recipient | −0.021⁎⁎ [0.008] | −0.014 [0.008] | −0.014⁎ [0.006] |
| % of SNAP recipient | −0.013⁎⁎ [0.004] | −0.011⁎⁎ [0.004] | −0.004 [0.003] |
| % of unemployment | −0.047⁎⁎⁎ [0.011] | −0.040⁎⁎⁎ [0.010] | −0.014 [0.008] |
| % of employment | 0.015⁎⁎⁎ [0.003] | 0.014⁎⁎⁎ [0.003] | −0.005 [0.003] |
| % of manufacturing occupations | 0.015⁎⁎⁎ [0.002] | 0.012⁎⁎⁎ [0.002] | 0.010⁎⁎⁎ [0.002] |
| % of service occupations | 0.002 [0.004] | 0.004 [0.004] | 0.005 [0.003] |
| % of agriculture, forestry, fishing, hunting, and mining occupations | 0.015⁎⁎⁎ [0.003] | 0.008⁎⁎ [0.003] | 0.001 [0.002] |
| % of armed forces | 0.003 [0.008] | 0.013 [0.007] | −0.010 [0.005] |
| % of commute by public transportation | 0.014⁎⁎ [0.005] | 0.009 [0.005] | 0.000 [0.005] |
| % of commute by drove alone | 0.011⁎⁎⁎ [0.002] | 0.009⁎⁎⁎ [0.002] | 0.002 [0.002] |
| % of commute by walked | −0.050⁎⁎⁎ [0.010] | −0.043⁎⁎⁎ [0.010] | −0.023⁎⁎ [0.007] |
| % of foreign born | 0.017⁎⁎⁎ [0.004] | 0.023⁎⁎⁎ [0.004] | 0.013⁎⁎ [0.004] |
| % of Asian | −0.046⁎⁎⁎ [0.006] | −0.039⁎⁎⁎ [0.006] | −0.045⁎⁎⁎ [0.005] |
| % of Hispanic | −0.002 [0.001] | −0.002 [0.001] | 0.009⁎⁎⁎ [0.002] |
| % of black | 0.014⁎⁎⁎ [0.001] | 0.013⁎⁎⁎ [0.001] | 0.009⁎⁎⁎ [0.001] |
| % of over 65 | 0.040⁎ [0.014] | −0.010⁎ [0.005] | −0.023⁎⁎⁎ [0.004] |
| % of male | 0.005 [0.006] | 0.004 [0.006] | 0.000 [0.005] |
| Constant | 3.728⁎⁎⁎ [0.504] | 4.037⁎⁎⁎ [0.652] | 6.356⁎⁎⁎ [0.510] |
| ρWY | 0.109⁎⁎⁎ [0.007] | ||
| λWε | 0.892⁎⁎⁎ [0.013] | ||
| -2LOGL | 5509.466 | 3956.928 | |
| Akaike info criterion | 5797.872 | 5559.466 | 4006.928 |
P < 0.05.
P < 0.01.
P < 0.001.
Unstandardized coefficient from spatial autoregressive models indicated that first, counties with larger population are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.741, p < 0.001, Spatial Error: B = 0.435, p < 0.01). Second, counties with higher median household income are negatively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = −0.759, p < 0.001, Spatial Error: B = −0.363, p < 0.01). Third, counties with higher poverty rate are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.038, p < 0.001, Spatial Error: B = 0.014, p < 0.001). Fourth, counties with higher percentage of bachelor's degree are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.008, p < 0.05, Spatial Error: B = 0.009, p < 0.01). Fifth, counties with higher percentage of no health insurance are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.017, p < 0.001, Spatial Error: B = 0.006, p < 0.05). Sixth, counties with higher percentage of cash assistance are negatively associated with higher number of COVID-19 cases in one model (Spatial Error: B = −0.014, p < 0.05). Seventh, counties with higher percentage of SNAP recipients are negatively associated with higher number of COVID-19 cases in one model (Spatial Lag: B = −0.011, p < 0.01). Eighth, counties with higher unemployment rate are negatively associated with higher number of COVID-19 cases in one model (Spatial Lag: B = −0.040, p < 0.001). Ninth, counties with higher employment rate are positively associated with higher number of COVID-19 cases in one model (Spatial Lag: B = 0.014, p < 0.001). Tenth, counties with higher percentage of manufacturing occupations are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.012, p < 0.001, Spatial Error: B = 0.010, p < 0.001). Eleventh, counties with higher percentage of agriculture, forestry, fishing, hunting, and mining occupations are positively associated with higher number of COVID-19 cases in one model (Spatial Lag: B = 0.008, p < 0.01). Twelfth, counties with higher percentage of commute by drove alone are positively associated with higher number of COVID-19 cases in one model (Spatial Lag: B = 0.009, p < 0.001). Thirteenth, counties with higher percentage of commute by walked are negatively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = −0.043, p < 0.001, Spatial Error: B = −0.023, p < 0.01). Fourteenth, counties with higher percentage of foreign born are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.023, p < 0.001, Spatial Error: B = 0.013, p < 0.01). Fifteenth, counties with higher percentage of Asian are negatively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = −0.039, p < 0.001, Spatial Error: B = −0.045, p < 0.001). Sixteenth, counties with higher percentage of Hispanic are positively associated with higher number of COVID-19 cases in one model (Spatial Error: B = 0.009, p < 0.001). Seventeenth, counties with higher percentage of Black are positively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = 0.013, p < 0.001, Spatial Error: B = 0.009, p < 0.001). Eighteenth, counties with higher percentage of senior citizen (over 65) are negatively associated with higher number of COVID-19 cases in both models (Spatial Lag: B = −0.010, p < 0.05, Spatial Error: B = −0.023, p < 0.001).
