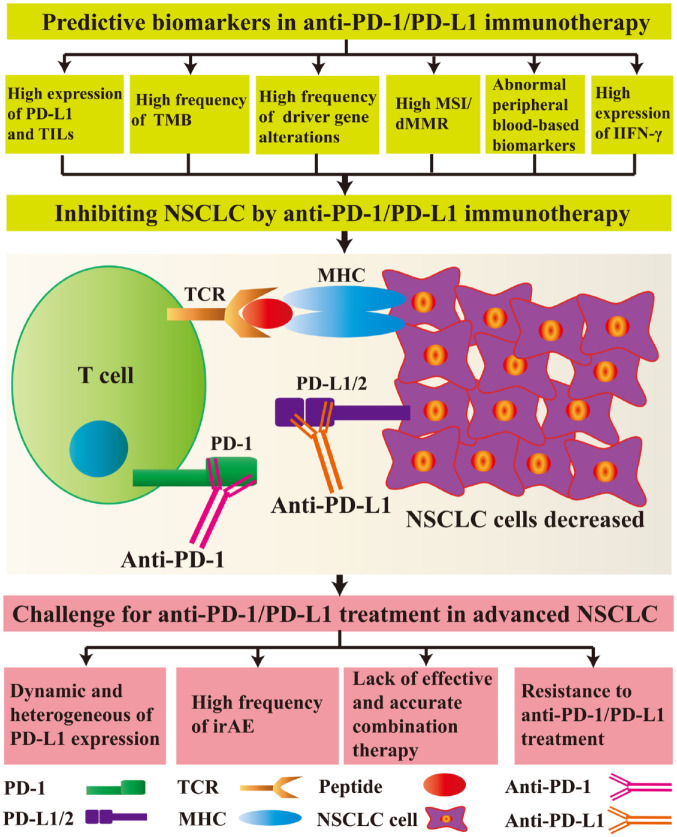
Figure 2.
Predictive biomarkers and challenges facing anti-programmed cell-death protein 1 (PD-1)/programmed cell-death ligand 1 (PD-L1) treatment in advanced non-small-cell lung cancer (NSCLC).
For inhibiting NSCLC cells, the predictive biomarkers include high expression levels of PD-L1, high numbers of tumour infiltrating lymphocytes (TILs), high tumour mutational burden (TMB), a high frequency of driver-gene alterations, high microsatellite instability (MSI)/defective mismatch repair (dMMR), abnormal peripheral blood-based biomarkers, and high expression levels of interferon gamma (IFN-γ). After administration of anti-PD-1 or anti-PD-L1 antibodies, the interaction between PD-1 and PD-L1/L2 is disrupted, inhibiting cell signalling pathways. T cells and other immune-related cells exert anti-tumour effects; however, there are still many unresolved problems in the clinical use of anti-PD-1/PD-L1 therapies, such as dynamic changes and heterogeneous differences in PD-L1 expression, a high frequency of immune-related adverse events (irAEs), the lack of effective and accurate combination therapies, and resistance to anti-PD-1/PD-L1 treatment.
MHC, major histocompatibility complex; TCR, T cell receptor.