Abstract
Objective
To describe the adaptations made to implement virtual cancer rehabilitation at the onset of the coronavirus disease 2019 pandemic, as well as understand the experiences of patients and providers adapting to virtual care.
Design
Multimethod study.
Setting
Cancer center.
Participants
A total of 1968 virtual patient visits were completed during the study period. Adult survivors of cancer (n=12) and oncology health care providers (n=12) participated in semi-structured interviews.
Interventions
Not applicable.
Main Outcome Measures
Framework-driven categorization of program modifications, qualitative interviews with patients and providers, and a comparison of process outcomes with the previous 90 days of in-person care via referrals, completed visits and attendance, method of delivery, weekly capacities, and wait times.
Results
The majority of program visits could be adapted to virtual delivery, with format, setting, and content modifications. Virtual care demonstrated an increase or maintenance in the number of completed visits by appointment type compared with in-person care, with attendance ranging from 80%-93%. For most appointment types, capacities increased, whereas wait times decreased slightly. Overall, 168 patients (11% of all assessments and follow-ups) assessed virtually were identified by providers as requiring an in-person appointment because of reassessment of musculoskeletal and/or neurologic impairment (n=109, 65%) and lymphedema (n=59, 35%). The interviews (n=24) revealed that virtual care was an acceptable alternative in some circumstances, with the ability to (1) increase access to care; (2) provide a sense of reassurance during a time of isolation; and (3) provide confidence in learning skills to self-manage impairments.
Conclusions
Many appointments can be successfully adapted to virtual formats to deliver cancer rehabilitation programming. Based on our findings, we provide practical recommendations that can be implemented by providers and programs to facilitate the adoption and delivery of virtual care.
Keywords: Cancer survivors, COVID-19, Neoplasms, Rehabilitation, Survivorship, Telemedicine
List of abbreviations: CaRE, Cancer Rehabilitation and Exercise program; COVID-19, coronavirus disease 2019; CRS, Cancer Rehabilitation and Survivorship Program; FRAME, Framework for Reporting Adaptations and Modifications-Expanded; HCP, health care provider; OT, occupation therapy; OTN, Ontario Telemedicine Network; PT, physiotherapy
Cancer rehabilitation is an essential component of survivorship care and has become increasingly relevant with a growing survivors of cancer cohort and high documented rates of impairment and disability.1 , 2 The coronavirus disease 2019 (COVID-19) pandemic has required a rapid transition from in-person rehabilitation to virtual care through telephone- or video-based visits.3 However, this shift has largely been made with little evidence on best practices.
Virtual care may improve access for geographically dispersed patients and reduce physical, financial, and logistical barriers to in-person care.4 Telehealth interventions have also shown promise in addressing physical and psychosocial concerns among survivors of cancer.5 , 6 Notwithstanding these potential benefits, regulatory restrictions surrounding reimbursement, licensing, and hospital credentialing, as well as patient and provider attitudes have impeded its broader adoption.7 , 8 Additionally, differential access to telecommunication technologies based on social and geographic factors can pose a challenge to its implementation.8
As a result of the evolving COVID-19 crisis, the Princess Margaret Cancer Centre proactively suspended all nonessential in-person appointments. Therefore, the Cancer Rehabilitation and Survivorship Program (CRS) abruptly shifted services to be delivered virtually as of March 16, 2020. Despite recent recommendations for virtual care during the pandemic,3 , 9 , 10 research on virtual cancer rehabilitation is limited. Given the uncertainty for when a return to previous levels of in-person care will occur, the current demand and surge in virtual care use presents a unique opportunity to examine the implementation of virtual cancer rehabilitation and provide strategies on how to adapt in-person care to deliver a sustainable virtual care model. The purpose of this study was to (1) describe the adaptations made to deliver virtual cancer rehabilitation during the first 90 days of the COVID-19 pandemic and (2) understand the experiences of patients and health care providers (HCPs) receiving and delivering virtual care.
Methods
We used a multimethod approach to describe the adaptations to the CRS during the first 90 days of the COVID-19 pandemic (March 16-June 12, 2020). This study was informed by the Framework for Reporting Adaptations and Modifications-Expanded (FRAME), a comprehensive framework used to support research on the nature, reasons for, and effect of modifications to interventions.11 This project was assessed by the Research Ethics Board at the institution and was issued a formal waiver exempting the study of the requirement for Research Ethics Board approval.
Description of the CRS
The CRS at the Princess Margaret Cancer Centre is a consultative impairment-driven program that includes a multidisciplinary rehabilitation team including physical medicine and rehabilitation, occupational therapy (OT), physiotherapy (PT), kinesiology, massage therapy, neuropsychology, social work, and dietetics. Patients with an identified impairment are referred to the CRS clinic by their oncology HCP and are seen by a team composed of a physiatrist and physiotherapist or occupational therapist who complete a comprehensive cancer rehabilitation assessment. A personalized care plan is developed based on their identified impairment(s), level of disability, and personal goals. Care within our program may include further 1-on-1 appointments with a member of our team (eg, occupational therapist, neuropsychologist, social worker) and/or group education (eg, return to work, lymphedema, brain fog). Patients can also be referred to the Cancer Rehabilitation and Exercise (CaRE) program, an 8-week program consisting of exercise and self-management skills education delivered in person in a group format (CaRE@ELLICSR) or a home-based model (CaRE@Home). The CaRE@Home program includes weekly on-line modules, a mobile application and wearable device to support exercise, and weekly health coaching calls to promote behavior change.12
Adaptations and modifications to the CRS
The FRAME was used to guide the documentation of the adaptations made to the CRS and included the following: (1) when during the implementation process the modifications were made; (2) whether the modifications were planned or unplanned and proactive or reactive; (3) the individuals involved in the decision to modify program elements; and (4) the nature of context (eg, format, setting) and content modifications (eg, tailored, substituted, removed elements).11 Information on program adaptations were collected through documents completed by clinical team leads outlining instructions and plans for virtual care.