4. Discussion
This study observed firstly that there is a positive association between larger population and higher cumulative number of COVID-19 cases. Even though this study used per capita figure (per 100,000 residents) to minimize the impact of the number of residents in a county level on dependent variable, population size still maintains significance.
This study observed secondly that low socioeconomic status variables particularly those characterized by lower median household income, higher poverty rate, and higher percent of no health insurance are positively associated with higher cumulative number of COVID-19 cases. This finding is similar to those reported in previous studies (Khazanchi et al., 2020; van Holm et al., 2020; Yancy, 2020). However, other related variables such as higher percentage of cash assistance recipient, higher percentage of SNAP recipient, and higher unemployment rate are negatively associated with higher cumulative number of COVID-19 cases. Cash assistance benefit and SNAP benefit are closely associated with high unemployment rate (O'Leary, 2020). On the other hand, counties with higher employment rate and higher percentage of bachelor's degree are positively associated with higher cumulative number of COVID-19 cases. There is a positive association between bachelor's degree and higher employment rate because people with bachelor's degree are more likely to be employed than those who without bachelor's degree (NCES, 2020). The COVID-19 outbreak is related to social activities such as work life because the COVID-19 virus is a person to person transmitted disease that spreads mainly through respiratory droplet and saliva of infected people (CDC, 2020b). For this reason, counties with higher employment rate seem to be more vulnerable to the COVID-19 outbreak. Therefore, public health authorities need to increase their efforts to prevent workplace exposures to COVID-19.
This study observed thirdly that counties with higher percentage of manufacturing occupations or primary industry are positively associated with higher cumulative number of COVID-19 cases. The manufacturing work environment particularly those characterized by bustling plant and numerous workers where workers have close touch with colleagues and supervisors may result in mass COVID-19 cases (CDC, 2020c). In terms of primary industry, it would be related to per capita cases (per 100,000). As shown in Fig. 3, the highest number of COVID-19 cases per capita is concentrated in rural counties such as Southeastern California, Southwestern Arizona, Inland Northwest (Eastern Washington, Eastern Oregon, Montana), North Dakota, South Dakota, Eastern Iowa, Indian Reservation (Northeastern Arizona, Southeastern Utah, and Northwestern New Mexico), Western Kansas, Western Texas, Southern Texas, Northeastern Wisconsin, and South (Louisiana, Mississippi, Alabama, Georgia, South Carolina, Tennessee, and Florida) which means that rural counties are also vulnerable to COVID-19.
This study observed fourthly that commute by drove alone is positively associated with higher cumulative number of COVID-19 cases. On the other hand, there is a negative association between commute by walked and higher cumulative number of COVID-19 cases. A previous study has reported that longer commute leads to spread of COVID-19 virus because long-distance commuters (commute by drove alone) are more likely to spread COVID-19 virus from one county to another county than short-distance commuters (commute by walked) (van Holm et al., 2020).
