Abstract
This study explored whether fertility-specific distress varied by race/ethnicity among a nationally representative sample of US women. Participants were 2363 White (n = 1266), Black (n = 569), Hispanic (n = 453), and Asian (n = 51) women who participated in the National Survey of Fertility Barriers. Participants were given the Fertility-Specific Distress Scale and assessed for strength of pregnancy intent, primary versus secondary infertility, and socioeconomic hardship. Black women reported lower levels of fertility-specific distress than White women, but these were fully mediated by the strength of pregnancy intentions. Primary versus secondary infertility and economic hardship were not associated with fertility-specific distress.
Keywords: black, disparities, distress, ethnicity, hispanic, infertility, race, white
Introduction
According to identity theory (Stryker, 1980), barriers to achieving or maintaining a valued identity should lead to a failure in identity verification, or an identity disruption (Burke and Stets, 2009). Identity disruptions have greater impact when the gap between desire and reality is large, when the interruption is not a result of choice, and when there is high commitment to the disrupted identity (Burke, 1991). Identity theory has been applied to the experience of infertility (McQuillan et al., 2003; Matthews and Martin-Matthews, 1986). Because infertility is often experienced as a failure to achieve a deeply desired identity (Becker, 2000; Exley and Letherby, 2001), infertility can lead to psychological distress (Johansson and Berg, 2005; Klemetti et al., 2010; Sexton et al., 2010). Little is known, however, about possible differences in levels of infertility-related distress among racial/ethnic groups in the United States. This study addresses this gap in the literature.
According to commonly accepted medical criteria, women are considered infertile if they experience a year or more of regular, unprotected, intercourse without conception (American Society for Reproductive Medicine, 2008). While the medical definition appears to assume that all women having regular, unprotected intercourse are trying to conceive, not all women fitting this definition describe themselves as actively trying to become pregnant. Many women who engage in regular, unprotected intercourse say they are “okay either way” with becoming pregnant (McQuillan et al., 2011). Medical professionals further classify women as having either primary or secondary infertility. The term “primary infertility” denotes infertility in women who have never achieved a pregnancy, whereas “secondary infertility” refers to infertile women who have previously been pregnant.
Using the medical definition of infertility as 1 year of regular, unprotected intercourse without conception, the National Survey of Family Growth estimated that 7.4 percent of married US women were currently infertile in 2002 (Chandra and Stephen, 2006). In a probability-based sample of women aged 25–50 years in 12 Midwestern states, 38 percent of all women, regardless of relationship status, reported infertility at some point in their lives (White et al., 2006). Pooled data from the 1982–2002 National Survey of Fertility Growth (NSFG) surveys revealed that among currently married women, infertility rates for Black (12.0%) and Hispanic (9.2%) women were higher than those for White women (6.9%) (Bitler and Schmidt, 2006). Despite evidence that infertility is distressing, fewer than 50 percent of infertile US women receive medical services for infertility (Chandra and Stephen, 2010). Bitler and Schmidt (2006) found statistically significant differences by race among a nationally representative sample of US women: 15.8 percent of White women, 10.7 percent of Black women, and 12.2 percent of Hispanic women reported ever having received medical services for infertility.
Most studies of infertility-related distress depend on clinic-based samples (Henning and Strauss, 2002). A focus on people receiving treatment makes it difficult to generalize to those who do not (Greil et al., 2010b). Ideally, an investigation of racial/ethnic differences in distress related to infertility should include those who have not received treatment as well as those who have. Therefore, one goal of this study was to examine a sample of women who have ever met criteria for infertility whether or not they have sought medical help. Many quantitative studies of the psychosocial concomitants of infertility use general measures of psychological distress, such as measures of depression or global life satisfaction. Such general measures of distress are unlikely to be sufficiently sensitive or specific to the problems of infertility to adequately reflect the experience of many women (Jacob et al., 2007; Schmidt, 2009). Specific measures of infertility distress are strongly correlated with standardized measures of distress, indicating their face validity (Abbey et al., 1992). A measure of fertility- specific distress would be more likely to uncover racial/ethnic differences in infertility distress; we therefore used such a measure in this study.
