Abstract
Physical activity (PA) is an effective depression treatment. However, knowledge on how variation in day-to-day PA relates to depression in women is lacking. The purposes of this study were to 1) compare overall objectively measured baseline daily steps and duration of moderate to vigorous PA (MVPA) and 2) examine differences in steps and MVPA on days of the week between women aged 25–65 years, who were physically inactive, with high and low depressive symptoms, enrolled in a run-in period of the mobile phone based physical activity education (mPED) trial. The Center for Epidemiological Studies Depression Scale was used to categorize low/high depressive symptom groups. We used linear mixed-effects models to examine the associations between steps and MVPA and depression-status overall and by day of the week, adjusting for selected demographic variables and their interactions with day of the week. 274 women were included in the final analysis, of which 58 had high depressive symptoms. Overall physical activity levels did not differ. However, day of the week modified the associations of depression with MVPA (p = 0.015) and daily steps (p = 0.08). Women with high depression were characterized by reduced activity at the end of the week (Posthoc: Friday: 791 fewer steps, 95% CI: 73–1509, p = 0.03; 8.8 lower MVPA, 95% CI: 2.16–15.5, p = 0.0098) compared to women with low depression, who showed increased activity. Day of the week might be an important target for personalization of physical activity interventions. Future work should evaluate potential causes of daily activity alterations in depression in women.
Keywords: Depressive symptoms, Pedometer, Physical activity, Mobile phone, mHealth
1. Introduction
Physical inactivity and depression are major global health problems. Both diseases are risk factors for many chronic illnesses, including cardiovascular disease (Penninx, 2017), diabetes (Santos et al., 2018) and obesity (Wyatt et al., 2006, Williams et al., 2015). The prevalence of both physical inactivity (Troiano et al., 2008, Kao et al., 2014) and depression (Kuehner, 2017) in women is higher than in men. For example, in previous work the percentage of women that adhered to physical activity guidelines was 18.0% versus 22.9% in men measured by self-report in almost 400.000 US adults Bennie et al. (2019). Further, data from the National Health and Nutrition Examination Survey collected in 2013–2016 shows that depression is twice as prevalent among American women over the age of 20 than in men (Brody et al., 2018). Therefore, it is of particular interest to study the relationship between depression and physical activity in women.
A growing body of evidence shows that physical inactivity and depression are related (Al-Qahtani et al., 2018, Ströhle, 2009). For instance, in a meta-analysis of 25 studies, lower self-reported physical activity levels were significantly associated with a higher risk of subsequent depression. Mammen and Faulkner (2013) Further, in a cohort study of over 30.000 healthy adults, individuals who did not engage in physical activity had a 44% increased risk of lifetime depression as compared to those with at least one hour of moderate or vigorous intensity physical activity (MVPA) per week (Harvey et al., 2017). Additionally, engaging in regular physical activity significantly improved depressive symptoms and a higher duration and intensity of physical activity was also associated with greater improvement (Mata et al., 2012).
There is strong evidence that encouraging physical activity is a valuable mental health promotion strategy from a population health perspective as it may reduce the risk of developing clinical depression (Mammen and Faulkner, 2013). Both mobile health interventions (Romeo et al., 2019) and face-to-face treatments Murray et al. (2017) have shown moderate effect-sizes, though their effects seem to diminish over time (Yerrakalva et al., 2019). In order to design effective physical activity interventions, we need to improve our understanding of physical activity patterns throughout the week in individuals with depressive symptoms. To date, most studies explored depression in relation to self-report measure of physical activity that are susceptible to both overestimation and underestimation of true physical activity levels due to social desirability and recall biases (Prince et al., 2008). We also published a paper demonstrating a large discrepancy between self-reported physical activity and objectively measured activity (Fukuoka et al., 2016) and also highlighted the inability to capture the absolute level of physical activity by self-report.
Physical activity patterns in individuals with no depressive symptoms appear to differ from day to day. For example, in youth, Wednesdays, Thursdays and Sundays were associated with a lower probability of meeting physical activity guidelines (Moore et al., 2014) based on self-report physical activity. Further, in urban adults in the United Kingdom, physical activity was lower on Sundays compared to weekdays and Saturdays (Davis et al., 2011) based on accelerometer data. In a 12-month study with Latina women using pedometers during a physical activity intervention, physical activity was higher on weekdays (Carr et al., 2016). By contrast, one study in older adults using a body-fixed sensor to measure physical activity for seven days found no differences between weekend and weekday physical activity (Nicolai et al., 2010). However, we do not know whether these findings can be generalizable to women with depressive symptoms. Here we explore the role of diminished activity in depression in women. This will help us understand relationships between physical inactivity and depression and design more targeted interventions. For example, this study can identify time varying and time fixed variables that we could use for personalization of physical activity interventions.
The purposes of this analysis are 1) to compare differences in objectively measured baseline physical activity levels (total daily steps and duration of MVPA minutes per day) between women with high and low depressive symptoms, and 2) to examine differences in the patterns of total daily steps and MVPA between the two groups on different days of the week (Monday through Sunday). We used the data from the mobile phone based physical activity education (mPED), a randomized controlled clinical trial (RCT) designed to evaluate the efficacy of a mobile app and accelerometer delivered physical activity intervention for physically inactive women.
