Abstract
Background
Gastric cancer remains a major cancer globally. More than half of patients with gastric cancer undergo surgery in Taiwan; however, few large nationwide studies have investigated the effects of traditional Chinese medicine (TCM) on gastric cancer management after surgery. This study aimed to evaluate the effect of TCM on patients with gastric cancer following surgery and adjuvant chemotherapy in Taiwan and its prescription trends.
Methods and Materials
The cohort sampling data set was obtained from the Registry of Catastrophic Illness Patient Database, a research database of patients with severe illnesses from the National Health Insurance Research Database, Taiwan. Patients who had received a new diagnosis of gastric cancer and had undergone surgery were enrolled. We matched TCM users and nonusers at a ratio of 1 : 3 based on the propensity score, and TCM users were also grouped into short-term and long-term users.
Results
The number of TCM users and nonusers was 1701 and 5103 after applying the propensity score at a ratio of 1 : 3. Short-term users and long-term TCM users were independently associated with a decreased risk of death with HRs of 0.59 (95% confidence interval (CI), 0.55–0.65) and 0.41 (95% CI, 0.36–0.47), respectively, compared with TCM nonusers. We also obtained similar results when we adjusted for covariates in the main model, as well as each of the additional listed covariates. We also observed similar HR trends in short-term users and long-term TCM users among men and women aged <65 years and ≥65 years. The most commonly prescribed single herb and herbal formula in our cohort were Hwang-Chyi (Radix Hedysari; 11.8%) and Xiang-Sha-Liu-Jun-Zi-Tang (15.5%), respectively.
Conclusion
TCM use was associated with higher survival in patients with gastric cancer after surgery and adjuvant chemotherapy. TCM could be used as a complementary and alternative therapy in patients with gastric cancer after surgery and adjuvant chemotherapy.
1. Introduction
Gastric cancer, including adenocarcinomas and other carcinomas, remains a major cancer globally and is ranked fifth among the most frequently diagnosed cancers, with over 1, 000, 000 new cases reported in 2018, and it is the third leading cause of cancer-related death, with approximately 7, 83, 000 deaths. [1] The incidence rate of gastric cancer is markedly high in Eastern Asia with 32.1 per 1, 00, 000 among men and 13.2 among women, and the incidence rate in South Korea is approximately 60 per 1, 00, 000 new cases annually among men and 25 per 1, 00, 000 among women. [2] Surgical resection is often adopted in the early stages of gastric cancer, whereas adjuvant therapies, such as radiotherapy or chemotherapy, are often considered in the advanced stages of gastric cancer. [3, 4] In 2010–2014, the five-year survival rate of gastric cancer was 69% in South Korea, 60% in Japan, and less than 40% in most other countries, including Taiwan and the United States. [5].
Traditional Chinese medicine (TCM), traumatology manipulative therapies, and acupuncture, which are included in traditional Chinese medical in Taiwan, are widely accepted as some of the most popular complementary and alternative (CAM) therapies for patients with cancer. In addition, Chinese herbal products (CHPs) represent decoctions that have been adopted more recently based on their consistent quality and are applied in clinical settings. In addition, because of their quality, convenience, and approval for full reimbursement for both single herbs and herbal formulas CHPs by the National Health Insurance (NHI) in Taiwan, Chinese medical physicians prescribe them to their patients. A computerized reimbursement database of the NHI, the National Health Insurance Research Database (NHIRD), contains comprehensive data on both TCM and Western medicine. Consequently, the NHIRD offers an appropriate resource for conducting pharmacoepidemiological research on medicine use.
A previous study reported that TCM improved overall survival among patients with gastric cancer in Taiwan. [6] In Taiwan, most patients with gastric cancer undergo surgery, and more than half of the patients who undergo surgery receive chemotherapy afterward. There are many clinical studies on the treatment of gastric cancer by TCM after surgery and chemoradiotherapy in China. However, large nationwide studies on the potential effects of the use of TCM on patients with gastric cancer after surgery and adjuvant chemotherapy remain limited. Therefore, the aim of the present study was to evaluate the effect of the use of TCM on patients with gastric cancer following surgery and adjuvant chemotherapy in Taiwan and the associated TCM prescription trends.
2. Methods
2.1. Data Source
The cohort sampling data set of the present study was obtained from the Registry of Catastrophic Illness Patient Database (RCIPD), a research database of patients with severe illnesses within the NHIRD system, NHI, Taiwan.
Because the Taiwanese NHI is obligatory for all residents, the NHIRD, which covers almost the entire population of 23.7 million people, is a rather detailed database in a health-related field.