Because most infertility clinic patients are White and middle-class, most studies of infertility have focused primarily on White, middle-class, infertile women (Culley et al., 2009). The few studies that do exist concerning infertility among women of color are based on small, non-random samples and usually focus on just one group. These smaller studies suggest that such experiences as loss of control, grief, and feelings of social isolation are found among racially marginalized women as well as among White women (see Becker et al., 2005; Ceballo et al., 2012; Inhorn et al., 2009; Szkupinski-Quiroga, 2007). We are aware of only two studies that compare psychological distress among women of various racial/ethnic groups among a probability-based sample (Greil et al., 2011b; Jacob et al., 2007). Neither of these studies found racial/ethnic differences in psychological distress, but neither was designed in such a way as to maximize the chance of finding such differences. One study (Jacob et al., 2007) failed to distinguish between different non-White groups, and neither study considered whether there might be indirect associations between race/ethnicity and psychological distress. Hence, we have advanced prior work by examining direct and indirect associations between race/ethnicity and psychological distress using a measure of fertility-specific distress.
Identity theory suggests that women who are more committed to the parent identity should be more distressed by infertility. Some evidence indicates that Black (Dunlap et al., 2006; Kendall et al., 2005) and Hispanic (Bengston, 2001; Skogrand et al., 2009) women are more committed to having children than White women. Because Black and Hispanic women are more likely to have their first child at a young age, secondary infertility is more common than primary infertility compared to White and Asian women (Greil et al., 2011a). Therefore, although infertility is more common, involuntary childlessness is less common. Even though infertility rates are higher among women of color, there are still high expectations of pregnancy among women of color (Ceballo et al., 2012). Szkupinski-Quiroga (2002) found that the infertile women of color she interviewed experienced infertility, not only as a challenge to personal identity, but as a challenge to ethnic identity as well, because they saw having children as a fundamental aspect of being full-fledged members of their ethnic communities. Ceballo et al. (2012) found that African American women’s sense of isolation and loneliness were heightened by their internalization of cultural stereotypes about race and reproduction and by their sense that infertility is a “White thing.” If women of color have stronger intentions to conceive, then we would expect to find higher levels of fertility-specific distress among infertile women of color.
Yet historical and contemporary circumstances may discourage Black and Hispanic women from trying to conceive instead of simply being open to conception. McQuillan et al. (2008) found that Black and Hispanic women had lower scores on a scale intended to measure importance of motherhood than White women. These same authors (McQuillan et al., 2012) also found, however, that their importance of motherhood measure did not exhibit measurement invariance across racial groups, suggesting that it may not be a suitable measure of racial differences in commitment to the motherhood identity. Historical and contemporary discrimination and socioeconomic inequality associated with race/ethnicity create contexts that lead to adverse circumstances for raising racial/ethnic minority children (Roberts, 1997). Because race/ethnicity is associated with social class, it is important to assess whether any association between race/ethnicity and fertility- specific distress is mediated by socioeconomic status.
The relationship between race/ethnicity and fertility-specific distress may be mediated by other factors in addition to socioeconomic status. Greil and McQuillan (2004) and Jacob et al. (2007) categorized infertile women into those with strong intent to become pregnant (women who say they tried to conceive for at least 12 months without conception) and those with weak intent to become pregnant (women who report having had unprotected intercourse without conception but who say they were “okay either way” when asked if they wanted to become pregnant at that time). Strong pregnancy intent is associated with higher fertility-specific distress than lower pregnancy intent (Greil et al., 2009, 2011b). On average, Black and Hispanic women have weaker pregnancy intent than White women (Greil et al., 2011a). It is therefore important to assess whether measures of pregnancy intent explain racial/ethnic differences in fertility-specific distress. Identity theory suggests that infertile women with stronger pregnancy intent, regardless of race/ ethnicity, will experience a larger gap between real and ideal states and thus report greater fertility-specific distress.