Capture of changes to CRS process outcomes
We collected data on process measures including (1) referrals; (2) completed visits and attendance; (3) method of appointment (ie, video, phone); (4) weekly appointment capacities; and (5) wait times. These outcomes were compared with the previous 3 months. Patients could be placed on a waiting list to be seen by our team in-person once services resumed or brought in if their condition was deemed serious. These appointments included comprehensive assessments, 1-on-1 appointments, and CaRE initial or follow-up assessments. The number of patients wait-listed and reasons for requiring an in-person visit were documented.
Experience with virtual care
We conducted semistructured interviews via telephone with CRS HCPs and patients who had received care virtually during the study period. We applied a pragmatic approach to recruitment and aimed to recruit 10 HCPs and 10 patients for interviews because of our narrow research question.13 However, data were collected until saturation was reached, meaning there were little or no changes to the codes from new interviews. Interviews were completed by 2 members of our team with experience with qualitative interviewing (C.L., B.E.). HCP interviews were informed by the FRAME and explored experiences with adapting to virtual care (supplemental appendix S1, available online only at http://www.archives-pmr.org/). We purposively sampled patients based on the type of CRS virtual visit they were attending (ie, comprehensive assessments, follow-up assessments, CaRE assessments), and interviews explored their perspectives with virtual care (supplemental appendix S2, available online only at http://www.archives-pmr.org/). Patients were also asked to complete a demographic questionnaire.
Data analysis
Context and content modifications were qualitatively synthesized based on the FRAME.14 Descriptive statistics were used to summarize process outcomes of the CRS during the 90 days before and after adapting to virtual care. Patient and HCP interviews were analyzed separately, and emerging themes were subsequently aligned to develop a cohesive understanding of experiences with virtual care. We followed a 6-step approach for thematic analysis.15 Interviews were digitally recorded and transcribed verbatim, and each transcript underwent a process of open coding by a member of the team (C.L.). The generated themes were reviewed in relation to the coded data and the entire data set and underwent further review by another interviewer (B.E.) to ensure they reflected the interviews conducted. These themes were refined, and representative quotes were chosen for each theme. Several strategies were used to ensure trustworthiness, including the appropriateness of the interview sample, the relevance of interview questions, and the steps taken to ensure the accuracy of the interview transcripts and generated themes.16
Results
Adaptations and modifications
All adaptations to the CRS were reactive to the COVID-19 crisis and planned over the course of 1 week prior to the suspension of all nonessential in-person visits. The adaptations were planned collaboratively and involved the CRS program director, program manager, and clinical team leads who shared this information with all clinical and administrative staff in team meetings to answer questions and obtain feedback from staff.
A summary of the context and content modifications for the delivery of virtual care is presented in table 1 . All in-person visits were rescheduled and delivered by telephone or through the Ontario Telemedicine Network (OTN), a secure 2-way videoconferencing telehealth platform. OTN is an independent, not-for-profit organization that partners with the provincial government to provide publicly funded virtual care. Patients receive an automated email detailing the date and time of the visit along with a link to access the appointment. HCPs were trained on how to use OTN, and patients were able to choose between conducting their appointments through either delivery method. Previously developed programs and resources (eg, CaRE@Home, education modules) facilitated adaptation to virtual care and mitigated the extent to which program elements were removed. No changes were made to the scheduled duration of appointments.
Table 1.
Adaptations to the cancer rehabilitation and survivorship program
| Appointment Type | Usual Care | Context and Content Modifications |
|---|---|---|
| Comprehensive assessments | Format: appointment includes an initial screen with an OT or PT, followed by an assessment with a MD (physiatrist). Setting: patients are seen in person. Content: patients complete electronic questionnaires in person, and moderate to high distress scores are flagged on a clinician report for the oncology team to assess. Assessments are guided by objective measures including a surveillance physical examination. Appointments include a comprehensive rehabilitation assessment and care plan based on a patient’s identified impairment, level of disability, and personal goals. Appointments are booked for a total of 1.5 h. |
Format: no change. Setting: adapted to video or phone. Tailored elements: (1) questions within standard distress screening questionnaires could be used as probes to guide the assessment, but summary reports were not available because a remote system had not been implemented within the cancer center; (2) physical tests and assessments were demonstrated and described to allow patients to complete them on their own; and (3) objective measures of function were not completed. Pacing/timing: no change was made to the scheduled appointment duration. |
| CaRE@Home | Patients are referred to the CaRE@Home program based on their comprehensive assessment. Format: initial 1-on-1 visit with an RKin, and follow-up visits at 8 wk and 3 and 6 mo. Setting: all assessments are conducted in person. Weekly counseling is delivered via phone. Content: in-person visits include a fitness assessment (6-min walk test, hand grip dynamometry, body composition, balance) and distress reports via questionnaires completed in person. Patients are supported with exercise Therabands, e-modules for education, a mobile application and wearable technology, and weekly brief telephone counseling. Assessments are booked for 1.5 h and weekly counseling is scheduled for 20 min. |
No change to the referral process. Format: no change. Setting: all assessments were switched to phone or video. Weekly counseling could now be delivered over video. Removed elements: (1) fitness assessment (6-min walk test, hand-drip dynamometry, body composition, 30-s balance); (2) provision of exercise Therabands; and (3) provision of wearable technology. Tailored elements: (1) exercises were demonstrated and described by the RKin over video, over phone, or through online instructional videos and (2) patient-reported outcomes were completed online at assessment timepoints, but summary reports were not available. Pacing/timing: no change was made to the scheduled appointment duration. |
