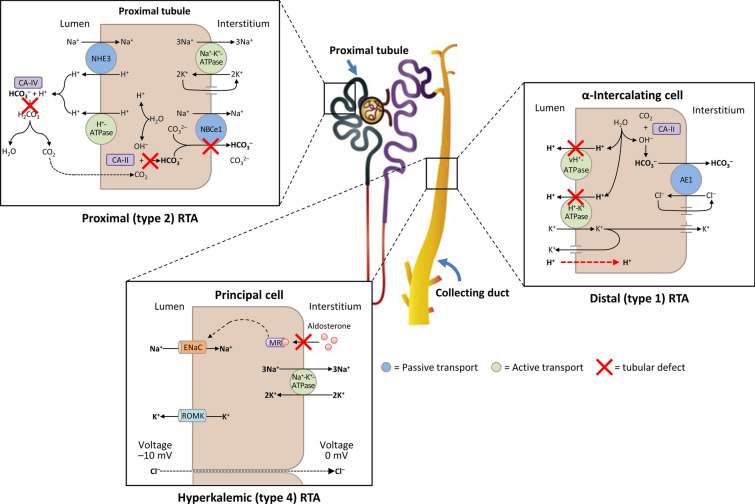
Fig. 3.
A schematic diagram illustrating the underlying kidney tubule defects causing the different types of renal tubular acidosis (RTA). Distal (type 1) RTA is caused by either impaired hydrogen (H+) secretion by vacuolar (v) H+-ATPase or H+/K+-ATPase or increased H+ permeability of luminal membrane by α-intercalated cells of the collecting duct, which leads to a reduction in net H+ secretion. Proximal (type 2) RTA is caused by defects in bicarbonate (HCO3–) reabsorption in the proximal tubule, due to either impaired HCO3– transport across the basolateral membrane or inhibition of carbonic anhydrase (CA) activity. Hyperkalemic (type 4) RTA is caused by aldosterone deficiency or resistance, which leads to reduced Na+ (sodium) reabsorption by principal cells of the collecting duct and decreased transepithelial voltage, leading to diminished H+ secretion by α-intercalated cells and K+ secretion by principal cells. AE1 kidney anion exchanger, ENaC epithelial Na+ channel, MR mineralocorticoid receptor, NHE3 Na+/H+ exchanger 3, ROMK apical membrane K+ channel