Differences in the incidence of primary versus secondary infertility among women in different racial/ethnic subgroups should also explain differences in fertility-specific distress between subgroups of women. Some studies have found that women with primary infertility exhibit higher levels of distress than women with secondary infertility (Epstein and Rosenberg, 2005; Greil et al., 2011b; Verhaak et al., 2007). Black and Hispanic women are more likely than White or Asian women to suffer from secondary infertility, possibly because more Black and Hispanic have their first child at younger ages than White women (Mathews and Hamilton, 2009). Identity theory suggests that, because infertile women who have never been pregnant have a larger gap between real and ideal status than those who have been pregnant, they should therefore experience more fertility-specific distress. Thus, any group differences in fertility-specific distress could be due to higher rates of primary infertility among White women than among Black or Hispanic women.
Differences in the historical experiences of fertility, infertility, helpseeking for infertility, and importance of motherhood between women in different racial/ethnic groups suggest that fertility-specific distress might be higher among White women compared to women of color. Yet differences in rates of primary versus secondary infertility, strength of pregnancy intent, and socioeconomic status by race/ethnicity could explain why fertility-specific distress is lower among Black and Hispanic compared to White and Asian women. This study therefore addressed important questions in the psychosocial study of infertility by testing whether or not fertility-specific distress varied by race/ethnicity among a broad spectrum of US women and what factors explained any differences.
Methods
Participants
This study examined the relationship between race/ethnicity and fertility-specific distress in the National Survey of Fertility Barriers (NSFB), a study employing a nation-wide probability sample of 4712 US women. Oversampling of Census central office codes with high Black or Hispanic populations helped to adequately represent these women: 19.6 percent of the total sample and 24.8 percent of ever-infertile women identify as Black, and 17.9 percent of the total sample and 19.7 percent of ever-infertile women identify as Hispanic. Interviewing was conducted by the Survey Research Center at the Pennsylvania State University and the Bureau of Sociological Research at the University of Nebraska-Lincoln using the same interviewer training and procedures.
The sample for this study consisted of 2363 women, 53.6 percent White (n = 1266), 24.1 percent Black (n = 569), 19.2 percent Hispanic (n = 453), and 2.2 percent Asian (n = 51) women who ever experienced a period of at least 1 year of regular unprotected intercourse without conception (the medical definition of infertility). Women who said they were trying not to become pregnant during their episode of at least 1 year of regular unprotected intercourse without conception were excluded from the sample. The sample included both women who have received treatment (whether or not they have received a definitive diagnosis of infertility) as well as those who have not received treatment.
Because the original survey was long, respondents were randomly assigned to two-thirds of the items for each scale, which shortened the survey to an average of 35 minutes. This “planned missing” design retained all of the essential concepts, minimized respondent burden, and minimized bias by adding only missing data that is “missing completely at random” (Allison, 2002). The response rate for the screener was 53.7 percent, which is typical for telephone surveys conducted in the last several years (McCarty et al., 2006). To assess the representativeness, we compared it to the NSFG, a population-based survey with a response rate close to 90 percent and found very similar responses to equivalent fertility-specific and demographic questions in the two surveys.
Measures
Fertility-specific distress.
The Fertility-Specific Distress Scale was a 6-item scale constructed by the creators of the NSFB based on the questions that draw on Hjelmstedt et al.’s (1999) Infertility Reaction Scale, qualitative research on infertile couples, and the clinical experience of members of the research team. Respondents were presented with a series of items and asked whether they felt this way frequently, occasionally, seldom, or never. The items were “I felt cheated by life,” “I felt that I was being punished,” “I felt angry at God,” “I felt inadequate,” “I felt seriously depressed about it,” and “I felt like a failure as a woman.” Items were recoded so that a higher score indicated greater distress. Fertility-specific distress is treated as a latent variable constructed from the six individual items. The analysis uses the full information maximum likelihood estimation method in Mplus to take missing data into account. The Fertility-Specific Distress Scale has a high degree of internal consistency (α = .83) for this sample.