| CaRE@ELLICSR | Patients are referred to the CaRE@ELLICSR program based on their comprehensive assessment. Format: initial 1-on-1 visit with an RKin, weekly group classes for 8 wk, and 1-on-1 follow-up visits with an RKin at 8 wk and 3 and 6 mo. Setting: all visits and classes are conducted in person. Content: patients receive an initial assessment and exercise prescription. Assessments include objective measures and distress reports via questionnaires completed in person. Group classes consist of supervised exercise and skills management education. Patients are supported with exercise Therabands, a mobile application, and wearable technology to track activity. Assessments are booked for 1.5 h. Weekly exercise and education classes are 60 min each. |
Patients currently enrolled in the CaRE@ELLICSR program were switched to CaRE@Home. All future groups were suspended. Format: weekly supervised group exercise classes were modified to individual weekly 1-on-1 telephone or video calls with an RKin for the remaining weeks of the program. Group skills management education was modified to individual online education. Setting: in-person assessments were adapted to video or phone. Education content was delivered via e-modules. Removed elements: (1) fitness assessment (6-min walk test, hand-drip dynamometry, body composition, 30-s balance). Pacing/timing: no changes were made to the scheduled duration of assessments. |
| OT and PT follow-up | Format: a 1-on-1 visit with an OT or PT. Setting: primarily in-person; however, OT consults could be delivered via phone. Content: assessments are guided by distress reports via questionnaires completed in clinic prior to the appointment and objective measures (eg, hand grip dynamometry, sit to stand, range of motion). Appointments are booked for 45 min. |
Format: no change. Setting: all appointments were delivered via phone or video. Tailored elements: (1) questions within standard distress screening questionnaires could be used as probes to guide the assessment, but reports were not available and (2) physical tests and assessments were demonstrated and described to allow patients to complete them on their own. Removed elements: objective measures of strength and function. Pacing/timing: no change was made to the scheduled appointment duration. |
| Manual lymphatic drainage | Format: a 1-on-1 visit with a PT or RMT. Setting: patients are seen in person. Content: treatments include manual lymphatic massage, compression bandaging, kinesiotaping, and education. Appointments can be booked for 30 or 60 min. |
Format: no change. Setting: adapted to video or phone. Removed elements: objective measures of lymphedema. Substituted elements: manual therapy was postponed, and patients were provided with online resources for manual lymphatic self-massage (videos and pamphlets). Pacing/timing: no change was made to the scheduled appointment duration. |
| NC, SW, and RD consults | Format: a 1-on-1 visit with the HCP. Setting: primarily in person; however, all visits could be delivered via phone. Content: assessments are guided by distress reports via questionnaires completed in clinic prior to the appointment and objective measures. Appointments are booked for 1 h. |
Format: no change. Setting: all appointments were delivered via phone or video. Tailored elements: questions within standard distress screening questionnaires could be used as probes to guide the assessment, but reports were not available. Removed elements: (1) objective measures of body composition for RD appointments and (2) neuropsychological testing. Pacing/timing: no change was made to the scheduled appointment duration. |
| Education classes | Format: group-based. Setting: in person. Content: monthly 1-h classes. Topics included return to work, brain fog, lymphedema, and sex and intimacy. |
Format: group format was postponed because additional time was required to adapt the content of the classes to a virtual format and ensure privacy concerns were addressed. Patients registered for an upcoming class were contacted by the class lead and offered a 1-on-1 appointment or other resources. Setting: adapted to video or phone consults or online resources. Substituted elements: resources included previously developed e-modules for return to work and brain fog classes, as well as a pamphlet on lymphedema management. E-modules on lymphedema and sex and intimacy were in the process of being developed. |
| Wellness group classes | Format: group-based. Setting: in person; however, cooking classes were streamed live online for patients. Content: classes included cooking and nutrition demonstrations, mindfulness meditation, and gentle therapeutic exercise. |
Format: in-person classes were postponed. Setting: patients were directed to online videos and resources available on the program website and external mediums. Tailored elements: cooking and nutrition classes were streamed live without an in-person audience. Removed elements: (1) mindfulness meditation and (2) gentle therapeutic exercise. |
Abbreviations: MD, medical doctor; NC, neurocognitive; OT, occupational therapist; PT, physiotherapist; RD, registered dietician; RKin, registered kinesiologist; RMT, registered massage therapist; SW, social work.
Process outcomes
The CRS received 221 referrals during the study period, a decrease of 153 relative to the previous 3 months (n=374). Despite the decrease during the initial hospital-wide shift to virtual care, the number of referrals increased substantially over the course of these first 90 days, with 37, 72, and 112 referrals received every 30 days, respectively. Notably, the last 30 days nearly reflected the average rate of referrals per month of in-person care from the previous 3 months (in-person n=125 vs virtual n=112).
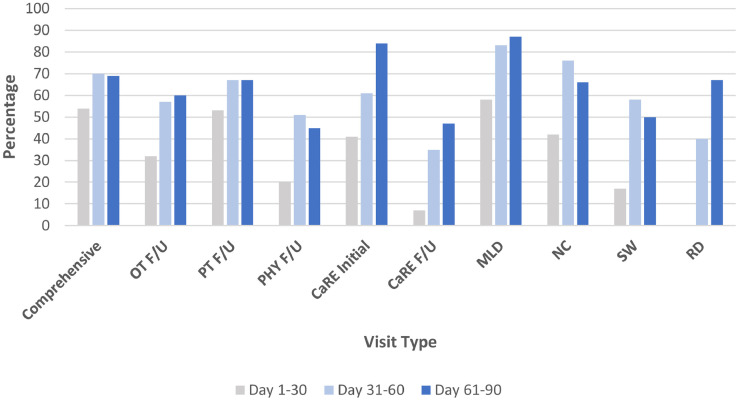
A total of 1968 virtual patient visits were completed during the study period. Attendance rates ranged from 80%-93% across visit types and remained relatively consistent throughout the 90 days (table 2 ). The proportion of appointments completed over video compared with phone increased substantially after the first 30 days (fig 1 ). A further increase in the use of video for virtual appointments was not apparent in the final 30 days of the study period for the majority of visit types; however, the use of video-based visits did continue to increase for CaRE initials, CaRE follow-ups, and dietician follow-ups.