2. Methods
2.1. Study design and sample
We analyzed the sociodemographic, clinical, and self-reported questionnaire data collected at the screening/baseline study visit and accelerometer data collected during the run-in period prior to a randomization visit in the mPED trial. Detailed descriptions of the study design and outcomes have been previously published (Fukuoka et al., 2011, Fukuoka et al., 2018, Fukuoka et al., 2019, Fukuoka et al., 2017, Fukuoka et al., 2015, Fukuoka et al., 2018, Lindgren et al., 2019, Zhou et al., 2019). In short, eligibility criteria were female sex, age from 25 to 65 years, body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) of 18.5 to 43.0, physically inactive at work and/or during leisure time based on the Stanford Brief Activity Survey, intent to be physically active, access to a home telephone or mobile phone, ability to speak and read English, no medical conditions or physical problems that required special attention in an exercise program, no current participation in other lifestyle modification programs, and no mild cognitive impairment as determined by the Mini-Cog test. This trial was not designed specifically for women with high depressive symptoms. Physical activity data were collected by accelerometer every day during the run-in period.
2.2. Procedures
During the screening/baseline visit, sociodemographics, medical and lifestyle history, the Center for Epidemiological Studies Depression Scale (CES-D) (Weissman et al., 1977), body mass index (BMI) were assessed by a trained research staff. At the end of this visit, eligible participants were issued a run-in app and an accelerometer and brief training was provided to insure participants could successfully use both devices. During the run-in period, all participants were asked to use the study app, wear an Omron Active Style Pro HJA-350IT with triaxial accelerometer every day, and not to increase their activity and not to change their lifestyle. The run-in period lasted approximately 3 weeks and no physical activity intervention was delivered during this period. A run-in mobile phone app was created specifically for this phase of the study and it was designed to mimic the intervention app without any content to encourage or support increasing physical activity. Participants were instructed to interact with the run-in app twice a day. First, they received a pre-programmed message between 11 a.m. to 3p.m.; such as, “Are you wearing a pedometer now?” “No” or “Yes” was selected by pushing the keypad. If “No” was selected, the next screen displayed “Please wear a pedometer all day, except for showering and swimming.” If “Yes” was selected, the next screen displayed “a great job.” Second, participants were instructed to enter an estimate of their daily step count into the app’s daily activity diary every night of the run-in period. None of the estimated daily step counts were used in this paper.
2.3. Measures
Depressive symptoms: The Center for Epidemiological Studies Depression Scale (CES-D) (Weissman et al., 1977) was used to assess self-reported depressive symptoms. The CES-D is a valid and reliable instrument that is widely used to assess depressive symptoms in a research context. It contains 20 items about symptoms that occurred in the week prior to the screening with response options from 0 to 3 that refer to frequency of the symptoms. Scores range from 0 to 60, with high scores indicating greater depressive symptoms. A cutoff score of 16 aids in identifying individuals at risk for clinical depression. For the purpose of this analysis, women with CES-D scores ≥ 16 were considered “high depressive symptoms” and women with scores < 16 were considered “low depressive symptoms.”
Objectively measured physical activity: The Omron Active Style Pro HJA-350IT with triaxial accelerometer was selected for this trial because it has well-established reliability and validity and records 150 days of daily activity data. The accelerometer was set to record and store physical activity (e.g. steps), but not to display the steps counts (only the current date and time were visible on the display). This accelerometer was programed to collect daily steps and physical activity intensity (metabolic equivalent values [METs]). The mean intensity value of a 1-minute epoch was calculated as the average value of six 10-second epochs. The METs determined by this accelerometer are closely correlated with METs calculated using energy expenditure measured by indirect calorimetry. Participants were asked to wear this device all day, except when showering/bathing, swimming, or sleeping, from the time they got up in the morning until the time they went to bed at night for the duration of the run-in period. In order for accelerometer data to be valid for this analysis, participants have to wear the accelerometer for at least 8-hour per day for a minimum of 7 days. We did not collect detailed information on reasons that subjects did not wear the accelerometer. MVPA was defined as ≥ 3 metabolic equivalents (METs), based on the Compendium of Physical Activity (Ainsworth et al., 1993). To closely match with the 2018 Physical Activity Guidelines for Americans, total weekly minutes of MVPA were estimated as physical activity ≥ 3 METs lasting at least 1 min in duration. In this study we used the actual minutes of MVPA and the number of steps. Steps and MVPA are correlated in this study (Pearson r = 0.8). Unlike MVPA, participants intuitively understand daily steps. However, daily steps does not take into account the intensity of physical activity levels (O’Brien et al., 2018). Thus, we presented both outcomes.
Other measures: A research staff asked the participants to fill out the sociodemographic and medical from immediately after participants completed the written consent form. The emotional support question, “How many people can you count on to provide you with emotional support?”, was developed by the research team. To calculate body mass index (BMI), weight was measured with a Tanita WB-110 digital electronic scale, and height was measured at baseline with a standard stadiometer.
2.4. Statistical analysis
Descriptive statistics were used to summarize participant characteristics. Women with high/low depression were compared using t, Mann Whitney, chis-square and Fisher’s exact tests as appropriate.