Race/ethnicity.
Race/ethnicity was measured using the two standard Census questions (US Census Bureau, 2011). Using commonly accepted classification procedures, individuals who reported multiple races were classified giving first priority to identification as “Hispanic” and second priority to identification as “Black.” Based on this coding, dummy variables were constructed for Black, Hispanic, and Asian compared to White. Due to small cell counts, those coded as “other” were combined with Whites, as previous experience with this data set has demonstrated that the two groups are quite similar. Although all racial/ethnic groups contain heterogeneous subgroups, these larger categories are indicators of gross distinctions that reflect patterns of racial/ethnic formation in the United States.
Mediating variables.
The three mediating variables in our model were as follows: strength of pregnancy intention, primary versus secondary infertility, and economic hardship. We used strength of intention to become pregnant rather than importance of motherhood as a measure of commitment to the motherhood identity because the importance of motherhood measure does not exhibit measurement invariance across racial groups and because the strength of intentions measure has been shown to be associated with fertility-specific distress and infertility service utilization in other studies (Greil et al., 2011b). Women who described themselves as trying to become pregnant at the time of their infertility episode were classified as having strong pregnancy intent. Women who did not report trying to become pregnant during their infertility episode were classified as having weak pregnancy intent.
Respondents were classified as having primary infertility if they experienced a period of infertility before they had experienced any pregnancies. The remainder of respondents had at least one pregnancy before their first infertility episode and therefore experienced secondary infertility. Women with a prior pregnancy but no live birth were classified as having secondary infertility because prior research indicates that they are more similar to infertile women with a prior pregnancy than to those without a prior pregnancy (Greil et al., 2010a). To measure socioeconomic status, we used a measure that has elsewhere been called perceived economic hardship and was based on responses to the following questions: (1) During the last 12 months, how often did it happen that you had trouble paying the bills?; (2) During the last 12 months, how often did it happen that you did not have enough money to buy food, clothes, or other things your household needed?; and (3) During the last 12 months, how often did it happen that you did not have enough money to pay for medical care? This unidimensional scale had high internal consistency (α = .82).
Data analysis plan
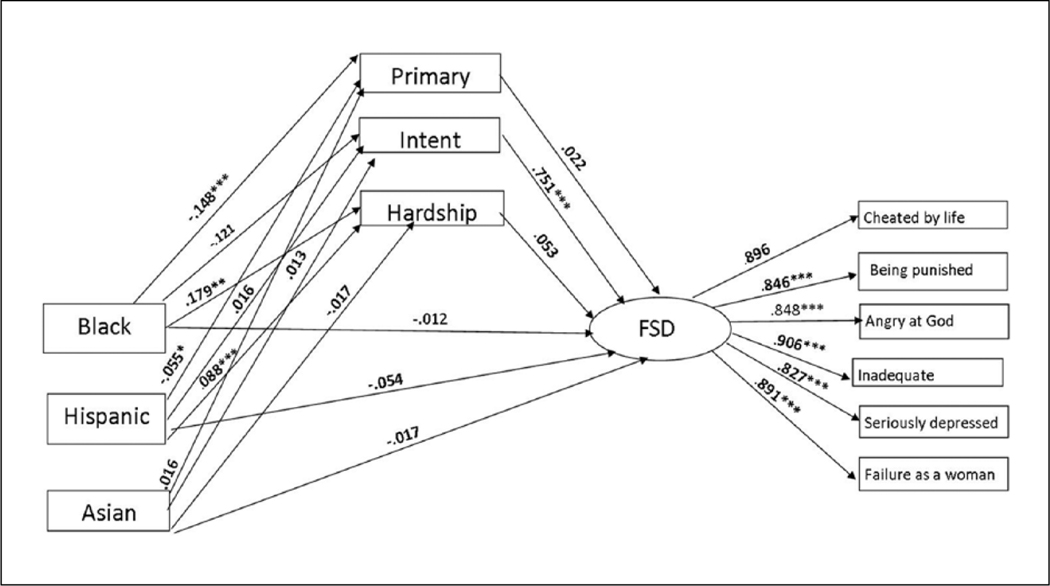
Data analysis was conducted by estimating a structural equation model looking at the effects of race/ethnicity on fertility-specific distress. Fertility-specific distress was modeled as a latent variable constituted by the 6 individual items of the fertility-specific distress scale. Primary infertility, strong pregnancy intent, and economic hardship were left free to correlate with one another. The dummy variables for race/ethnicity were modeled as having direct effects on fertility-specific distress as well as indirect effects through the mediating variables.