Table 2.
Attendance of virtual appointments (n=1968)
| Visit Type | Day 1-30 |
Day 31-60 |
Day 61-90 |
Total∗ |
|---|---|---|---|---|
| n† (%) | n (%) | n (%) | n (%) | |
| CRS Initial | 119 (82) | 116 (85) | 97 (80) | 332 (83) |
| OT F/U | 34 (79) | 58 (83) | 48 (83) | 140 (82) |
| PT F/U | 36 (80) | 54 (89) | 45 (80) | 135 (83) |
| Physiatry F/U | 88 (91) | 65 (96) | 85 (93) | 238 (93) |
| CaRE Initial | 27 (84) | 54 (79) | 44 (83) | 125 (82) |
| CaRE F/U | 91 (80) | 48 (84) | 57 (85) | 196 (82) |
| CaRE HC | 84 (79) | 186 (91) | 223 (84) | 493 (86) |
| MLD F/U | 26 (90) | 40 (89) | 54 (92) | 120 (90) |
| NC F/U | 12 (80) | 17 (85) | 29 (97) | 58 (89) |
| SW F/U | 18 (56) | 38 (93) | 40 (85) | 96 (80) |
| Diet F/U | 13 (93) | 10 (83) | 12 (80) | 35 (85) |
Abbreviations: CaRE F/U, kinesiology follow-up; CaRE HC, CaRE@Home registered kinesiologist health coaching calls; CaRE Initial, kinesiology initial fitness assessment; CRS initial, initial comprehensive assessment with a physiatrist and occupational therapist or physiotherapist; Diet F/U, dietician follow-up; OT F/U, occupational therapy follow-up; PT F/U, physiotherapy follow-up; MLD F/U, manual lymphatic drainage; NC F/U, neurocognitive follow-up; SW F/U, social work follow-up.
Patients seen for a virtual visit during the 90 days (March 16-June 12) may have been referred to the CRS prior to March 16. Therefore, the total number of visits completed may exceed the total number of referrals during the study period.
Total number of visits attended.
Fig 1.
Proportion of virtual visits completed by video relative to phone for each visit type throughout the 90 days of delivering care virtually. Percentages are displayed for each 30-day period in gray (days 1-30), light blue (days 31-60), and blue (days 61-90).; Abbreviations: CaRE F/U, kinesiology follow-up; CaRE Initial, kinesiology initial fitness assessment; Comprehensive, initial comprehensive assessment with a physiatrist and occupational therapist or physiotherapist; MLD, manual lymphatic drainage; NC, neurocognitive follow-up; OT F/U, occupational therapy follow-up; PT F/U, physiotherapy follow-up; PHY F/U, physiatry follow-up; RD, dietician follow-up; SW, social work follow-up.
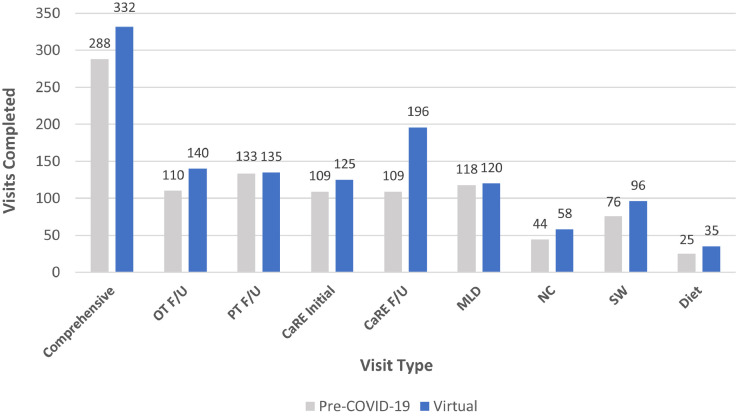
Virtual care demonstrated an increase in the number of completed visits for all appointment types compared with the previous 3 months of in-person care (fig 2 ). Comprehensive assessments (in-person n=288 vs virtual n=332), OT follow-ups (in-person n=110 vs virtual n=140), and CaRE follow-ups (in-person n=109 vs virtual n=196) demonstrated the greatest increase.
Fig 2.
Comparison of the no. of visits completed before and during physical distancing measures. Visits completed are displayed for the 90 days prior to adapting to virtual care (gray) and the first 90 days of delivering care virtually (blue). The number of virtual visits (blue) include telephone and video visits.; Abbreviations: CaRE F/U, kinesiology follow-up; CaRE Initial, kinesiology initial fitness assessment; Comprehensive, initial comprehensive assessment with a physiatrist and occupational therapist or physiotherapist; MLD, manual lymphatic drainage; NC, neurocognitive follow-up; OT F/U, occupational therapy follow-up; PT F/U, physiotherapy follow-up; RD, dietician follow-up; SW, social work follow-up.
The weekly capacities of appointments were adjusted to accommodate setting and format (eg, removal of group classes) modifications, as well as removed need for clinic space. The maximum number of comprehensive assessments that could be scheduled per week slightly decreased (in-person n=40 vs virtual n=36). Nevertheless, the capacity for most 1-on-1 appointments increased. This included OT (in-person n=15 vs virtual n=20), PT (in-person n=15 vs virtual n=25), manual lymphatic drainage (in-person n=13 vs virtual n=15), neurocognitive (in-person n=4 vs virtual n=8), and social work (in-person n=10 vs virtual n=12). The capacity of weekly CaRE assessments decreased slightly (in-person n=28 vs virtual n=24), whereas the capacity of CaRE registered kinesiologist health coaching calls increased substantially (in-person n=32 vs virtual n=75).