We used linear mixed models (LMMs) to examine whether women with high vs low depressive symptoms differed in average daily step counts and MVPA minutes per day. Based on prior evidence, we included self-reported emotional support, BMI, employment (paid work, yes or no), time in study, age, and day of the week, in addition to depression-status, as covariates in the model (Tudor-Locke et al., 2004, Strine et al., 2008, Ludwig et al., 2018). We additionally corrected for daily time spent wearing the Omron device. We then examined modification of between-group differences by day of week using an augmented LMM adding interactions of depressive group as well as covariates with day of the week (Monday through Sunday). We used likelihood ratio (LR) tests to ensure adequate modeling of the covariance structure of the repeated outcomes, as recommended by Barr et al. (2013), first adding a random slope in for time (study day) to the initial random-intercept model, then further allowing for AR(1) residuals, as previous studies showed autocorrelation for physical activity patterns over time (Korinek et al., 2018). We also used LR tests to assess the need for more flexible modeling of secular trend in study day. Model assumptions were further checked by visual inspections of residual plots. Analyses were carried out in R studio V. 1.1.423 using the nmle package (Pinheiro et al., 2017). To estimate and plot marginal means (effects of independent variables adjusted for all other covariates and interactions), we used the ggeffects package (Lüdecke, 2018).
3. Results
3.1. Participants
318 women came to the screening/baseline visit, but nine did not meet the eligibility criteria. The remaining 309 started the run-in period (Fukuoka et al., 2015). See Supplementary Flowchart. After removing participants who had less then 7 days in total of suitable data available (i.e. > 8 h recorded wearing time), 274 women were included in the analysis. The distribution of available weekdays for both groups is shown in supplemental Table 1. Of these, 216 (78%) participants had low depressive symptoms (CESD < 16) and 58 (22%) participants had high depressive symptoms. The median CESD score was 8.00 (IQR: 4/8/14). Table 1. shows baseline characteristics with differences between high and low depression groups. High and low depression groups statistically differed on self-reported health (p = 0.021), antidepressant-use (p = 0.015), and emotional support (p = 0.001).
Table 1.
Univariate Comparisons of Participants with and without clinically significant depressive symptoms at baseline (n = 275).
| Low depressive symptoms (CES-D < 16) (n = 216) |
High depressive symptoms (CES-D >=16) (n = 58) | p-value | |
|---|---|---|---|
| Age Median (Upper/lower quantile) | 56.0 (44–61) | 50.5 (41–59) | 0.067 |
| Race/Ethnicity | 0.92 | ||
| Native Hawaiian/Pacific Islander | 1 (0.5%) | 0 (0%) | |
| Black/African-American | 21 (9.7%) | 5 (8.6%) | |
| Hispanic/Latino | 13 (6.0%) | 4 (6.9%) | |
| Asian | 49 (22.7%) | 10 (17.2%) | |
| White (non-Hispanic) | 113 (51.9%) | 34 (58.6%) | |
| >1 race | 20 (9.3%) | 5 (8.6%) | |
| Education | 0.32 | ||
| Completed High School & some college | 55 (25.5%) | 14 (24.1%) | |
| Completed College | 82 (38.0%) | 28 (48.3%) | |
| Completed Graduate School | 80 (36.7%) | 16 (27.6%) | |
| Household Income | 0.44 | ||
| Under 40,000 | 35 (16.2%) | 14 (24.1%) | |