Results
Bivariate analysis (not shown here) indicated that Black and Hispanic women with infertility are less likely (25.0% and 31.6%, respectively), and Asian women (54.0%) are more likely to have primary infertility than are White women (37.1%). White women with infertility were more likely (53.3%) to have strong pregnancy intent than Black women (42.0%). Both Black and Hispanic women with infertility had higher mean hardship scores (.086) than White women. In the bivariate analysis, Black women have significantly lower fertility-specific distress (.26) than White women.
Table 1 presents coefficients from the structural equation model with mediators added as well as data on the direct and indirect effect of racial/ethnic groups on fertility-specific distress. Figure 1 presents the same data in graphic form. None of the direct effects indicated that racial/ethnic groups differed in fertility-specific distress from Whites. Black and Hispanic women had lower odds (odds ratio (OR) = .705 and .868, respectively) and Asian woman higher odds (OR = 1.575) of having primary infertility than White women, but primary infertility was not associated with fertility-specific distress. Black women had lower odds (OR = .752) of having strong pregnancy intent than White women. Women with strong pregnancy intent had higher fertility-specific distress than those with weak pregnancy intent (β = .751). That the indirect but not the direct association between “Black” and fertility-specific distress was significant indicates that the Black–White difference in fertility-specific distress was fully mediated by strength of pregnancy intent. Black and Hispanic women had greater odds (OR = 1.39 and OR = 1.198, respectively) of experiencing economic hardship compared to White women, but economic hardship was not related to fertility-specific distress. Therefore, economic hardship did not mediate the association between race/ethnicity and fertility-specific distress.
Table 1.
Direct and indirect effects of race- and fertility-specific distress and other variables among infertile women (n = 2363).
| Direct effects | Difference between Black and White women |
Difference between Hispanic and White women |
Difference between Asian and White women |
Effect on fertility-specific distress |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | OR/β | B | SE | OR/β | B | SE | OR/β | B | SE | OR/β | |
| Primary infertility | −.35 | .07 | .71*** | −.14 | .07 | .87* | .45 | .18 | 1.58* | −.02 | .05 | −.02 |
| Infertile with intent | −.29 | .06 | .75*** | .04 | .07 | 1.04 | .09 | .18 | 1.09 | .67 | .05 | .75*** |
| Economic hardship | .34 | .04 | 1.40*** | .18 | .04 | 1.20*** | −.17 | .13 | .85 | .06 | .03 | .05 |
| FSD | −.03 | .06 | −.01 | −.13 | .07 | −.05 | −.11 | .17 | −.02 | |||
| R2 | .54 | |||||||||||
| Direct, indirect, and total effects | Black |
Hispanic |
Asian |
|||||||||
| Standard coefficient | Standard coefficient | Standard coefficient | ||||||||||
| Indirect through | ||||||||||||
| Primary infertility | .00 | .00 | .00 | |||||||||
| Infertile with intent | −.09*** | .01 | .01 | |||||||||
| Economic hardship | .01 | .01 | .00 | |||||||||
| Direct effects | −.01 | −.05 | −.02 | |||||||||
| Total indirect effects | −.08*** | .02 | .01 | |||||||||
| Total effects | −.09** | −.04 | −.01 | |||||||||
SE: standard error; OR: odds ratio; FSD: female sexual dysfunction.
