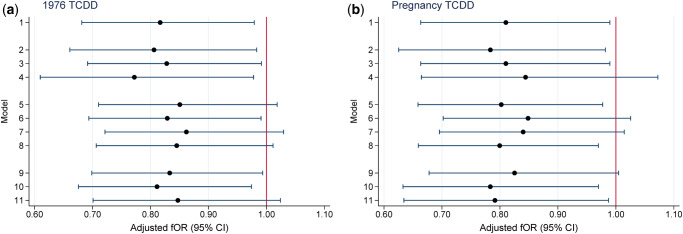
Figure 1.
Sensitivity analyses for the relationship between TCDD exposure (log10) and time to pregnancy, Seveso Women’s Health Study, Seveso, Italy, 1976–2016. The fOR can be viewed as the change in the odds of conceiving in a given cycle associated with a 10-fold increase in TCDD concentration. (a) fOR for TCDD in 1976 and (b) fOR for TCDD at pregnancy. Models adjusted for maternal age at trying, smoking in previous year, oral contraceptive use in previous year, pre-explosion parity, irregular menstrual cycle, history of reproductive or endocrine conditions and paternal age. Key to y-axis numbers: primary analysis (Model 1) 1. Live births not due to contraceptive failure (n = 446); alternate subsets (Models 2–4). 2. Exclude women whose first pregnancy did not result in a live birth (n = 371). 3. Include women who attempted for ≥12 months who never conceived (n = 464). 4. Exclude women who conceived in the first cycle (n = 287). Include pregnancies resulting from contraceptive failure (Models 5–8). 5. Add 78 pregnancies after reported regular contraceptive use (TTP = 0) (n = 524). 6. Add 36 pregnancies after reported irregular contraceptive use (TTP = duration of irregular use/2) (n = 482). 7. Add 114 pregnancies after reported regular (TTP = 0) or irregular (TTP = duration of irregular use/2) contraceptive use (n = 560). 8. Add 114 pregnancies after reported regular or irregular contraceptive use (TTP = 0) (n = 560). Change censoring window from 12 months for TTP (Models 9–11). 9. Censor at 14 months (n = 446). 10. Censor at 10 months (n = 446). 11. Censor at 7 months (n = 446). fOR, fecundability odds ratio; TCDD, 2,3,7,8-tetrachlorodibenzo-p-dioxin; TTP, time to pregnancy.