| 40,001 to 75,000 | 52 (24.1%) | 11 (19.0%) | |
| Over 75,000 | 112 (51.9%) | 27 (46.6%) | |
| Don't know or Declined to state | 17 (7.9%) | 6 (10.3%) | |
| Marital status | 0.51 | ||
| Never married | 65 (30.1%) | 21 (36.2%) | |
| Currently married/cohabitating | 106 (49.1%) | 28 (48.3%) | |
| Divorced/widowed | 45 (20.8%) | 9 (15.5%) | |
| Employment and shift work | 0.20 | ||
| Full or Part time Job No Shift Work | 118 (54.6%) | 27 (46.6%) | |
| Full or Part time Job with Shift Work | 45 (20.8%) | 10 (17.2%) | |
| No paid employment | 53 (24.5%) | 21 (36.2%) | |
| Used a pedometer prior to the study | 99 (46.3%) | 28 (48.3%) | 0.90 |
| Previously participated in a weight loss/diet program | 128 (59.3%) | 36 (62.1%) | 0.81 |
| Health variables | |||
| Self-reported health (Mean, SD) | 5.01 (1.05) | 4.62 (1.15) | 0.021 |
| Antidepressant use (%) | 40 (18.5%) | 20 (34.5%) | 0.015 |
| Emotional support (Mean, SD) | 2.80 (0.464) | 2.53 (0.863) | 0.0013 |
| Body mass index, kg/m (Mean, SD) | 29.7 (6.06) | 29.8 (6.38) | 0.89 |
| Self-reported high blood pressure (%) | 0.29 | ||
| No | 153 (70.8%) | 46 (79.3%) | |
| Yes | 58 (26.9%) | 12 (20.7%) | |
| Don't know | 5 (2.3%) | 0 (0%) | |
| Self-reported high cholesterol (%) | 0.37 | ||
| No | 113 (52.3%) | 36 (62.1%) | |
| Yes | 71 (32.9%) | 14 (24.1%) | |
| Don’t know | 32 (14.8%) | 8 (13.8%) | |
| Reached menopause (%) | 59% | 50% | 0.25 |
3.2. Physical activity
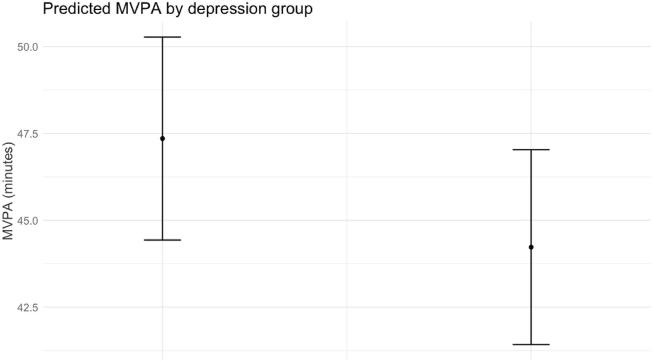
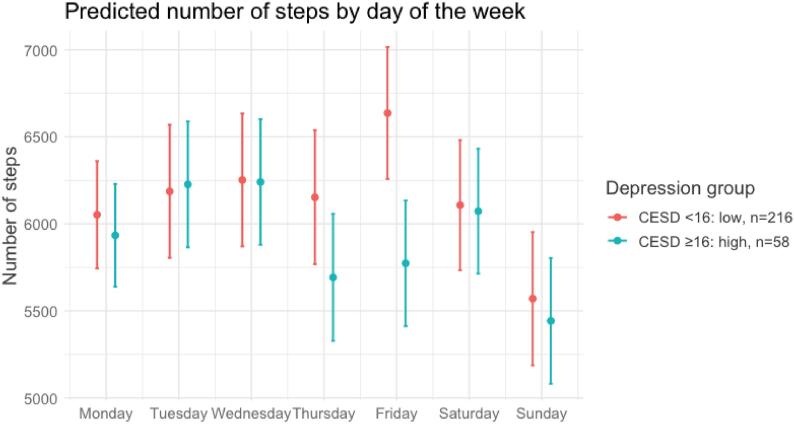
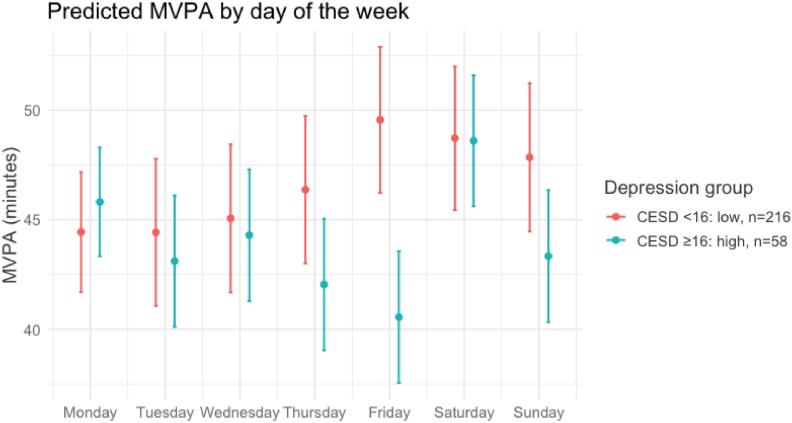
A total of 4811 days were available for the analysis with a mean available number of days of 17.6 (SD = 5.6) per participant. The mean number of aggregated steps per day (over the entire study period) was 6000 (SD = 1990) for the non-depressed group and 5560 (SD:2580) for the depressed group and MVPA per day was 46.5 (SD = 19.9) and 42.5 (SD = 22.7) minutes. Overall, we did not find any significant differences in total average daily steps (estimate = 112.3 fewer steps, 95% CI −182 to 407.3, p = 0.46) and MVPA minutes (estimate = 1.45 min /per day lower MVPA, 95% CI −1.31 to 4.23, p = 0.31) in women with high compared to low depressive symptoms, after adjusting for covariates specified a priori (see supplemental Table 2 and 3). However, these effects were modified by day of week for MVPA p = 0.015 for interaction. and for steps p = 0.08 for the interaction. Post-hoc analyses to quantify physical activity differences (adding dichotomous variables for every day in the model) showed that lower activity was most evident on Friday for women with high depressive symptoms (8.8 lower MVPA, 95% CI: 2.16 to 15.5, p = 0.0098 and 791 fewer steps, 95% CI: 73 to 1509, p = 0.03). Adjusted between-group differences extracted from these models overall, averaged over day of the week are shown in Fig. 1, Fig. 2. Differences by day of the week between women with high and low depressive symptoms are shown in Fig. 3, Fig. 4. The Supplemental Material shows the tables with the Type III (partial sum of squares) tests outcomes for all fixed effects of these four models, and figures to illustrate daily physical activity over time for the entire sample. In the Supplementary material, we also plot a post-hoc 3-way interaction between working status, weekday and depression-status. This 3-way interaction was not significant.