Using data from the RCIPD, we can gather information based on both admissions and outpatient visits, which contains patient data such as admission and discharge dates, sex, age, diagnoses (made according to the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes), and outpatient visits. In addition, data include prescription for patients, such as the prescribed medicine, initiation date, duration, dosage, and total expenditure.
Because the information in the database is anonymous, in line with personal electronic data protection regulations set by the National Health Research Institutes of Taiwan, NHIRD data can only be used for research purposes. The use of the database, in which information is anonymized and informed consent requirement is waived, was approved by the Ethics Review Board of Chang Gung Memorial Hospital, Chiayi Branch, Taiwan.
2.2. Study Subjects
The study cohort was selected from admission and outpatient department records using diagnostic variables in the RCIPD. The ICD-9-CM codes 151 and codes beginning with 151 were used for the identification of gastric cancer. We included patients who had received a diagnosis of gastric cancer between January 1, 1999, and December 31, 2008, and survival was tracked until December 31, 2013. The endpoint of observation was death or end of follow-up. We excluded patients who had previously received a diagnosis of other cancer. In addition, we excluded patients who had not undergone surgery, patients who had undergone chemotherapy before surgery, and patients who did not undergo chemotherapy after surgery. In the consequence, patients with gastric cancer after surgery and adjuvant chemotherapy were included, whether they have done radiotherapy or not. Patients with missing information related to age, sex, level of urbanization, or level of income were also excluded.
2.3. Traditional Chinese Medicine Exposure
We downloaded data on reimbursements for Chinese medicine from the NHI website. We obtained the corresponding drug data from the Committee on Chinese Medicine and Pharmacy website, including the proportions of each constituent, date and period of drug approval, drug names, and manufacturers' codes.
To classify patients into TCM users and nonusers, patients who used TCM for 30 days or more were considered TCM users and those who used TCM for less than 30 days were considered TCM nonusers. In addition, to enable the evaluation of a dose-response relationship, we further grouped TCM users into short-term TCM users (patients who used TCM for 30–179 days) and long-term TCM users (patients who used TCM for more than 180 days).
2.4. Potential Confounders
We identified some comorbidities as potential confounding risk factors for gastric cancer, including the following diagnoses recorded during the study period: diabetes mellitus (ICD-9-CM codes 249-250), hypertension (ICD-9-CM codes 401-405), alcoholism (ICD-9-CM code 303), smoking-related disorder (ICD-9-CM code 305.1), chronic renal failure (ICD-9-CM code 585), and liver cirrhosis (ICD-9-CM codes 571.2, 571.5, and 571.6). We also considered age, sex, monthly insurance income, and urbanization level in the model. Chemotherapy treatments were classified into epirubicin- and mitomycin-based treatments, taxanes, and other regimens.
2.5. Matched Cohort
By using propensity scores, TCM users and nonusers were perfectly matched at a ratio of 1 : 3, and it is a great estimate of how likely a patient would use TCM as a treatment. Background information, such as urbanization level, monthly insurance income, age, sex, and all comorbidities, was obtained.
2.6. Statistical Analysis
We compared the distribution of baseline characteristics, namely sex, age at surgery, urbanization level, income level, comorbidities, and chemotherapy regimen, between TCM users and nonusers.
We used the Kaplan–Meier method to estimate the cumulative probability of the overall survival of TCM users and nonusers. We performed the log-rank test to examine differences in overall survival between the cohorts. We used the Cox proportional hazards model to compute hazard ratios (HRs) at a 95% confidence interval (CI) after adjustment for age, sex, monthly insurance income, urbanization level, and chemotherapy regimen. A two-tailed P value of 0.05 was considered significant. All analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC, USA).
3. Results
Of 33, 256 patients who had received a new diagnosis of gastric cancer between 1999 and 2008, 1331 were excluded because they had received a prior diagnosis of another cancer, 21 103 were excluded because they did not undergo surgery, chemotherapy, or surgery after chemotherapy, 2 were excluded because they were aged less than 18 years, and 203 were excluded because their data were incomplete. A total of 1721 and 8896 patients were classified as TCM users and nonusers, respectively. After applying the propensity score at a ratio of 1 : 3, the number of TCM users and nonusers was 1701 and 5103, respectively (Figure 1).
Figure 1.
