Abstract
Family-centered care (FCC) has become the normative practice in Neonatal ICUs across North America. Over the past 25 years, it has grown to impact clinician-parent collaborations broadly within children’s hospitals as well as in the NICU and shaped their very culture. In the current COVID-19 pandemic, the gains made over the past decades have been challenged by “visitor” policies that have been implemented, making it difficult in many instances for more than one parent to be present and truly incorporated as members of their baby’s team. Difficult access, interrupted bonding, and confusing messaging and information about what to expect for their newborn can still cause them stress. Similarly, NICU staff have experienced moral distress. In this perspective piece, we review those characteristics of FCC that have been disrupted or lost, and the many facets of rebuilding that are presently required.
Subject terms: Quality of life, Medical ethics
After the seminal publication of “The principles for family-centered neonatal care” in Pediatrics in 1993 [1], a large wave of interest developed in doing better by babies and families in the neonatal intensive care units (NICUs) across North America. This interest was not only by parents, parent and patient advocates, and non-professionals in and out of healthcare, but by interdisciplinary clinicians as well. Psychologists, nurses, neonatologists, and pediatricians all began to study and implement means by which care could be more patient and family-centered in its development and delivery [2, 3]. Observations were made of how pediatric resident experiences might improve in the NICU [4] and even how parents of newborns on extreme life-support measures like ECMO (extra-corporeal membrane oxygenation) could add to the conversations [5].
In time, as NICUs across North America aged and new NICUs were being planned and built, the very design of the physical spaces in the NICU accommodated family presence and engagement better than any time in history [6, 7]. FCC became the norm, the expectation, and the focus of many clinician-parent collaborations broadly within children’s hospitals as well as in the NICU. Adult hospitals mirrored the work done first in pediatric centers [8]. Now, there is additional importance of parental involvement in the NICU, underscored by a consideration of renaming the NICU to the neonatal intensive parenting unit, to highlight the involvement of the family and emphasize the necessity of bonding and attachment between the parents and the newborn [9].
Then came a pandemic, or two. In 2003, there were restrictions placed on family presence at the bedside of their loved one during the SARS-1 pandemic [10]. At that time, issues of social isolation—felt by patients, parents, and clinicians—were described in situations where concerns for infection control prevailed over facilitating FCC. These same situations brought with them considerable emotions that challenged and even changed professional and parental roles. Communication was difficult. And investigators noted that “…effective clinical approaches…” should be developed “…in the event of future outbreaks…” [10]. The H1N1 pandemic of 2009 was such an anticipated event, but it did not substantively materialize in North America.
Now, in 2021, we contend with COVID-19, the ongoing pandemic illness caused by the SARS-CoV2 virus. Almost overnight, units of care in pediatric and adult hospitals closed to family and visitors in the spring of 2020. While families may not have become “visitors” in the strictest sense, a general perception by many NICU staff and parents has been that even parents of critically ill or preterm newborns, were subjected to “visitor policies”. This occurred for all stages of care—on admission, while on critical life-supporting technologies, and even when dying. While NICUs and children’s hospitals have not been overwhelmed with neonatal and pediatric cases of COVID-19, the staff have nonetheless had to struggle with several moral and ethical issues [11].
Clinical staff in NICUs are distraught, disillusioned, and have been experiencing moral distress. Given a quarter century history of developing and knowing what “was right”, and what has been enculturated in the NICU and across children’s hospitals, they can see how current constraints by infection control and “visitation” policies that have been promoted in efforts to mitigate, if not absolutely prevent, infection among NICU staff or patients keep them from providing the care they believe is best for babies and families in both the short and the long-term. While speaking from an adult hospital perspective, Morley et al. relate a number of contributors to moral distress among staff at this time including a lack of personal protective equipment (PPE), visitation restrictions, impaired communication, and relational capacity between staff and patients/families, risks to their own personal and family safety, contending with scarce resource allocation, and some reduction in the overall level of care provided amidst the pandemic [12]. Virani et al. utilize three pediatric cases (one being a newborn) to elicit responses from a diverse group of pediatric clinicians and ethicists [13]. Haward enjoins other neonatology and ethics colleagues in describing not only the moral, ethical and emotional toll that this pandemic and healthcare organizations’ responses have taken on vulnerable patients, their families, and staff, but offer different suggestions to guide leadership in ways forward [14].