Fig. 1.
Marginal means plot for daily steps and depression groups.
Fig. 2.
Marginal means plot for moderate to vigorous physical activity (MVPA) minutes per day and depression group.
Fig. 3.
Marginal means plot for steps by day of the week and depression group.
Fig. 4.
Marginal means plot for MVPA (minutes of moderate to vigorous physical activity) by day of the week and depression group.
4. Discussion
This study did not identify overall differences in objectively measured total amount of daily physical activity for women with high compared to low depressive symptoms. However, there was a significant interaction between depressive symptom groups and day of the week for MVPA. Women with high depressive symptoms showed significantly reduced physical activity towards the end of the week, particularly for minutes of moderate or rigorous physical activity, most pronounced on Fridays, even after adjusting for potential confounding factors such as employment, BMI, emotional support and age, and their interactions with day of the week.
Although many studies found a relation between overall levels of physical activity and depressive symptoms (Al-Qahtani et al., 2018, Ströhle, 2009, Ludwig et al., 2018, Ku et al., 2018, Schuch et al., 2017) of which most were measured by self-report physical activity, a handful of studies that objectively measured physical activity did not observe this relationship (Mata et al., 2012, Whitaker et al., 2014). The results of this study suggest that differences in physical activity in depression (when measured objectively) might not lie in the total amount of activity, but rather in the day-to-day differences in patterns of physical activity.
Our finding of decreased physical activity towards the end of the week mainly on Friday for women with high depressive symptoms is intriguing and may have several potential explanations. First, Friday, the end of the working week, may be particularly associated with an increase in social physical activities for women with low, but not high depression. Leisure time physical activity has been associated with mental well being more than work related physical activity (White et al., 2017). Some studies observed that participating in physical activity in a club setting (sports club) or other organized activities is related to lower depressive symptoms (Kleppang et al., 2018, Prince et al., 2008). This suggests an important role of social physical activities: exercise that can be done in a social context such as in a group and physical activity. Second, though we corrected for working status in our models, findings could be associated with work related physical activity. When plotting results separately for working status in a posthoc analysis (see Supplementary material), we find that even when women are unemployed, women with high depression still walk less on Friday. Perhaps women with low depression are better able to compensate for missing out on work-related physical activities.
We did not measure if participants engaged in social physical activities throughout the week or exercised alone, and we did not assess which days were workdays or non-workdays for our individual participants. Thus, we are limited in making definite conclusions regarding the reasons for these outcomes. Our results reveal the complex nature of differences in physical activity between women with and without high depressive symptoms. Future work should therefore assess the relation between physical activity patterns throughout the week and accompanying emotions, social events and work-related activities in depression, for instance by combining accelerometer data with ecological mood monitoring and/or an activity dairy. This type of work could also provide insights on the direction of the relationship between depression and physical activity (e.g. previous work suggests a bidirectional relationship47), which we did not assess in the current study.
It is also of interest for future work to examine unique relationships between depression and physical activity for men and women. Globally, women are less active than men (Troiano et al., 2008, Kao et al., 2014). A recent meta-analysis found that for women, and not for men, increasing PA protected against depression (Gianfredi et al., 2020). However, this study also pointed out that only a few studies specifically examined the relationship between (objective) PA and depression in just men Gianfredi et al. (2020). Other work has shown that women aged > 60 prefer to exercise indoors as opposed to outdoors (van Uffelen et al., 2017) and a systematic review found that women walk more as a means to exercise than men Pollard and Wagnild, 2017. Regarding daily patterns, a UK biobank study of 96,600 individuals found that participants walked slightly less in the weekend, but that this did not differ by gender (Doherty et al., 2017). As far as we know, no studies examined differences in day of the week by depression status for men.
This research has potential implications for data-driven personalization of physical activity interventions for depression through apps or other digital tools. Currently, there are a few studies focusing on mobile health personalization. Some of these studies use machine learning to adapt the intervention content (Triantafyllidis and Tsanas, 2019). Our results provide preliminary evidence that for individuals with depression, day of the week might be an important factor for personalization. Improving personalization of physical activity interventions might increase the effectiveness of these interventions Zhou et al., 2019, Triantafyllidis and Tsanas, 2019 (Zhou et al., 2018). For example, content can be developed to specifically target increasing motivation towards the end of the working week, when individuals with depression may be less active. This is important as, though a wealth of research highlighted the benefits of physical activity on depression Schuch et al., 2016, previous work has also reported that physical activity interventions do not reduce depression (Chalder et al., 2012), or that the effects of these interventions on depression diminish after longer follow-up periods Krogh et al., 2011.
5. Strengths and limitations
Strengths of this work include the use of objectively measured physical activity in a relatively large sample of diverse women. To the best of our knowledge, this is the first study to report the specific patterns of objectively measured physical activity over different weekdays in relation to depressive symptoms. In addition, the accelerometer was set to not display the steps counts or other physical activity information (only the current date and time were visible on the display) during the run-in period. We believe that this display mode prevented participants increasing physical activity.