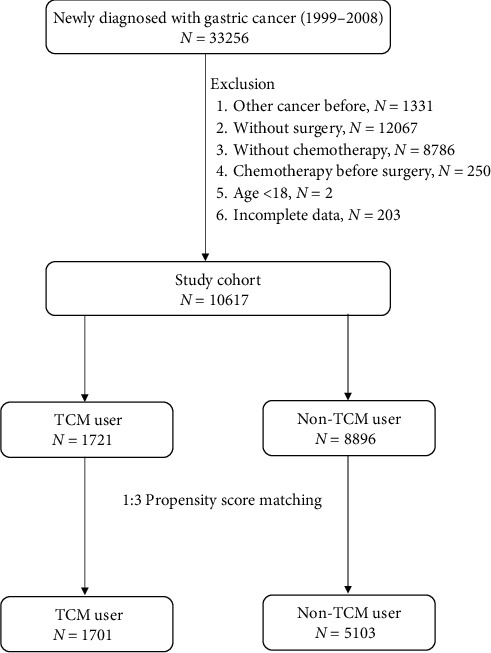
Flow chart of the patient enrollment process for the study cohort and the matched cohort.
In our study cohort, the mean age at surgery of TCM users and nonusers was 59.8 and 59.7 years, respectively. No significant differences were noted between the percentage of TCM users and nonusers based on sex, age at surgery, urbanization level, income level, and comorbidities (Table 1).
Table 1.
Baseline patient characteristics of TCM users and nonusers.
| Variables | TCM user (N = 1701) | Non-TCM user (N = 5103) | P value1 | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | 0.2554 | ||||
| Female | 722 | 42.5 | 2086 | 40.9 | |
| Male | 979 | 57.6 | 3017 | 59.1 | |
| Age at surgery, years | 0.5590 | ||||
| 18–64 | 1020 | 60.0 | 3019 | 59.2 | |
| ≥65 | 681 | 40.0 | 2084 | 40.8 | |
| Mean (SD) | 59.8 (12.2) | 59.7 (13.5) | 0.6760 | ||
| Urbanization | 0.9494 | ||||
| Very high | 499 | 29.3 | 1467 | 28.8 | |
| High | 790 | 46.4 | 2411 | 47.3 | |
| Moderate | 286 | 16.8 | 852 | 16.7 | |
| Low | 126 | 7.4 | 373 | 7.3 | |
| Income level (NTD2/per month) | 0.9925 | ||||
| 0 | 265 | 15.6 | 782 | 15.3 | |
| 1–15840 | 268 | 15.8 | 812 | 15.9 | |
| 15841–25000 | 779 | 45.8 | 2348 | 46.0 | |
| ≥25001 | 389 | 22.9 | 1161 | 22.8 | |
| Comorbidities | |||||
| Diabetes mellitus | 275 | 16.2 | 817 | 16.0 | 0.8788 |
| Hypertension | 554 | 32.6 | 1669 | 32.7 | 0.9168 |
| Alcoholism | 24 | 1.4 | 64 | 1.3 | 0.6202 |
| Smoking-related disorder | 154 | 9.1 | 454 | 8.9 | 0.8444 |
| Chronic renal failure | 33 | 1.9 | 100 | 2.0 | 0.9597 |
| Liver cirrhosis | 37 | 2.2 | 99 | 1.9 | 0.5484 |
| Chemotherapy regimen | 0.8593 | ||||
| Group 1 (epirubicin-based) | 169 | 9.9 | 474 | 9.3 | |
| Group 2 (mitomycin-based) | 260 | 15.3 | 767 | 15.0 | |
| Group 3 (taxanes) | 20 | 1.2 | 60 | 1.2 | |
| Group 4 (others) | 1252 | 73.6 | 3802 | 74.5 | |
| Death | 849 | 3490 | |||
1Pearson's chi-square test for categorical variables and t-test for continuous variables.21US $ = 32.3 New Taiwan Dollars (NTD) in year 2008.
Table 2 shows overall survival in patients with gastric cancer among TCM nonusers, short-term TCM users, and long-term TCM users. Figure 2 shows Kaplan–Meier curves for overall survival in patients with gastric cancer among TCM nonusers, short-term TCM users, and long-term TCM users.
Table 2.
Data showing overall survival in patients with gastric cancer after surgery and adjuvant chemotherapy among TCM nonusers, short-term TCM users, and long-term TCM users.
| TCM use (days) | Death | Total follow-up (person-year) | Incidence rate1 | 95% CI | Mean follow-up (year) | |
|---|---|---|---|---|---|---|
| <30 (N = 5103) | 3490 | 25445.3 | 13715.7 | 13268.1 | 14178.4 | 5.0 |
| 30–179 (N = 1178) | 630 | 7915.9 | 7958.7 | 7360.9 | 8605.1 | 6.7 |
| ≥180 (N = 523) | 219 | 4163.1 | 5260.5 | 4608.0 | 6005.5 | 8.0 |
1Per 100,000 person-years. 2TCM nonusers: TCM use <30 days; short-term TCM users: TCM use 30–179 days; long-term TCM users: TCM use≥180 days.