OR computed for categorical and β computed for continuous dependent variables.
p< .05
p<.001.
Figure 1.
Effects of race on fertility-specific distress among infertile women.
CFI: comparative fit index; TLI: Tucker–Lewis index; RMSEA: root mean square error of approximation.
Chi-square = 56.277; p = .036; CFI = .998; TLI = .997; RMSEA = .014.
Discussion
Guided by identity theory, this study sought to explore an understudied area in the psychosocial literature on infertility among women, namely, potential racial/ethnic differences in fertility-specific distress. This analysis showed that Black women have lower fertility-specific distress than non-Hispanic White women. Hispanic and Asian women did not have significantly different fertility-specific distress scores than non-Hispanic White women. At first glance, this appears to suggest that Black women were less distressed about infertility than non-Hispanic White women. Adding mediators to the model, however, showed that strength of pregnancy intent fully mediates the association. Thus, the relationship between race/ethnicity and fertility-specific distress disappeared when we take into account that Black women were less likely than White women to think of themselves as trying to become pregnant at the time of their infertility episode.
From a theoretical point of view, these findings were consistent with the idea, drawn from identity theory, that fertility-specific distress— as a form of identity disruption—should vary with the size of the gap between present circumstances and a desired state. These findings also have important practical implications for policy makers, medical professionals, psychologists, and other health-care professionals working with women with infertility. This study shows that all women—regardless of race/ethnicity and socioeconomic status—who find that infertility prevents them from achieving goals to which they are strongly committed may suffer from fertility-specific distress. Because Black and Hispanic women are likely to have lower socioeconomic status than White women, they may have reduced access to many fertility services. Yet, adjusting for degree of intentions, fertility-specific distress was similar among the four groups of women. Simply comparing fertility-specific distress by race/ethnicity would be misleading because it would suggest that Black women are less distressed than White women about infertility.
Due to its cross-sectional design, this study does not allow us to make claims about causality. Longitudinal data would allow a fuller elucidation of the ways in which fertility intentions are related to fertility-specific distress. In addition, our sample included all women who ever had an episode of infertility; thus, some women were reporting on events that occurred several years before the interview. The women’s recollections about the strength of their pregnancy intentions in the past may not be accurate. Finally, some central concepts referred to the past while others referred to the present. For example, fertility-specific distress was measured at the time of the interview even though the infertility episode may have been in the past. There is no reason to suspect that these timing issues are different for different subgroups; it is therefore unlikely that these issues had a substantial impact on the main findings. Furthermore, an analysis not reported here indicated that time since infertility episode is not associated with levels of fertility-specific distress.
The measure of commitment to motherhood identity used here referred to strength of intention to become pregnant. It would have been desirable to use a more general measure of commitment to the motherhood identity. Unfortunately, preliminary analyses indicated that the general items measuring importance of motherhood were not consistent across racial groups. Classifying women into one of four racial groups obscured the fact that these broad classifications contained heterogeneous subgroups. Sample-size limitations prevented us from conducting a more detailed analysis of racial/ethnic groups. Future research should include more details on immigration experiences and specific ethnic groups to more fully understand variations in the experiences of infertility. Studying subgroup differences in men’s experiences of infertility will also provide valuable information.
This study provided an initial step toward systematically comparing fertility-specific distress among various racial/ethnic groups using a probability-based sample. Finding that Hispanic women do not differ from non-Hispanic White women and that Black women have lower fertility-specific distress than non-Hispanic White women only because of differences in the strength of pregnancy intentions provided valuable new insights into race/ethnicity and the experience of infertility. It is our hope that our work will inspire additional research on the experience of infertility among subgroups of women.
Acknowledgments
Funding
This study was supported by a grant from NICHD [R01-HD044144 “Infertility: Pathways and Psychosocial Outcomes” (Lynn White and David Johnson, Co-PIs)].