This study observed fifthly that counties with higher percentage of immigrants or ethnic minorities (Hispanic and Black) are positively associated with higher cumulative number of COVID-19 cases. Residential segregation has a negative effect on health outcomes for ethnic minorities in the United States (Greer et al., 2011; White and Borrell, 2011). In addition, high poverty rate and high working poor rate among ethnic minorities might lead to higher number of COVID-19 cases. This is because compared to Non-Hispanic white, ethnic minorities have higher poverty rate (White: 9.0%, Hispanic: 17.2%, Black: 21.2%, Asian: 9.7%) Kaiser Family Foundation (KFF), 2020. and higher working poor rate (White: 3.9%, Hispanic: 7.9%, Black: 7.8%, Asian: 3.2%) (BLS, 2018). Asian has lower poverty rate and lower working poor rate than other ethnic minorities that might lead to lower cumulative number of COVID-19 cases among Asian people.
This study observed sixthly that there is a negative association between senior citizen (over 65) and higher cumulative number of COVID-19 cases. This phenomenon seems to be closely related to social activities including work life. Generally, senior citizens are less likely to engage in social activities than young adults and middle aged that might lead to lower cumulative number of COVID-19 cases among senior citizens.
The observations of this study should be considered in light of several limitations. Firstly, log transformed dependent variable may conceal the real variations of COVID-19 cases among counties. Secondly, this study used pre-existing cross-sectional neighborhood contexts in 2018 that may not correspond with COVID-19 cases through October 20, 2020. Thirdly, the temporal causal relationship between neighborhood contexts and cumulative number of COVID-19 cases cannot be determined because the study design was cross-sectional. Finally, this study did not consider the number of days since the first case in a county. For this reason, it was impossible to demonstrate how the number of confirmed cases may vary over time.
5. Conclusion
Despite the above limitations, this study provides meaningful information from a spatial analysis of the effect of neighborhood contexts on cumulative number of COVID-19 cases in U.S. counties. In summary, there exist geographical differences in cumulative number of COVID-19 cases in U.S. counties, which is influenced by various neighborhood contexts. Larger population, high poverty rate, higher % of bachelor's degree, higher % of no health insurance, higher employment rate, higher % of manufacturing jobs, higher % of primary industry jobs, higher % of commute by drove alone, higher % of foreign born, higher % of Hispanic, and higher % of Black are positively associated with higher cumulative number of COVID-19 cases. On the other hand, higher income, higher % of cash assistance recipient, higher % of SNAP recipient, higher unemployment rate, higher % of commute by walked, higher % of Asian, and higher % of senior citizen are negatively associated with higher cumulative number of COVID-19 cases. In the United States, the total economic burden of COVID-19 is about $16 trillion (NBER, 2020). In consideration of economic and health implications of COVID-19, effective COVID-19 prevention measures are needed. Hence, these findings emphasize the need to take various neighborhood contexts into account when planning COVID-19 prevention.
Declaration of Competing Interest
None.
References
- USA FACTS . 2020. US coronavirus cases and deaths. Track COVID-19 data daily by state and county.https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ (Accessed date: 28 October 2020) [Google Scholar]
- American Community Survey (ACS) 2014—2018 ACS 5-Year Data Profile. 2020. https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/ (Accessed date: 25 October 2020)
- Centers for Disease Control and Prevention (CDC). 2020b. Coronavirus Disease 2019 (COVID- 19). How COVID-19 Spreads. (Accessed date: 29 October 2020) https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Ftransmission.html.