The average wait time decreased for comprehensive assessments (12 weeks in-person vs 4 weeks virtual), in part because of the decrease in referrals during the initial hospital-wide shift to virtual care. Similarly, wait times for 1-on-1 follow-ups such as PT and OT (5 weeks in-person vs 3 weeks virtual), neurocognitive (2.5 weeks in-person vs 2 weeks virtual), and social work (2 weeks in-person vs 1 week virtual) decreased slightly. There was no change in the wait time for CaRE initial fitness assessments (4 weeks in-person vs 4 weeks virtual).
There were 168 patients (11% of all comprehensive assessments, 1-on-1 appointments, and CaRE initial or follow-up appointments) who were assessed virtually and identified by CRS staff as requiring an in-person appointment. Reasons included reassessment of suspected musculoskeletal and/or neurologic impairments (n=109 of 168, 65%) and/or lymphedema (n=59 of 168, 35%). Management of patients with musculoskeletal and neurologic conditions often included further assessment to confirm diagnosis, such as identifying the cause(s) of upper quadrant impairment in survivors of breast cancer with significant disability and providing therapy to prevent delays in anticancer therapy (eg, addressing shoulder range of motion restrictions with myofascial release or injections during radiation). Reasons for in-person visits for patients with lymphedema included further assessment with objective limb size measurements and assistance for patients having difficulties learning self-massage or bandaging. These patients were put on a priority waiting list for booking once in-person assessments restarted or were seen in person (n=8) to ensure care was provided in a timely and safe manner.
Experience with virtual care
Twenty-four participants were interviewed (n=12 HCPs and n=12 patients). HCPs included physiatrists (n=2), occupational therapists (n=2), physiotherapists (n=3), kinesiologists (n=2), a dietician (n=1), a social worker (n=1), and a neuropsychologist (n=1). Patient participant demographics are presented in table 3 . Participating patients were referred to the CRS for multiple and varied reasons, including lymphedema (n=6), musculoskeletal (n=5), fatigue (n=5), deconditioning (n=3), neurologic (n=2), difficulties with activities of daily living (n=2), and neurocognitive (n=2) issues. The majority of patient participants were on posttreatment surveillance (n=9, 75%). The mean duration of the interviews was 27 minutes (range, 15-58 minutes). Three themes emerged from the interviews. Each theme is described below and representative quotes for each theme are provided in table 4 .
Table 3.
Patient participant demographics and characteristics (n=12)
| Characteristics | Median (IQR) |
|---|---|
| Age (y) | 56.5 (17) |
| Frequency (%) | |
| Sex | |
| Female | 9 (75) |
| Male | 3 (25) |
| Cancer type | |
| Breast | 5 (42) |
| Gastrointestinal | 2 (17) |
| Leukemia | 1 (8) |
| Lung | 1 (8) |
| Head and neck | 1 (8) |
| Genitourinary | 1 (8) |
| Gynecologic | 1 (8) |
| Ethnicity | |
| White | 6 (50) |
| South Asian | 1 (8) |
| Latin American | 1 (8) |
| Prefer not to answer | 4 (33) |
| Marital status | |
| Married | 6 (50) |
| Single | 5 (42) |
| Divorced | 1 (8) |
| Education | |
| College/university | 7 (58) |
| Prefer not to answer | 5 (42) |
| Work status | |
| Not working | 6 (50) |
| Retired | 3 (25) |
| Working | 2 (17) |
| Prefer not to answer | 1 (8) |
| Annual household income | |
| $40,000-$75,000 | 4 (33) |
| >$75,000 | 1 (6) |
| Prefer not to answer | 7 (58) |
Abbreviation: IQR, interquartile range.
Table 4.
Representative quotes from participant and health care provider interviews
| Theme | Quote |
|---|---|
| Access to care | “Our clinic usually struggles with issues of having enough rooms, so the option of virtual care gives us some more clinic space in a way. I think it’ll solve our issue of clinic space which means we can see more patients or hire more staff and allow our program to grow.” (HCP, occupation therapist) “My acceptance to virtual care has allowed me to see people with very strong barriers to rehabilitation such as those with mobility issues or who live far away.” (HCP, physiatrist) “We have to think about whether we should keep this as an option because maybe I won’t have as easy access to downtown hospitals, but I want to maintain my relationship with my doctors and other providers. This would be an amazing source to rely on until together as a team, you decide on when an in-person appointment would be necessary.” (P08) “Virtual helped me get the care I needed while managing my kids. The convenience was important. If I had to go downtown, I would have to think of a lot of different things to plan my day with the kids and travel. The convenience of it was very helpful.” (P09) |
| Meeting support needs | “The benefit is that we can still connect with patients and they seem to really appreciate that we can speak with them. We can still build a therapeutic relationship with patients and still provide some sort of connection and opportunity to check in. So, I think that has been working well. I think we actually have been needed more now as many other points of connection may have stopped.” (HCP, occupation therapist) “I think it would be helpful to tell patients what to expect for the virtual visit. So, like a module or link on how to make the most out of the visit. Giving them steps like arriving five minutes before the visit, test the camera and audio, wear clothes for exercise, bring any equipment they have. Also, continuing to communicate the expectations of the visit and that there are going to be limitations for what we can assess virtually.” (HCP, physiotherapist) “I feel I got really great guidance. I feel continued to be cared for. If I need support or more understanding because something changes, I feel like I could reach out and I can get help. And with the continued uncertainty in the world, it might be necessary to be virtual for the next year. So, it feels really good moving forward.” (P02) “I feel blessed for this opportunity. I was given the confidence to manage my wellness, and needed support during a pandemic. You can feel like you’re still working towards something that is going to help you. I think it has made an improvement in my physical and mental life. I had tools that were able to help me handle the cancer and the COVID situation.” (P04) |
| Confidence with assessment and care plan | “Assessing range of motion is okay for upper extremities, but sometimes people don’t have that mobility with their camera to show their whole body or a good distance from the camera. It’s hard to get a good visual of their lymphedema unless the swelling is quite pronounced and visible. Also, often we’re doing this over the phone, where I can only go by patient description about their mobility, strength, and lymphedema.” (HCP, physiotherapist) “We also have an app we use where patients see the videos and instructions of the exercises, and they can message us on that if they have questions. Through that, we can also share our screen and show them the videos on the app and show the videos and talk it through with them. This makes it easier to teach the exercises and build rapport.” (HCP, kinesiologist) “I might have the language to be able to describe what I’m feeling, but the majority might not be able to. So, for someone who doesn’t know a lot about the body and can’t see or tell if something bad is going on, then you’re relying on self-description and they may not describe it well or accurately. Not being able to have a someone go and feel my armpit for example and feel what’s swollen, or even look at it well is a problem because you can’t visibly see something like that well on a screen.” (P06) “The worry about the care not being very personalized was removed right away during the first appointment because I could see [the health care provider], they could see me, and we could communicate with each other. I didn’t really know how I was going to be able to say a certain exercise was not okay for me because you can’t do an exercise in front of someone virtually. It just doesn’t work for me or them actually. So, the video of the exercises were shown to me during the appointment and everything was explained to me so well that it removed all my worries and made it easy.” (P11) |
Abbreviation: P, participant.