Figure 2.
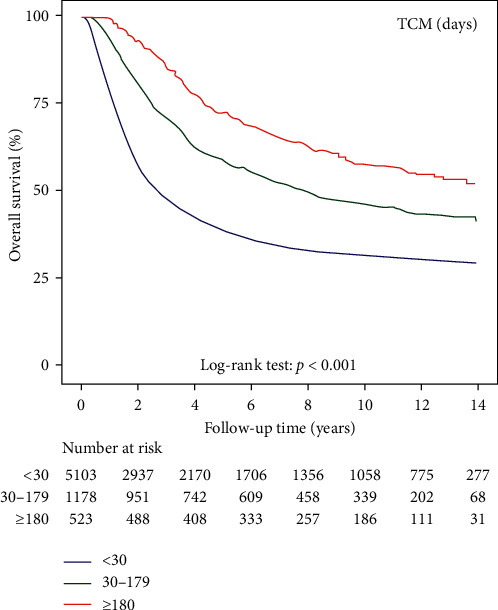
Kaplan–Meier curves of overall survival in patients with gastric cancer after surgery and adjuvant chemotherapy among TCM nonusers, short-term TCM users, and long-term TCM users.
After adjusting for sex, age, urbanization level, and income level in the main model, short-term and long-term TCM users were independently associated with a decreased risk of death with HRs of 0.59 (95% CI, 0.55–0.65) in TCM users and 0.41 (95% CI, 0.36–0.47) in TCM nonusers. We obtained similar results when covariates were adjusted for in the main model, as well as for each additional covariate, namely, diabetes mellitus, hypertension, alcoholism, smoking-related disorder, chronic renal failure, liver cirrhosis, and chemotherapy regimen. In the subgroup analysis of sex and age, we observed similar HR trends in short-term and long-term TCM users among men (0.62 [95% CI, 0.55–0.69] and 0.45 [95% CI, 0.38–0.54], respectively), women (0.56 [95% CI, 0.49–0.64] and 0.36 [95% CI, 0.29–0.45], respectively), those aged <65 years (0.60 [95% CI, 0.54–0.67] and 0.38 [95% CI, 0.31–0.45], respectively), and those aged ≥65 years (0.58 [95% CI, 0.51–0.66] and 0.46 [95% CI, 0.38-057], respectively) (Table 3).
Table 3.
Cox model with hazard ratios and 95% confidence intervals of short-term users and long-term TCM users versus TCM nonusers.
| Variables | Short-term TCM users1 | Long-term TCM users2 | ||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p value | HR | 95% CI | p value | |||
| Main model3 | 0.59 | 0.55 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Additional covariates4 | ||||||||
| Main model + diabetes mellitus | 0.59 | 0.54 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + hypertension | 0.59 | 0.54 | 0.64 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + alcoholism | 0.59 | 0.55 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + smoking-related disorder | 0.59 | 0.55 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + chronic renal failure | 0.59 | 0.55 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + liver cirrhosis | 0.59 | 0.55 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Main model + chemotherapy regimen | 0.59 | 0.54 | 0.65 | <0.0001 | 0.41 | 0.36 | 0.47 | <0.0001 |
| Subgroup effects | ||||||||
| Sex | ||||||||
| Male | 0.62 | 0.55 | 0.69 | <0.0001 | 0.45 | 0.38 | 0.54 | <0.0001 |
| Female | 0.56 | 0.49 | 0.64 | <0.0001 | 0.36 | 0.29 | 0.45 | <0.0001 |
| Age at surgery, years | ||||||||
| 18–64 | 0.60 | 0.54 | 0.67 | <0.0001 | 0.38 | 0.31 | 0.45 | <0.0001 |
| ≥65 | 0.58 | 0.51 | 0.66 | <0.0001 | 0.46 | 0.38 | 0.57 | <0.0001 |
1Short-term TCM users: TCM use 30–179 days. 2Long-term TCM users: TCM use≥180 days. 3Main model is adjusted for sex, age, urbanization level, and income level. 4Models were adjusted for covariates in the main model as well as for each additional listed covariate.