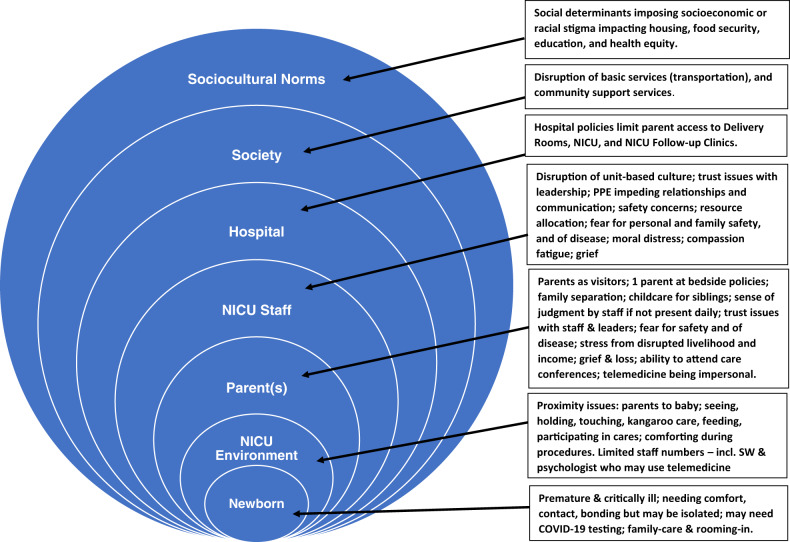
Borrowing from a model used by Raman et al. in their report on a child rights-based response to COVID-19 [15], the following figure is offered to help us organize our thoughts around pertinent clinical, environmental, ethical, and sociocultural responses to challenges brought forth by the pandemic as we attempt to regain what has been lost in FCC care these past few months [Fig. 1].
Fig. 1.
Family-centered care determinants in COVID-19 times.
As the pandemic continues, there will be vacillations in efforts to contain the spread of infection and mitigate disease largely based upon epidemiologic data within geographic regions, states, and cities. This will involve ongoing surveillance, testing, rigorous hygienic practices, the wearing of masks, social distancing, concerted efforts within hospitals to wear and utilize PPE and isolate infected patients. Hospitals, and individual units of care within them such as the NICU, will need to strike a balance between the increasingly understood risks of spread and the less clear but nonetheless important risks that minimal contact of newborns with their parents will have on both infant adaptation, bonding and development, and parental growth and development. [Textbox].
Box.
Textbox.
|
(1) Advocating for community parental support. (2) Provision of transportation and other community support services. (3) Hospital and NICU policy exceptions, likely on a case-by-case basis. (4) Transparency in leadership and managing change. (5) Provision of PPE and other staff and family safety and protection methods. (6) Education for parents about COVID-19 and pregnancy, childbirth, neonatal management, and outcomes. (7) Addressing moral distress. (8) Staff morale support, critical incident debriefs (e.g., after neonatal deaths), and stress counseling. (9) Resource provisions in a just and equitable manner. (10) Staffing that makes clear to parents that their baby is safe. (11) Using telemedicine in an effective and equitable manner. (12) Special end-of-life considerations. (13) Family grief and stress counseling and support. (14) Allowing parental contact with their newborn as much as possible. (15) Trauma-informed care touchpoints to remind staff of the experience of patients and families and how it connects to their experience of the NICU, therefore their behavior. (16) Diversity of thought and discipline in decisions involving changes in family engagement with their baby (i.e., visitor restrictions etc.). (17) Involvement of parents and bedside staff representatives in policy development and implementation. Targeted efforts to regain what aspects of FCC may have been lost in the pandemic. |
FCC is a valuable philosophy and practice to keep in the forefront of leadership, management, and clinician’s minds, especially in the high-stress and intense setting of the NICU. Given the numerous societal stressors our nation is currently undergoing, this is truer now than ever before. For various reasons families, NICU staff, and even babies are overwhelmed. Despite COVID-19, the principles of FCC, established in 1993, are still important to carry out in 2021. Families need their babies and babies need their families, and it is the responsibility of hospital systems to ensure this can continue to be supported in the safest manner possible. To do this, we must continue to consider the many clinical, environmental, ethical, and sociocultural determinants that impact care and affect the family unit.