Theme 1: access to care
Patient and HCP participants highlighted the ability for virtual care to increase access and attendance to rehabilitation programming. Patients emphasized being able to better manage household and childcare responsibilities while attending virtual appointments, as well as managing multiple visits and transportation. HCPs highlighted the potential to increase the program’s capacity because of reduced burden for additional clinic space. Despite patient participants being highly receptive to virtual care, there were a few concerns regarding access. Some patients indicated challenges accessing a private space to discuss their health issues at home. Additionally, some communicated barriers to accessing the virtual platform, including receiving multiple emails for various hospital appointments and a lack of description for the appointment on the automated email and platform. In some cases, this led to patients not being initially aware of the purpose of the visit or the reason for the referral. As a result, HCPs recommended providing pertinent information to patients prior to the appointment (eg, instructions on how to access the virtual platform, guidelines on ensuring high-quality virtual appointments).
Theme 2: meeting support needs
Patient participants expressed a sense of reassurance and noted that they felt supported during a time of isolation and uncertainty. Several patients emphasized feeling empowered to cope with the worries of the pandemic in addition to their rehabilitation needs. Furthermore, patient and HCP participants indicated that they were able to establish rapport, particularly during video appointments because this normalized the virtual care experience. However, several HCPs indicated that compared with in-person appointments, communication barriers were more pronounced in a virtual environment, which hindered their ability to assess and build rapport with patients using interpretation services. Additionally, a few patient participants described virtual care as an isolating approach to their rehabilitation and expressed a desire for virtual group interactions with other survivors of cancer. This was acknowledged by many HCPs, who discussed challenges with abruptly adapting the group classes to a virtual platform.
Theme 3: confidence with assessment and care plan
HCPs indicated that virtual visits were effective for screening many cancer-related impairments, including neurocognitive, psychosocial, fatigue, and diet concerns. However, HCPs, specifically physical therapists, occupational therapists, and physiatrists, experienced more difficulties because of limitations in assessing musculoskeletal and neurologic impairments and lymphedema. Because of a lack of in-person examination, HCPs often relied on patient self-report and self-assessment. Virtual visits made it difficult to reliably test, palpate, and observe patients to evaluate their level of impairment and function. This led to a greater level of difficulty narrowing the differential diagnosis, ordering pertinent medical tests, and evaluating their condition at follow-up appointments. HCPs also indicated several challenges teaching locoregional rehabilitative exercises (eg, pelvic floor strengthening, upper quadrant range of motion), resistance exercises, and lymphatic self-massage and bandaging. Limitations included distances and angles of patients’ cameras and availability of space for patients to demonstrate these movements for the HCP. This reflected patient participants’ concerns about the absence of an in-person assessment. Many felt worried about how accurately they were describing their physical limitations and symptoms. Nevertheless, most patients indicated that their confidence with receiving care virtually was increased with the provision of online resources and materials, such as a mobile application to guide exercise. Moreover, patients and HCPs agreed that video-based appointments provided a greater sense of confidence with the examination and care plan than telephone visits. Finally, patients and HCPs expressed a preference for an initial in-person assessment, particularly for those with moderate to severe physical impairments, followed by shared decision making regarding the appropriate setting for follow-up appointments.
Discussion
This study describes the adaptations made to implement virtual cancer rehabilitation programming at the onset of the COVID-19 pandemic. The rapid shift to virtual care presented a challenge and an opportunity to ensure survivors of cancer had access to rehabilitation services. The CRS was able to translate the majority of appointments to virtual formats and deliver care at similar or greater volumes compared to in-person care prior to the pandemic.
Virtual delivery is a priority in cancer rehabilitation because of its ability to mitigate barriers to in-person care.4 , 17 , 18 Our findings demonstrate that virtual care may be feasible, consistent with previous studies,19, 20, 21 with a few important limitations for physical examinations (eg, musculoskeletal and neurologic impairments, lymphedema). We were able to deliver care at high volumes and attendance rates across a variety of visit types. Our findings suggest that survivors of cancer feel they can easily access care and gain confidence in learning skills to self-manage their impairments. However, the value of group-based interventions was highlighted in this study, reflecting previous findings on their social benefits.22 Accordingly, we have begun piloting virtual group education classes.