Table 4 lists single herbs and herbal formulas most commonly prescribed for gastric cancer after surgery and adjuvant chemotherapy in our cohort, including the prescription frequencies, average prescription durations, and average daily doses. The single herb most commonly prescribed in our cohort was Hwang-Chyi (Radix Hedysari; 11.8%), followed by Dan-Shen (Radix Salviae Miltiorrhizae; 9.8%), Yan-Hu-Suo (Rhizoma Corydalis; 9.4%), Bai-Hua-She-She-Cao (Herba Hedyotidis Diffusae; 9.2%), and Hou-Pu (Cortex Magnoliae; 9.0%). Xiang-Sha-Liu-Jun-Zi-Tang (15.5%) was the herbal formula most commonly prescribed in our cohort, followed by Ping-Wei-San (12.6%), Ban-Xia-Xie-Xin-Tang (11.8%), Bu-Zhong-Yi-Qi-Tang (10.3%), and Shen-Lin-Bai-Zhu-San (10.2%).
Table 4.
Single herbs and herbal formulas most commonly prescribed for gastric cancer after surgery and adjuvant chemotherapy in our cohort.
| Chinese herbal name | No. of users | % | Average duration (day) | Daily dose (g) |
|---|---|---|---|---|
| Single herbs | ||||
|
| ||||
| Hwang Chyi (Radix Hedysari) | 201 | 11.8 | 9.3 | 1.7 |
| Dan-Shen (Radix Salviae Miltiorrhizae) | 166 | 9.8 | 8.9 | 1.5 |
| Yan-Hu-Suo (Rhizoma Corydalis) | 160 | 9.4 | 7.8 | 1.5 |
| Bai-Hua-She-She-Cao (Herba Hedyotidis Diffusae) | 157 | 9.2 | 11.1 | 1.7 |
| Hou-Pu (Cortex Magnoliae) | 153 | 9.0 | 8.7 | 1.4 |
|
| ||||
| Herbal formulas | ||||
|
| ||||
| Xiang-Sha-Liu-Jun-Zi-Tang | 264 | 15.5 | 8.9 | 4.6 |
| Ping-Wei-San | 214 | 12.6 | 7.9 | 4.0 |
| Ban-Xia-Xie-Xin-Tang | 200 | 11.8 | 8.2 | 4.4 |
| Bu-Zhong-Yi-Qi-Tang | 175 | 10.3 | 9.2 | 4.7 |
| Shen-Lin-Bai-Zhu-San | 174 | 10.2 | 9.5 | 4.9 |
The daily doses of the most commonly prescribed single herbs and herbal formulas were in the ranges of 1.4–1.7 g and 4.0–4.9 g, respectively. The average duration of single herbs and herbal formulas most commonly prescribed ranged from 7.8 to 11.1 days.
4. Discussion
This study has several merits. Because our population data set was directly obtained from the RCIPD, our study enrolled all patients with gastric cancer between 1999 and 2008 in Taiwan instead of a representative sample. In addition, our study cohort was obtained from the RCIPD, which is highly accurate due to its high demand for implicating catastrophic illness.
A previous study demonstrated that TCM enhanced the survival of patients with gastric cancer. [6] As the tumor stage could not be defined, the previous study could not reveal the potential relationship between adopted therapies and differences in disease severity. However, because in the present study we examined patients with gastric cancer who underwent chemotherapy following surgery, our study cohort had similar disease severity levels and stages. Based on propensity score matching, we increased homogeneity between TCM users and nonusers and reduced the number of nonmatched users as much as possible. After propensity score matching, only 20 (1.16%) of 1721 TCM users could not be matched in our study, whereas more than 25% of TCM users could not be matched in the previous study. In addition, we classified TCM users into short-term users who used TCM for less than 180 days and long-term users who used TCM for 180 days or more to observe the effect of long-term TCM use. To verify our results, we adjusted additional covariates, namely, diabetes mellitus, hypertension, alcoholism, smoking-related disorder, chronic renal failure, liver cirrhosis, and chemotherapy regimen, to examine whether results were consistent, and similar results in subgroup effects based on sex and age at surgery also confirmed our findings. Finally, because survival was calculated from the day TCM was taken in our study, we reduced immortal time bias as much as possible.
In Taiwan, CHPs are considered a modern form of decoctions because of their more consistent quality when compared with TCM. The NHI program reimburses patients fully for both single-herb products and multi-herb products prescribed. Chinese medical physicians used to prescribe one or more herbal formulas in combination with several single herbs in each prescription according to the state of illness of a patient.