Despite these strengths, there are limitations to this study. First, we included a sample of female adults aged 25–69 years from the San Francisco Bay Area. The San Francisco Bay Area offers an extensive public transportation network that does not require a car to access the research office. Thus, findings from this study may not be generalizable to men or children, or to physically active women beyond the Bay Area. Second, while we adjusted for employment status in our analysis models (full-time/part-time versus no employment), we did not have physical activity information related to the nature or working hours of participants’ jobs. Lastly, we lack information on the types of physical activity, for example whether participants engaged in social or individual physical activity or leisure versus work or household related activity. This information may have shed more light on the nature of our findings. Further, another explanation for the lack of differences in overall PA between the depressed and non-depressed women could be related to a selection bias. Individuals with higher depressive symptoms may be less likely to participate in the 12-month physical activity intervention trial than those with lower depressive symptoms. The women with high depressive symptoms in this study might have been more motivated to become physically active than a general population sample with high depressive symptoms outside of the context of a physical activity study. Moreover, we excluded women who were already physically active prior to the study. Because of this, our study answers questions about physical inactivity in depression, not physical activity in general. These sample selection criteria might contribute to non-significant physical activity levels between the two groups.
6. Conclusion
We did not find differences in physical activity in low-active women who participated in a run-in period of a mobile physical activity intervention with high compared to low depressive symptoms in the total amount of physical activity. Instead, we observed differences in the daily patterns of physical activity. Day of the week might be an important target for personalization of physical activity interventions, with a relation between high depressive symptoms and low physical activity towards the end of the traditional working week. Future work should evaluate potential causes of alterations in day-to-day physical activity patterns in depression.
Declaration
Ethics, consent and permissions: The study protocol was approved by the University of California, San Francisco (UCSF) Committee on Human Research and the mPED Data and Safety Monitoring Board (DSMB). All participants provided written consent and gave consent to publication prior to study enrollment.
Availability of data and materials
Curated technical appendices, statistical code, and anonymized data supporting the conclusions of this article is available from the authors on request.
Author contributions
Dr. Fukuoka was the principal investgator of the mPED trial, designed and implemented the study, and collected the data. Dr. Figueroa drafted the first version of the manuscript and conducted the quantitative analysis. Dr. Vittinghoff was a principal biostatistician of the mPED trial and supervised the statistical analysis for this paper. Dr. Aguilera assisted with interpreting the results of the analyses. All authors contributed to the writing of the final manuscript.
Funding
The project described was supported by the Award Number R01HL104147 from the National Heart, Lung, and Blood Institute, by the American Heart Association, and by a grant (K24NR015812) from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2021.101325.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Penninx B.W. Depression and cardiovascular disease: epidemiological evidence on their linking mechanisms. Neurosci. Biobehav. Rev. 2017;74:277–286. doi: 10.1016/j.neubiorev.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Santos T., Martins J., Matos M.G.D., Valeiro M.G. The association between physical activity and chronic diseases in European adults AU – Marques, Adilson. Eur. J. Sport Sci. 2018;18(1):140–149. doi: 10.1080/17461391.2017.1400109. [DOI] [PubMed] [Google Scholar]
- Wyatt S.B., Winters K.P., Dubbert P.M. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Am. J. Med. Sci. 2006;331(4):166–174. doi: 10.1097/00000441-200604000-00002. [DOI] [PubMed] [Google Scholar]
- Williams E.P., Mesidor M., Winters K., Dubbert P.M., Wyatt S.B. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr. Obesity Rep. 2015;4(3):363–370. doi: 10.1007/s13679-015-0169-4. [DOI] [PubMed] [Google Scholar]
- Troiano R.P., Berrigan D., Dodd K.W., Masse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Kao M.-C.-J., Jarosz R., Goldin M., Patel A., Smuck M. Determinants of physical activity in America: a first characterization of physical activity profile using the National Health and Nutrition Examination Survey (NHANES) PM&R. 2014;6(10):882–892. doi: 10.1016/j.pmrj.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–158. doi: 10.1016/S2215-0366(16)30263-2. [DOI] [PubMed] [Google Scholar]
- Bennie J.A., De Cocker K., Teychenne M.J., Brown W.J., Biddle S.J.H. The epidemiology of aerobic physical activity and muscle-strengthening activity guideline adherence among 383,928 U.S. adults. Int. J. Behav. Nutr. Phys. Activity. 2019;16(1):34. doi: 10.1186/s12966-019-0797-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody, D.J., Pratt, L.A., Hughes, J.P., 2018. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. US Department of Health and Human Services, Centers for Disease Control and ….