The ability of the CRS to abruptly shift to virtual care was facilitated by regulations surrounding billing for virtual care as well as organizational capacity and readiness for change.23 The provincial government approved virtual care to be covered by insurance and introduced temporary billing codes and procedures. Additionally, the Princess Margaret Cancer Centre had been delivering virtual appointments on OTN in a limited capacity prior to the pandemic, which facilitated its rapid adoption within the CRS, and all HCPs were trained on how to navigate OTN prior to delivering care virtually. Finally, previous use of telephone visits (eg, return to work, social work) and previously developed resources (eg, e-modules) may have facilitated implementation. The abovementioned factors are consistent with previous research suggesting that the readiness of the environment can lead to successful implementation of virtual care, including policies and regulations, and the capacity to manage virtual care infrastructure and effects on staffing times and multiprofessional work roles.24, 25, 26
Performing physical examinations during virtual rehabilitation visits, particularly via telephone, is a key limitation to this form of delivery.27 During the study period, there were several patients wait-listed for an in-person visit, echoing shared concerns of interviewed patients and HCPs on the accuracy and reliability of the assessment. Additional considerations may include difficulties communicating because of language barriers or speech impairments, as well as cognitive impairments making it difficult to navigate a virtual platform. Such considerations for virtual care have been recently discussed.9 The inability for some patients to access and navigate video-based platforms posed a challenge to HCPs because they were unable to observe the patient’s impairment and therefore had to rely on patient self-report. Therefore, further attention to health literacy may be warranted because of the benefits of accurately describing symptoms, monitoring impairments, and making informed clinical decisions.28, 29, 30 Lastly, the video quality and distances to cameras can make it difficult for HCPs and patients to demonstrate and perform tests and exercises, consistent with previously suggested limitations to virtual assessments.27 Efforts to improve access and the quality of virtual appointments for individuals with limited knowledge about technology may be warranted.
Based on our findings, we have suggested practical recommendations for HCPs (table 5 ). These recommendations encompass strategies for the following: (1) pragmatic and logistical considerations; (2) communicating expectations of virtual visits; (3) understanding patient capabilities and concerns; and (4) prescribing individualized self-management strategies. These strategies add to previous recommendations for conducting virtual care.9 , 10 , 31 Factors such as selecting appropriate and multiple modes of virtual delivery, providing patients with instructions about the virtual visit, and using mobile applications to monitor exercise can facilitate the transition and delivery of virtual care.
Table 5.
Health care provider perspectives on recommendations for virtual care
| Considerations | Recommendations |
|---|---|
| Pragmatic and logistical |
|
| Communicating expectations of virtual visits |
|
| Understanding patient capabilities and concerns |
|
| Prescribing individualized self-management strategies |
|
Study limitations
Although this study has strengths, including the use of multiple methods to provide a comprehensive understanding of factors that may facilitate the implementation of virtual care, there are also limitations that warrant mention. We did not compare demographic information on the patients seen virtually and in-person. Factors such as the geographic distribution of patients accessing care as well as the characteristics of patients attending video vs phone assessments will provide additional insight into the accessibility and reach of virtual care. Additionally, although this study described the changes to the CRS process outcomes over time, we did not determine whether these changes were significant. Moreover, we did not examine the effectiveness of virtual care. Previous research on virtual cancer rehabilitation has shown promising results in patients managing functional and cognitive impairments, as well as pain and depression.32, 33, 34, 35 Further research on the effectiveness of the program will provide additional insight into the advantages and disadvantages of virtual care. Finally, given the relatively small number of patient participants interviewed, the qualitative findings should be interpreted in the context of the participant sample. Further research is needed to understand potential differences in the utility of virtual rehabilitation for different cancer types, rehabilitation needs, and work status, to name a few.
Conclusions
The findings of this study suggest that many appointments can be successfully adapted to virtual formats to deliver cancer rehabilitation programming. Virtual delivery can be a feasible and acceptable alternative to in-person care during physical distancing recommendations. Although these findings are encouraging and can inform implementation efforts for virtual models, further research is needed to understand its effectiveness.
Footnotes
Disclosures: none.
Supplementary data
References
- 1.Silver J.K., Baima J., Mayer R.S. Impairment-driven cancer rehabilitation: an essential component of quality care and survivorship. CA Cancer J Clin. 2013;63:295–317. doi: 10.3322/caac.21186. [DOI] [PubMed] [Google Scholar]
- 2.Cheville A.L. Adjunctive rehabilitation approaches to oncology. Phys Med Rehabil Clin North Am. 2017;28:i. [Google Scholar]
- 3.Nekhlyudov L., Duijts S., Hudson S.V., et al. Addressing the needs of cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2020;14:601–606. doi: 10.1007/s11764-020-00884-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cox A., Lucas G., Marcu A., et al. Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res. 2017;19:e11. doi: 10.2196/jmir.6575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agboola S.O., Ju W., Elfiky A., Kvedar J.C., Jethwani K. The effect of technology-based interventions on pain, depression, and quality of life in patients with cancer: a systematic review of randomized controlled trials. J Med Internet Res. 2015;17:e65. doi: 10.2196/jmir.4009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larson J.L., Rosen A.B., Wilson F.A. The effect of telehealth interventions on quality of life of cancer patients: a systematic review and meta-analysis. Telemed J E Health. 2018;24:397–405. doi: 10.1089/tmj.2017.0112. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein R.S., Lopez A.M., Joseph B.A., et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med. 2014;127:183–187. doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Dorsey E.R., Topol E.J. State of telehealth. N Engl J Med. 2016;375:154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 9.McIntyre M., Robinson L.R., Mayo A. Practical considerations for implementing virtual care in physical medicine and rehabilitation: for the pandemic and beyond. Am J Phys Med Rehabil. 2020;99:464–467. doi: 10.1097/PHM.0000000000001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verduzco-Gutierrez M., Bean A.C., Tenforde A.S., Tapia R.N., Silver J.K. How to conduct an outpatient telemedicine rehabilitation or prehabilitation visit. PM R. 2020;12:714–720. doi: 10.1002/pmrj.12380. [DOI] [PubMed] [Google Scholar]
- 11.Wiltsey Stirman S., Baumann A.A., Miller C.J. The FRAME: an expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement Sci. 2019;14:58. doi: 10.1186/s13012-019-0898-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald A.M., Chafranskaia A., Lopez C.J., et al. CaRE @ Home: pilot study of an online multidimensional cancer rehabilitation and exercise program for cancer survivors. J. Clin. Med. 2020, 9, 3092. J Clin Med. 2020;9:3440. doi: 10.3390/jcm9103092. Addendum: MacDonald, A.M., et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green J, Thorogood N. Qualitative methods for health. 3rd ed. Los Angeles: SAGE; 2014.