In our study, half of the single herbs and herbal formulas most commonly prescribed that are listed in Table 4 are often used to treat ailments of the gastrointestinal system. Xiang-Sha-Liu-Jun-Zi-Tang, the most commonly prescribed herbal formula identified in the present study, was often used to treat upper gastrointestinal disorders, including indigestion, gastroesophageal reflux, and anorexia, [7, 8] and has been reported to prevent nausea, vomiting, and anorexia induced by chemotherapy in patients with cancer [9–11] and exert beneficial effects on gastrointestinal disorders, anorexia, and postoperative gastric ileus when used in combination with Western drugs. [12, 13] Ping-Wei-San is also often prescribed for the treatment of upper gastrointestinal disorders, including esophageal reflux, gastritis, gastric or duodenal ulcers, and enteritis. [14–16] Furthermore, Ban-Xia-Xie-Xin-Tang has been reported to reduce diarrhea during chemotherapy [17, 18] and could prevent chemotherapy-induced oral mucositis in esophageal cancer [19] and in chemoradiation of head and neck cancers. [20] Shen-Ling-Bai-Zhu-San is one of the most common formulas used for the treatment of ulcerative colitis [21, 22] and has also been reported to reduce gastric cancer chemotherapy-induced toxicity. [23] Hou-Pu (Cortex Magnoliae) had been demonstrated to be beneficial for the treatment of gastrointestinal disorders. [24] Huang-Chyi (Radix Hedysari), which was the most commonly prescribed single herb in our study, and Bu-Zhong-Yi-Qi-Tang have been demonstrated to alleviate cancer-related fatigue. [25–27] Dan-Shen (Radix Salviae Miltiorrhizae) and Bai-Hua-She-She-Cao (Herba Hedyotidis Diffusae) have been shown to have anticancer effects, [28–30] whereas Bai-Hua-She-She-Cao (Herba Hedyotidis Diffusae) is the most common single herb prescribed for patients with colon cancer and breast cancer in Taiwan. [31, 32] Finally, Yan-Hu-Suo (Rhizoma Corydalis) showed pain control benefits. [33, 34].
Our study has some limitations that should be addressed. First, the NHI program only reimburses the cost of CHPs prescribed by Chinese medical physicians. Therefore, CHPs or decoctions purchased directly from TCM pharmacies were not included in our analysis. Consequently, the frequency of TCM use could have been underestimated in the present study. Nevertheless, because the NHI program has a comprehensive cover for CHPs prescribed by Chinese medical physicians, which is generally lower than the cost of CHPs or decoctions sold in TCM pharmacies, the underestimation would likely be minimal. In the present study, we could not verify exact dosages taken by enrolled patients. We could only assume that patients took medications as prescribed, which may overestimate the actual ingested dosage because some degree of noncompliance is always anticipated. Furthermore, detailed information, such as living environment, lifestyle, nutrition, and other examination data, were not available from the RCIPD. Finally, the stages of cancer were not recorded in the RCIPD. Nevertheless, we controlled the severity of cancer in our study cohort to some extent by selecting patients with gastric cancer undergoing chemotherapy after surgery.
5. Conclusions
In conclusion, in our study, TCM use was associated with higher survival in patients with gastric cancer after surgery and adjuvant chemotherapy. TCM could be adopted as a CAM therapy in patients with gastric cancer after surgery and adjuvant chemotherapy.
Acknowledgments
The authors thank the Health Information and Epidemiology Laboratory of Chang Gung Memorial Hospital, Chiayi Branch, for the comments on the study and assistance with data analysis. This study was supported by a grant from Chang Gung Memorial Hospital, Chiayi Branch, Taiwan (CFRPG6K0021). This study was based on a portion of data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health, which is managed by the National Health Insurance Research Institutes, Taiwan.
Abbreviations
- TCM:
Traditional Chinese medicine
- CAM:
Complementary and alternative medicine
- CHPs:
Chinese herbal products
- NHI:
National Health Insurance
- NHIRD:
National Health Insurance Research Database
- RCIPD:
Registry of Catastrophic Illness Patient Database
- ICD-9-CM:
International Classification of Diseases, Ninth Revision, Clinical Modification
- HRs:
Hazard ratios
- CI:
Confidence interval.
Data Availability
The data sets used and analyzed in this study are available from the corresponding author on reasonable request.
Disclosure
The funding body played no role in study design, analysis, and interpretation of data in this paper. Also, the statistical results and conclusions presented in this paper do not represent those of the Bureau of National Health Insurance, Department of Health, or the National Health Insurance Research Institutes.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
WTS and CYW contributed to study conception and design. Acquisition of data was carried out by YHY. Analysis and interpretation of data was performed by PRY and YCS. Drafting of manuscript was done by WTS. Critical revision was done by CYW.
