Figure 1.
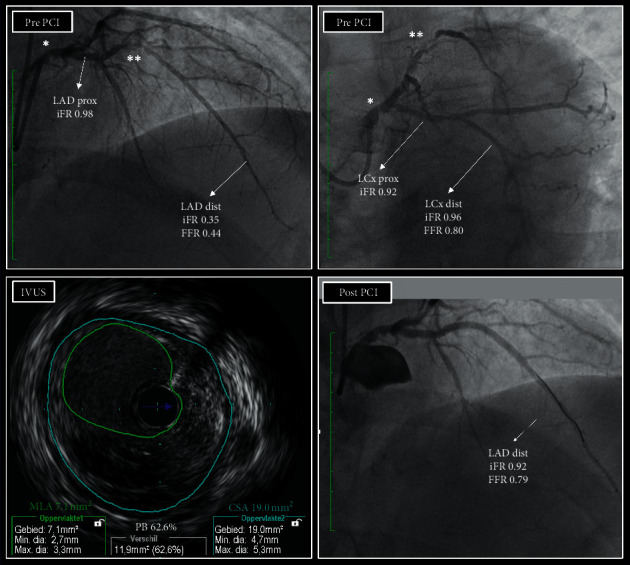
A practical example of a LM lesion with downstream disease. A patient with effort angina had a LM lesion (∗) which appeared angiographically at least moderate, but also a severe lesion at the level of the mid LAD (∗∗). The LCx showed some disease but was clearly the least affected daughter branch of the LM. iFR distal to LAD was 0.35, indicating flow-limiting disease upstream, but assessment of the iFR along the course of the LAD revealed that the drop in iFR was mainly caused by the mid LAD lesion. In the proximal part of the LAD, the iFR was 0.92, suggesting that the LM lesion was not physiologically significant. iFR in the LCx was 0.92 in the proximal part and 0.96 in the distal part, which seemed to confirm this. However, since the disease in the LAD was so severe that it may also have been flow-limiting at rest, stable resting conditions may have been absent and, theoretically, the iFR might have been lower at that level if the downstream disease was not so critical. FFR towards LAD was 0.44, also indicating critical disease upstream. FFR towards LCx was 0.80, borderline significant. Since the disease in LAD was severe and the value was below 0.85, the LM lesion might still have been flow-limiting. Given the iFR and FFR findings, the operators decided to also evaluate the LM lesion with IVUS. The MLA was 7.1 mm2 (above 6.0 mm2), and the operators decided to defer the LM, treat the LAD lesion, and repeat physiological assessment. After PCI, the result was good by IVUS, and the iFR was 0.92. FFR was 0.79, just below 0.80 but above 0.75. Maximal preventive treatment was installed and, 20 months later, the patient is still asymptomatic and event free. Because of the disease in the LM (plaque burden, PB, on IVUS was 62%) and the final FFR value, the operators did plan a follow-up angiography with physiological assessment and IVUS 2 years after the index procedure. LM: left main; LAD: left anterior descending artery; LCx: left circumflex artery; iFR: instantaneous wave-free ratio; FFR: fractional flow reserve; IVUS: intravascular ultrasound; MLA: minimal lumen area; CSA: external elastic membrane cross sectional area; PB: plaque burden; PCI: percutaneous coronary intervention. Of note, the higher iFR value in the distal LCx versus in the proximal LCx can be explained by the fact that the distal part of the LCx is located significantly lower than the aortic root and thus exposed to a higher hydrostatic pressure.