- Al-Qahtani A.M., Shaikh M.A.K., Shaikh I.A. Exercise as a treatment modality for depression: a narrative review. Alexand. J. Med. 2018;54(4):429–435. [Google Scholar]
- Ströhle A. Physical activity, exercise, depression and anxiety disorders. J. Neural Transm. 2009;116(6):777. doi: 10.1007/s00702-008-0092-x. [DOI] [PubMed] [Google Scholar]
- Mammen G., Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am. J. Prev. Med. 2013;45(5):649–657. doi: 10.1016/j.amepre.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Harvey S.B., Øverland S., Hatch S.L., Wessely S., Mykletun A., Hotopf M. Exercise and the prevention of depression: results of the HUNT cohort study. Am. J. Psychiatry. 2017;175(1):28–36. doi: 10.1176/appi.ajp.2017.16111223. [DOI] [PubMed] [Google Scholar]
- Mata J., Thompson R.J., Jaeggi S.M., Buschkuehl M., Jonides J., Gotlib I.H. Walk on the bright side: physical activity and affect in major depressive disorder. J. Abnorm. Psychol. 2012;121(2):297. doi: 10.1037/a0023533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo A., Edney S., Plotnikoff R. Can smartphone apps increase physical activity? Systematic review and meta-analysis. J. Med. Internet Res. 2019;21(3) doi: 10.2196/12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray J.M., Brennan S.F., French D.P., Patterson C.C., Kee F., Hunter R.F. Effectiveness of physical activity interventions in achieving behaviour change maintenance in young and middle aged adults: A systematic review and meta-analysis. Soc. Sci. Med. 2017;192:125–133. doi: 10.1016/j.socscimed.2017.09.021. [DOI] [PubMed] [Google Scholar]
- Yerrakalva D., Yerrakalva D., Hajna S., Griffin S. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. J. Med. Internet Res. 2019;21(11) doi: 10.2196/14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Gorber S.C., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behavioral Nutrition Physical Activity. 2008;5(1):56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Haskell W., Vittinghoff E. New insights into discrepancies between self-reported and accelerometer-measured moderate to vigorous physical activity among women–the mPED trial. BMC Public Health. 2016;16(1):761. doi: 10.1186/s12889-016-3348-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J.B., Beets M.W., Morris S.F., Kolbe M.B. Day of the week is associated with meeting physical activity recommendations and engaging in excessive sedentary time in youth. J. Phys. Act Health. 2014;11(5):971–976. doi: 10.1123/jpah.2012-0190. [DOI] [PubMed] [Google Scholar]
- Davis M.G., Fox K.R., Hillsdon M., Sharp D.J., Coulson J.C., Thompson J.L. Objectively measured physical activity in a diverse sample of older urban UK adults. Med. Sci. Sports Exerc. 2011;43(4):647–654. doi: 10.1249/MSS.0b013e3181f36196. [DOI] [PubMed] [Google Scholar]
- Carr L.J., Dunsinger S., Marcus B.H. Long-term surveillance of physical activity habits of Latinas enrolled in a 12-month physical activity intervention. J. Phys. Activity Health. 2016;13(7):740–746. doi: 10.1123/jpah.2015-0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolai S., Benzinger P., Skelton D.A., Aminian K., Becker C., Lindemann U. Day-to-day variability of physical activity of older adults living in the community. J. Aging Phys. Activity. 2010;18(1):75–86. doi: 10.1123/japa.18.1.75. [DOI] [PubMed] [Google Scholar]
- Fukuoka Y., Komatsu J., Suarez L. The mPED randomized controlled clinical trial: applying mobile persuasive technologies to increase physical activity in sedentary women protocol. BMC Public Health. 2011;11(1):1–8. doi: 10.1186/1471-2458-11-933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Lindgren T.G., Mintz Y.D., Hooper J., Aswani A. Applying natural language processing to understand motivational profiles for maintaining physical activity after a mobile app and accelerometer-based intervention: the mPED randomized controlled trial. JMIR mHealth and uHealth. 2018;6(6) doi: 10.2196/10042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Haskell W., Lin F., Vittinghoff E. Short-and long-term effects of a mobile phone app in conjunction with brief in-person counseling on physical activity among physically inactive women: the mPED randomized clinical trial. JAMA Network Open. 2019;2(5) doi: 10.1001/jamanetworkopen.2019.4281. e194281–e194281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Lisha N.E., Vittinghoff E. Comparing asian american women's knowledge, self-efficacy, and perceived risk of heart attack to other racial and ethnic groups: the mPED trial. J. Women's Health. 2017;26(9):1012–1019. doi: 10.1089/jwh.2016.6156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindgren T., Hooper J., Fukuoka Y. Perceptions and experiences of women participating in a digital technology-based physical activity intervention (the mPED trial): qualitative study. JMIR Public Health Surveillance. 2019;5(4) doi: 10.2196/13570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Gay C., Haskell W., Arai S., Vittinghoff E. Identifying factors associated with dropout during prerandomization run-in period from an mHealth physical activity education study: the mPED trial. JMIR mHealth and uHealth. 2015;3(2) doi: 10.2196/mhealth.3928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M., Fukuoka Y., Goldberg K., Vittinghoff E., Aswani A. Applying machine learning to predict future adherence to physical activity programs. BMC Med. Inf. Decis. Making. 2019;19(1):169. doi: 10.1186/s12911-019-0890-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuoka Y., Zhou M., Vittinghoff E., Haskell W., Goldberg K., Aswani A. Objectively measured baseline physical activity patterns in women in the mPED trial: cluster analysis. JMIR Public Health Surveillance. 