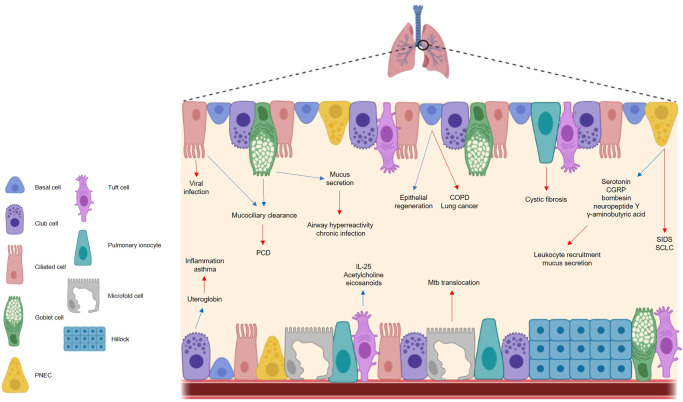
Fig. 1. The respiratory epithelium is important in maintaining respiratory homeostasis but can become implicated in disease.
The cells of the airway epithelium each play a functionally distinct role in health and disease. In a healthy state (blue arrows), basal cells are the principal stem cells of the airway, facilitating epithelial regeneration. Club cells secrete the anti-inflammatory protein uteroglobin, and ciliated cells ensure effective mucociliary clearance in conjunction with goblet cells, the chief mucus producing cells of the airways. Pulmonary neuroendocrine cells secrete a range of neuropeptides, while tuft cells are thought to secrete IL-25, acetylcholine and eicosanoids, although the exact role of these molecules in a respiratory context is unclear. In a diseased state (red arrows), cells of the respiratory epithelium contribute to different illnesses. Basal cells have been linked to COPD and lung cancer, while uteroglobin deficiencies are seen in asthma sufferers. Ciliated cells are the target of viral infection and impaired cilia functionality can cause issues with mucociliary clearance e.g. PCD. Aberrations in mucus production can cause respiratory complications including chronic infection. Neuropeptides induce mucus secretion and leukocyte recruitment and contribute to the pathogenesis of SIDS and SCLC, and microfold cells facilitate Mtb translocation. The mechanisms by which pulmonary ionocytes contribute to cystic fibrosis are largely unknown, and the impact of tuft cells on respiratory disease are poorly characterized. PNEC pulmonary neuroendocrine cell, PCD primary ciliary dyskinesias, CGRP calcitonin gene-related peptide; SIDS sudden infant death syndrome, SCLC small cell lung carcinoma, Mtb mycobacterium tuberculosis, COPD chronic obstructive pulmonary disease.