- Centers for Disease Control and Prevention (CDC) 2020. Coronavirus Disease 2019 (COVID-19). Manufacturing Workers and Employers. Interim Guidance from CDC and the Occupational Safety and Health Administration (OSHA)https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-manufacturing-workers-employers.html (Accessed date: 02 November 2020) [Google Scholar]
- KFF . 2020. State health facts. poverty rate by race/ethnicity.https://www.kff.org/other/state-indicator/poverty-rate-by-raceethnicity/?currentTimeframe=0&selectedRows=%7B%22states%22:%7B%22all%22:%7B%7D%7D,%22wrapups%22:%7B%22united-states%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (Accessed date: 03 November 2020) [Google Scholar]
- National Center for Education Statistics (NCES) FAST FACTS. Employment Rates of College Graduates. 2020. https://nces.ed.gov/fastfacts/display.asp?id=561 (Accessed date: 31 December 2020)
- U.S. Bureau of Labor Statistics (BLS) BLS REPORTS. A Profile of the Working Poor, 2018. 2020. https://www.bls.gov/opub/reports/working-poor/2018/home.htm (Accessed date: 03 November 2020)
- Andersen S.W., Blot W.J., Shu X.O., et al. Associations between neighborhood environment, health behaviors, and mortality. Am. J. Prev. Med. 2018;54(1):87–95. doi: 10.1016/j.amepre.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin L. Lagrange multiplier test diagnostics for spatial dependence and spatial heterogeneity. Geogr Analysis. 1988;20(1):1–17. [Google Scholar]
- Anselin L., Bera A.K., Florax R., et al. Simple diagnostic tests for spatial dependence. Regional Sci Urban Econ. 1996;26(1):77–104. [Google Scholar]
- Bleich S.N., Thorpe R.J., Sharif-Harris H., et al. Social context explains race disparities in obesity among women. J. Epidemiol. Community Health. 2010;64(5):465–469. doi: 10.1136/jech.2009.096297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2020. National Notifiable Diseases Surveillance System. Coronavirus Disease 2019 (COVID-19) 2020 Interim Case Definition. Approved August 5, 2020. [Google Scholar]
- Clarke P., Morenoff J., Debbink M., et al. Cumulative exposure to neighborhood context: consequences for health transitions over the adult life course. Res Aging. 2013;36(1):115–142. doi: 10.1177/0164027512470702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway D., Li C.Q., Wolch J., et al. A spatial autocorrelation approach for examining the effects of urban Greenspace on residential property values. J. Real Estate Financ. Econ. 2010;41(2):150–169. [Google Scholar]
- Frank L.D., Sallis J.F., Conway T.L., et al. Many pathways from land use to health: associations between neighborhood walkability and active transportation, body mass index, and air quality. J. Am. Plan. Assoc. 2006;72(1):75–87. [Google Scholar]
- Gaskin D.J., Price A., Brandon D.T., et al. Segregation and disparities in health services use. Med. Care Res. Rev. 2009;66(5):578–589. doi: 10.1177/1077558709336445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K., Rimer B.K., Viswanath K. 4th ed. Jossey-Bass; San Francisco (CA): 2008. Health Beahvior and Health Education: Theory, Research and Practice; pp. 170–171. [Google Scholar]
- Greer S., Casper M., Kramer M., et al. Racial residential segregation and stroke mortality in Atlanta. Ethn Dis. 2011;21(4):437–443. [PubMed] [Google Scholar]
- van Holm E.J., Wyczalkowski C.K., Dantzler P.A. Neighborhood conditions and the initial outbreak of COVID-19: the case of Louisiana. Journal of Public Health. 2020:fdaa147. doi: 10.1093/pubmed/fdaa147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazanchi R., Beiter E.R., Gondi S., et al. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. J. Gen. Intern. Med. 2020;35(9):2784–2787. doi: 10.1007/s11606-020-05882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T.A., Thorpe R.J., Bowen-Reid T., et al. Exploring health disparities in integrated communities: overview of the EHDIC study. J. Urban Health. 2008;85(1):11–21. doi: 10.1007/s11524-007-9226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaViest T.A., Thorpe R.J., Galarraga J.E., et al. Environmental and socioeconomic factors as contributors to racial disparities in diabetes prevalence. J. Gen. Intern. Med. 2009;24(10):1144–1148. doi: 10.1007/s11606-009-1085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D. Spatial Autoregression in Stata. Cross-sectional Spatial Autoregression : spregress. 2020. https://www.stata.com/training/webinar_series/spatial-autoregressive-models/spatial/resource/spregress.html (Accessed date: 31 October 2020)
- Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental united states. Sci. Total Environ. 2020;728:138884. doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Leary C.J. 2020. 75th W.E. UPJOHN INSTITUTE FOR EMPLOYMENT RESEARCH. Food Stamps and Unemployment Compensation in the COVID-19 Crisis.https://www.upjohn.org/research-highlights/food-stamps-and-unemployment-compensation-covid-19-crisis (Accessed date: 02 November 2020) [Google Scholar]
- Sun F., Matthews S.A., Yang T.C., Hu M.H. A spatial analysis of the COVID-19 period prevalence in U.S. counties through June 28, 2020: where geography matters? Ann. Epidemiol. 2020;52:54–59. doi: 10.1016/j.annepidem.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe R.J., Wilson-Frederick S.M., Bowie J.V., et al. Health behaviors and allcause mortality in African American men. Am J Mens Health. 2013;7(4Suppl) doi: 10.1177/1557988313487552. (8S-18S) [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Borrell L.N. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438–448. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M.S., Chan K.S., Jones-Smith J.C., et al. The neighborhood environment and obesity: understanding variation by race/ethnicity. Prev. Med. 2018;111:371–377. doi: 10.1016/j.ypmed.2017.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]