References
- 1.Bray F., Ferlay J., Soerjomataram I., Siegel R. L., Torre L. A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer Journal for Clinicians. 68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J., Ervik M., Lam F., et al. Global cancer observatory: cancer today. Breast Cancer Epidemiology. 2010:1–19. [Google Scholar]
- 3.cancer J. G. C. A. J. G. Japanese gastric cancer treatment guidelines 2014. Gastric Cancer. 20(1):1–19. doi: 10.1007/s10120-016-0622-4. (ver. 4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coburn N., Cosby R., Klein L., et al. Staging and surgical approaches in gastric cancer: a systematic review. Cancer Treatment Reviews. 63:104–115. doi: 10.1016/j.ctrv.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Allemani C., Matsuda T., Di Carlo V., et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 391(10125):1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hung K. F., Hsu C. P., Chiang J. H., et al. Complementary Chinese herbal medicine therapy improves survival of patients with gastric cancer in Taiwan: a nationwide retrospective matched-cohort study. Journal of Intercultural Ethnopharmacology. 199:168–174. doi: 10.1016/j.jep.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Oka T., Okumi H., Nishida S., et al. Effects of Kampo on functional gastrointestinal disorders. BioPsychoSocial Medicine. 8(1):p. 5. doi: 10.1186/1751-0759-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tominaga K., Arakawa T. Kampo medicines for gastrointestinal tract disorders: a review of basic science and clinical evidence and their future application. Journal of Gastroenterology. 48(4):452–462. doi: 10.1007/s00535-013-0788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harada T., Amano T., Ikari T., et al. Rikkunshito for preventing chemotherapy-induced nausea and vomiting in lung cancer patients: results from 2 prospective, randomized phase 2 trials. Frontiers in Pharmacology. 8:p. 972. doi: 10.3389/fphar.2017.00972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ohnishi S., Watari H., Kanno M., et al. Additive effect of rikkunshito, an herbal medicine, on chemotherapy-induced nausea, vomiting, and anorexia in uterine cervical or corpus cancer patients treated with cisplatin and paclitaxel: results of a randomized phase II study (JORTC KMP-02) Journal of Gynecologic Oncology. 28(5) doi: 10.3802/jgo.2017.28.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshiya T., Ito M., Misumi K., et al. The effect of rikkunshito, a traditional Japanese herbal medicine, on food intake and plasma acylated ghrelin levels in lung cancer patients treated with platinum-based chemotherapy. Annals of Oncology. 27(6) [Google Scholar]
- 12.Mogami S., Hattori T. J. E.-B. C., Medicine A. Beneficial effects of rikkunshito, a Japanese kampo medicine, On Gastrointestinal Dysfunction and Anorexia in Combination with Western Drug: A Systematic Review. Evidence-Based Complementary and Alternative Medicine. 2014;2014:7. doi: 10.1155/2014/519035.519035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Endo M., Hori M., Ozaki H., Oikawa T., Hanawa T. J. J. Rikkunshito, a Kampo medicine, ameliorates post-operative ileus by anti-inflammatory action. Journal of Pharmacological Sciences. 124(3):374–385. doi: 10.1254/jphs.13182fp. [DOI] [PubMed] [Google Scholar]
- 14.Cha J. Y., Jung J. Y., Jung J. Y., et al. Inhibitory effects of traditional herbal formula pyungwi-san on Inflammatory Response in Vitro and in Vivo. Evidence-Based Complementary and Alternative Medicine. 2013;2013:19. doi: 10.1155/2013/630198.630198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seo C. S., Lee J.-A., Jung D., et al. Simultaneous determination of liquiritin, hesperidin, and glycyrrhizin by HPLC-photodiode array detection and the anti-inflammatory effect of Pyungwi-san. Archives of Pharmacal Research. 34(2):203–210. doi: 10.1007/s12272-011-0204-2. [DOI] [PubMed] [Google Scholar]
- 16.Tiong C., Liang W.-L., Liu H.-Y., et al. Gastroprotective Effects of Ping-Wei San on Indomethacin-lnduced Gastric Ulcer. Journal of Food and Drug Analysis. 19(4) [Google Scholar]
- 17.Hoshi N., Kofunato Y., Yashima R., Shimura T., Takenoshita S. J. G. chemotherapy Treating side effects of FOLFIRINOX--A study of the effect of hange-shashin-to on preventing diarrhea. American Journal of Gastroenterology. 42(12):2364–2366. [PubMed] [Google Scholar]