Author contributions
BC conceived the idea and wrote the first draft. TW and AK edited and revised the first draft and both the Figure and the Textbox. All authors contributed to and approved the final version of the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harrison H. The principles for family-centered neonatal care. Pediatrics. 1993;92:643–50. [PubMed] [Google Scholar]
- 2.Als H, Gilkerson L. The role of relationship-based developmentally supportive newborn intensive care in strengthening outcomes of preterm infants. Semin Perinatol. 1997;21:178–89. doi: 10.1016/S0146-0005(97)80062-6. [DOI] [PubMed] [Google Scholar]
- 3.Bracht M, Kandankery A, Nodwell S, Stade B. Cultural differences and parental responses to the preterm infant at risk: Strategies for supporting families. Neonat Netw. 2002;21:31–38. doi: 10.1891/0730-0832.21.6.31. [DOI] [PubMed] [Google Scholar]
- 4.Clark PA. What residents are not learning: Observations in a NICU. Acad Med. 2001;76:419–24. doi: 10.1097/00001888-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Curley MA, Meyer EC. Parental experience of highly technical therapy: Survivors and non-survivors of extracorporeal membrane oxygenation support. Pediatr Crit Care Med. 2003;4:214–9. doi: 10.1097/01.PCC.0000043915.79848.8D. [DOI] [PubMed] [Google Scholar]
- 6.White RD, Smith JA, Shepley MM. Recommended standards for newborn ICU design. J Perinatol. 2013;33:S2–16. doi: 10.1038/jp.2013.10. [DOI] [PubMed] [Google Scholar]
- 7.White RD. The next big ideas in NICU design. J Perinatol. 2016;36:259–62. doi: 10.1038/jp.2016.6. [DOI] [PubMed] [Google Scholar]
- 8.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–28. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 9.Hall SL, Hynan MT, Phillips R, Craig JW, Goyer E, Hatfield RF, et al. The neonatal intensive parenting unit: an introduction. J Perinatol. 2017;37:1257–64. doi: 10.1038/jp.2017.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koller DF, Nicholas DB, Goldie RS, Gearing R, Selkirk EK. When family-centered care is challenged by infectious disease: pediatric health care delivery during the SARS outbreaks. Qual Health Res. 2006;16:47–60. doi: 10.1177/1049732305284010. [DOI] [PubMed] [Google Scholar]
- 11.Arnaez J, Montes MT, Herranz-Rubia N, Garcia-Alix A. The impact of the current SARS-CoV-2 pandemic on neonatal care. Front Pediatr. 2020;8:247. doi: 10.3389/fped.2020.00247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morley G, Sese D, Rajendram P, Horsburgh CC. Addressing caregiver moral distress during the COVID-19 pandemic. Cleveland Clin J Med. 2020. 10.3949/ccjm.87a.ccc047. [DOI] [PubMed]
- 13.Virani AK, Puls HT, Mitsos R, Longstaff H, Goldman RD, Lantos JD. Benefits and risks of visitor restrictions for hospitalized children during the COVID pandemic. Pediatrics. 2020;146:e2020000786. doi: 10.1542/peds.2020-000786. [DOI] [PubMed] [Google Scholar]
- 14.Haward MF, Moore GP, Lantos J, Janvier A. Paediatric ethical issues during the COVID-19 pandemic are not just about ventilator triage. Acta Paediatr. 2020:1–3. 10.1111/apa.15334. [DOI] [PMC free article] [PubMed]
- 15.Raman S, Harries M, Nathawad R, Kyeremateng R, Seth R, Lonne B, et al. Where do we go from here? A child rights-based response to COVID-19. BMJ Paediatr Open. 2020;4:e000714. doi: 10.1136/bmjpo-2020-000714. [DOI] [PMC free article] [PubMed] [Google Scholar]