- 14.Bowen G.A. Document analysis as a qualitative research method. Qual Res J. 2009;9:27–40. [Google Scholar]
- 15.Braun V, Clarke V. Thematic analysis. In: APA handbook of research methods in psychology, vol 2: research designs: quantitative, qualitative, neuropsychological, and biological. Washington (DC): American Psychological Association; 2012. p 57-71.
- 16.Tracy S.J. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq. 2010;16:837–851. [Google Scholar]
- 17.Pergolotti M., Alfano C.M., Cernich A.N., et al. A health services research agenda to fully integrate cancer rehabilitation into oncology care. Cancer. 2019;125:3908–3916. doi: 10.1002/cncr.32382. [DOI] [PubMed] [Google Scholar]
- 18.Brennan D.M., Mawson S., Brownsell S. In: Advanced technologies in rehabilitation. Gaggioli A., Keshner E.A., Weiss P.L., et al., editors. IOS Press; Amsterdam, Netherlands: 2009. Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self management; pp. 231–248. [Google Scholar]
- 19.Burton R.L., O’Connell M.E. Telehealth rehabilitation for cognitive impairment: randomized controlled feasibility trial. J Med Internet Res. 2018;20:e43. doi: 10.2196/resprot.9420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coats V., Moffet H., Vincent C., et al. Feasibility of an eight-week telerehabilitation intervention for patients with unresectable thoracic neoplasia receiving chemotherapy: a pilot study. Can J Respir Crit Care Sleep Med. 2020;4:14–24. [Google Scholar]
- 21.Villaron C., Cury F., Eisinger F., Cappiello M.A., Marqueste T. Telehealth applied to physical activity during cancer treatment: a feasibility, acceptability, and randomized pilot study. Support Care Cancer. 2018;26:3413–3421. doi: 10.1007/s00520-018-4191-4. [DOI] [PubMed] [Google Scholar]
- 22.Midtgaard J., Hammer N.M., Andersen C., Larsen A., Bruun D.M., Jarden M. Cancer survivors’ experience of exercise-based cancer rehabilitation - a meta-synthesis of qualitative research. Acta Oncol. 2015;54:609–617. doi: 10.3109/0284186X.2014.995777. [DOI] [PubMed] [Google Scholar]
- 23.Weiner B.J. A theory of organizational readiness for change. Implement Sci. 2009;4:67. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jennett P.A., Andruchuk K. Telehealth: “real life” implementation issues. Comput Methods Programs Biomed. 2001;64:169–174. doi: 10.1016/s0169-2607(00)00136-x. [DOI] [PubMed] [Google Scholar]
- 25.Schreiweis B., Pobiruchin M., Strotbaum V., Suleder J., Wiesner M., Bergh B. Barriers and facilitators to the implementation of eHealth services: systematic literature analysis. J Med Internet Res. 2019;21 doi: 10.2196/14197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jafni T.I., Bahari M., Ismail W., Radman A. Understanding the implementation of telerehabilitation at pre-implementation stage: a systematic literature review. Procedia Comput Sci. 2017;124:452–460. [Google Scholar]
- 27.Tenforde A.S., Hefner J.E., Kodish-Wachs J.E., Iaccarino M.A., Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9:S51–S58. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 28.Kim H., Goldsmith J.V., Sengupta S., et al. Mobile health application and e-Health literacy: opportunities and concerns for cancer patients and caregivers. J Cancer Educ. 2019;34:3–8. doi: 10.1007/s13187-017-1293-5. [DOI] [PubMed] [Google Scholar]
- 29.Koay K., Schofield P., Jefford M. Importance of health literacy in oncology. Asia Pac J Clin Oncol. 2012;8:14–23. doi: 10.1111/j.1743-7563.2012.01522.x. [DOI] [PubMed] [Google Scholar]
- 30.Jensen J.D., King A.J., Davis L.A., Guntzviller L.M. Utilization of internet technology by low-income adults: the role of health literacy, health numeracy, and computer assistance. J Aging Health. 2010;22:804–826. doi: 10.1177/0898264310366161. [DOI] [PubMed] [Google Scholar]
- 31.Newton R.U., Hart N.H., Clay T. Keeping patients with cancer exercising in the age of COVID-19. JCO Oncol Pract. 2020;16:656–664. doi: 10.1200/OP.20.00210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheville A.L., Moynihan T., Herrin J., Loprinzi C., Kroenke K. Effect of collaborative telerehabilitation on functional impairment and pain among patients with advanced-stage cancer: a randomized clinical trial. JAMA Oncol. 2019;5:644–652. doi: 10.1001/jamaoncol.2019.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lyons K.D., Hull J.G., Kaufman P.A., et al. Development and initial evaluation of a telephone-delivered, behavioral activation, and problem-solving treatment program to address functional goals of breast cancer survivors. J. Psychosoc Oncol. 2015;33:199–218. doi: 10.1080/07347332.2014.1002659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bray V.J., Dhillon H.M., Bell M.L., et al. Evaluation of a web-based cognitive rehabilitation program in cancer survivors reporting cognitive symptoms after chemotherapy. J Clin Oncol. 2017;35:217–225. doi: 10.1200/JCO.2016.67.8201. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K., Theobald D., Wu J., et al. Effect of telecare management on pain and depression in patients with cancer. JAMA. 2010;304:163. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.