- 18.Yamaguchi O., Kawashima A., Shiono A., et al. Hange-Shashin-to for preventing diarrhea during afatinib therapy. Pediatrics (Childhood Diarrhea) 42(5):581–583. [PubMed] [Google Scholar]
- 19.Takahashi M., Nakajima M., Muroi H., et al. Prevention of the chemotherapy-induced oral mucositis in esophageal cancer by use of hangeshashinto (TJ-14) International Surgery. 103(7):401–408. [Google Scholar]
- 20.Yamashita T., Araki K., Tomifuji M., Kamide D., Tanaka Y., Shiotani A. J. S. A traditional Japanese medicine—Hangeshashinto (TJ-14) —alleviates chemoradiation-induced mucositis and improves rates of treatment completion. Supportive Care in Cancer. 23(1):29–35. doi: 10.1007/s00520-014-2315-z. [DOI] [PubMed] [Google Scholar]
- 21.Yang L., Song Y., Jin P., et al. Shen-Ling-Bai-Zhu-San for ulcerative colitis: Protocol for a systematic review and meta-analysis. Medicine. 97:38. doi: 10.1097/MD.0000000000012337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SaÅ‚aga M., Zatorski H., Sobczak M., Chen C., Fichna J. J. C. Chinese herbal medicines in the treatment of IBD and colorectal cancer: a review. Current Treatment Options in Oncology. 15(3):405–420. doi: 10.1007/s11864-014-0288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tian H., Shang J., Ji Z. Curative effect of Shenling Baizhu powder on chemotherapy-induced toxicity in advanced gastric cancer. Indian Journal of Pharmaceutical Sciences. 82(s1) [Google Scholar]
- 24.Luo H., Wu H., Yu X., et al. A review of the phytochemistry and pharmacological activities of Magnoliae officinalis cortex. Journal of Ethnopharmacology. 236:412–442. doi: 10.1016/j.jep.2019.02.041. [DOI] [PubMed] [Google Scholar]
- 25.Jung Y., Jerng U., Lee S. A systematic review of anticancer effects of Radix Astragali. Chinese Journal of Integrative Medicine. 22(3):225–236. doi: 10.1007/s11655-015-2324-x. [DOI] [PubMed] [Google Scholar]
- 26.Yang L., Li T.-t., Chu Y.-t., et al. Traditional Chinese medical comprehensive therapy for cancer-related fatigue. Chinese Journal of Integrative Medicine. 22(1):67–72. doi: 10.1007/s11655-015-2105-6. [DOI] [PubMed] [Google Scholar]
- 27.Jeong J. S., Ryu B. H., Kim J. S., Park J. W., Choi W. C., Yoon S. W. J. I. Bojungikki-tang for cancer-related fatigue: a pilot randomized clinical trial. Integrative Cancer Therapies. 9(4):331–338. doi: 10.1177/1534735410383170. [DOI] [PubMed] [Google Scholar]
- 28.Wang T., Fu X., Wang Z. J. E.-B. C., Medicine A. Danshen Formulae for Cancer: A Systematic Review and Meta-Analysis of High-Quality Randomized Controlled Trials. Based Complementary and Alternative Medicine. 2019;2019:16. doi: 10.1155/2019/2310639.2310639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin J., Li Q., Chen H., Lin H., Lai Z., Peng J. J. O. . l. Hedyotis diffusa Willd. extract suppresses proliferation and induces apoptosis via IL-6-inducible STAT3 pathway inactivation in human colorectal cancer cells. Oncology Letters. 9(4):1962–1970. doi: 10.3892/ol.2015.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang P., Zhang B., Gu J., et al. The study of the effect of Hedyotis diffusa on the proliferation and the apoptosis of the cervical tumor in nude mouse model. Cell Biochemistry and Biophysics. 72(3):783–789. doi: 10.1007/s12013-015-0532-9. [DOI] [PubMed] [Google Scholar]
- 31.Chao T.-H., Fu P.-K., Chang C.-H., et al. Prescription patterns of Chinese herbal products for post-surgery colon cancer patients in Taiwan. Journal of Ethnopharmacology. 155(1):702–708. doi: 10.1016/j.jep.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 32.Yeh Y.-C., Chen H.-Y., Yang S.-H., et al. Hedyotis diffusa combined with scutellaria barbata are the core treatment of Chinese herbal medicine used for breast cancer patients: a population-based study. Evidence-Based Complementary and Alternative Medicine. 2014;2014:19. doi: 10.1155/2014/202378.202378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiao W.-P., Yang Y.-F., Wu H.-Z., Xiong Y. Predicting the mechanism of the analgesic property of yanhusuo based on network pharmacology. Natural Product Communications. 14(10) doi: 10.1177/1934578x19883071.1934578X19883071 [DOI] [Google Scholar]
- 34.Wang L., Zhang Y., Wang Z., et al. The antinociceptive properties of the corydalis yanhusuo extract. Plos One. 11(9) doi: 10.1371/journal.pone.0162875.e0162875 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets used and analyzed in this study are available from the corresponding author on reasonable request.