2018;4(1) doi: 10.2196/publichealth.9138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M.M., Sholomskas D., Pottenger M., Prusoff B.A., Locke B.Z. Assessing depressive symptoms in five psychiatric populations: a validation study. Am. J. Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Ainsworth B.E., Haskell W.L., Leon A.S. Compendium of physical activities: classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- O’Brien M.W., Kivell M.J., Wojcik W.R., d’Entremont G., Kimmerly D.S., Fowles J.R. Step rate thresholds associated with moderate and vigorous physical activity in adults. Int. J. Environ. Res. Public Health. 2018;15(11):2454. doi: 10.3390/ijerph15112454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C., Ham S.A., Macera C.A. Descriptive epidemiology of pedometer-determined physical activity. Med. Sci. Sports Exerc. 2004;36(9):1567–1573. doi: 10.1249/01.mss.0000139806.53824.2e. [DOI] [PubMed] [Google Scholar]
- Strine T.W., Chapman D.P., Balluz L., Mokdad A.H. Health-related quality of life and health behaviors by social and emotional support. Soc. Psychiatry Psychiatr. Epidemiol. 2008;43(2):151–159. doi: 10.1007/s00127-007-0277-x. [DOI] [PubMed] [Google Scholar]
- Ludwig V.M., Bayley A., Cook D.G. Association between depressive symptoms and objectively measured daily step count in individuals at high risk of cardiovascular disease in South London, UK: a cross-sectional study. BMJ Open. 2018;8(4) doi: 10.1136/bmjopen-2017-020942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr D.J., Levy R., Scheepers C., Tily H.J. Random effects structure for confirmatory hypothesis testing: Keep it maximal. J. Mem. Lang. 2013;68(3) doi: 10.1016/j.jml.2012.1011.1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek E.V., Phatak S.S., Martin C.A. Adaptive step goals and rewards: a longitudinal growth model of daily steps for a smartphone-based walking intervention. J. Behav. Med. 2018;41(1):74–86. doi: 10.1007/s10865-017-9878-3. [DOI] [PubMed] [Google Scholar]
- Pinheiro, J., Bates, D., DebRoy, S., et al., 2017. Package ‘nlme’. Linear and nonlinear mixed effects models, version. 2017.
- Lüdecke D. ggeffects: Tidy data frames of marginal effects from regression models. J. Open Source Software. 2018;3(26):772. [Google Scholar]
- Ku P.W., Steptoe A., Liao Y., Sun W.J., Chen L.J. Prospective relationship between objectively measured light physical activity and depressive symptoms in later life. Int. J. Geriatric Psychiatry. 2018;33(1):58–65. doi: 10.1002/gps.4672. [DOI] [PubMed] [Google Scholar]
- Schuch F., Vancampfort D., Firth J. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J. Affect. Disord. 2017;210:139–150. doi: 10.1016/j.jad.2016.10.050. [DOI] [PubMed] [Google Scholar]
- Whitaker K.M., Sharpe P.A., Wilcox S., Hutto B.E. Depressive symptoms are associated with dietary intake but not physical activity among overweight and obese women from disadvantaged neighborhoods. Nutr. Res. 2014;34(4):294–301. doi: 10.1016/j.nutres.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White R.L., Babic M.J., Parker P.D., Lubans D.R., Astell-Burt T., Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am. J. Prev. Med. 2017;52(5):653–666. doi: 10.1016/j.amepre.2016.12.008. [DOI] [PubMed] [Google Scholar]
- Kleppang A.L., Hartz I., Thurston M., Hagquist C. The association between physical activity and symptoms of depression in different contexts–a cross-sectional study of Norwegian adolescents. BMC Public Health. 2018;18(1):1368. doi: 10.1186/s12889-018-6257-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianfredi V., Blandi L., Cacitti S. Depression and objectively measured physical activity: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health. 2020;17(10):3738. doi: 10.3390/ijerph17103738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Uffelen J.G., Khan A., Burton N.W. Gender differences in physical activity motivators and context preferences: a population-based study in people in their sixties. BMC Public Health. 2017;17(1):624. doi: 10.1186/s12889-017-4540-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard T.M., Wagnild J.M. Gender differences in walking (for leisure, transport and in total) across adult life: a systematic review. BMC Public Health. 2017;17(1):1–11. doi: 10.1186/s12889-017-4253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty A., Jackson D., Hammerla N. Large scale population assessment of physical activity using wrist worn accelerometers: The UK Biobank Study. PLoS ONE. 2017;12(2) doi: 10.1371/journal.pone.0169649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triantafyllidis A.K., Tsanas A. Applications of machine learning in real-life digital health interventions: review of the literature. J. Med. Internet Res. 2019;21(4) doi: 10.2196/12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M., Fukuoka Y., Mintz Y. Evaluating machine learning–based automated personalized daily step goals delivered through a mobile phone app: Randomized controlled trial. JMIR mHealth and uHealth. 2018;6(1) doi: 10.2196/mhealth.9117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Richards J., Rosenbaum S., Ward P.B., Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J. Psychiatr. Res. 2016;77:42–51. doi: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- Chalder M., Wiles N.J., Campbell J. Facilitated physical activity as a treatment for depressed adults: randomised controlled trial. BMJ: Br. Med. J. 2012;344 doi: 10.1136/bmj.e2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogh J., Nordentoft M., Sterne J., Lawlor D.A. Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet] Centre for Reviews and Dissemination (UK); 2011. The effect of exercise in clinically depressed adults: systematic review and meta-analysis of randomized controlled trials. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.