References
- Abbey A, Andrews FM and Halman LJ (1992) Psychosocial, treatment, and demographic predictors of the stress associated with infertility. Fertility and Sterility 57(1): 122–128. [DOI] [PubMed] [Google Scholar]
- Allison PD (2002) Missing Data. Thousand Oaks, CA: SAGE. [Google Scholar]
- American Society for Reproductive Medicine (2008) Definitions of infertility and recurrent pregnancy loss. Fertility and Sterility 90(Suppl. 3): S60. [DOI] [PubMed] [Google Scholar]
- Becker G (2000) The Elusive Embryo: How Women and Men Approach New Reproductive Technologies. Berkeley, CA: University of California Press. [Google Scholar]
- Becker G, Castrillo M, Jackson R, et al. (2005) Infertility among low-income Latinos. Fertility and Sterility 85(4): 882–887. [DOI] [PubMed] [Google Scholar]
- Bengston VL (2001) Beyond the nuclear family: The increasing importance of multigenerational bonds. Journal of Marriage and the Family 63(1): 1–16. [Google Scholar]
- Bitler M and Schmidt L (2006) Health disparities and infertility: Impacts of state level mandates. Fertility and Sterility 85(4): 858–864. [DOI] [PubMed] [Google Scholar]
- Burke PJ (1991) Identity processes and social stress. American Sociological Review 56(6): 836–849. [Google Scholar]
- Burke PJ and Stets JE (2009) Identity Theory. Oxford: Oxford University Press. [Google Scholar]
- Ceballo R, Graham ET and Hart J (2012) “A White thing”: Stereotypes and the experience of infertility among African American women. Paper presented at the annual meeting of the American Psychological Association, Orlando, FL, 3 August. [Google Scholar]
- Chandra A and Stephen EH (2006) Declining estimates of infertility in the United States: 1982– 2002. Fertility and Sterility 86(3): 516–523. [DOI] [PubMed] [Google Scholar]
- Chandra A and Stephen EH (2010) Infertility service use among U.S. women: 1995 and 2002. Fertility and Sterility 93(3): 725–736. [DOI] [PubMed] [Google Scholar]
- Culley LA, Hudson N and van Rooij F (eds) (2009) Marginalized Reproduction: Ethnicity, Infertility, and Reproductive Technologies. London: Earthscan. [Google Scholar]
- Dunlap E, Sturzenhofecker G and Johnson B (2006) The elusive romance of motherhood: Drugs, gender and reproduction in inner-city distressed households. Journal of Ethnicity in Substance Abuse 5(3): 1–27. [DOI] [PubMed] [Google Scholar]
- Epstein YM and Rosenberg HS (2005) Depression in primary versus secondary infertility egg recipients. Fertility and Sterility 83(6): 1882–1884. [DOI] [PubMed] [Google Scholar]
- Exley C and Letherby G (2001) Managing a disrupted lifecourse: Issues of identity and emotion work. Health: An Interdisciplinary Journal for the Social Study of Health, Illness and Medicine 5: 112–132. [Google Scholar]
- Greil AL and McQuillan J (2004) Help-seeking patterns among infertile women. Journal of Reproductive and Infant Psychology 22(4): 305–319. [Google Scholar]
- Greil AL, Johnson KM, McQuillan J, et al. (2010a) Are prior pregnancy outcomes relevant for models of fertility-specific distress or infertility helpseeking? Human Fertility 14(3): 160–166. [DOI] [PubMed] [Google Scholar]
- Greil AL, McQuillan J, Johnson KM, et al. (2009) The hidden infertile: Infertile women without pregnancy intent in the United States. Fertility and Sterility 93(6): 2080–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greil AL, McQuillan J, Shreffler KM, et al. (2011a) Race-ethnicity and medical services for infertility: Stratified reproduction in a population-based sample of U.S. women. Journal of Health and Social Behavior 52(4): 493–507. [DOI] [PubMed] [Google Scholar]
- Greil AL, Shreffler KM, Schmidt L, et al. (2011b) Variation in distress among women with infertility: Evidence from a population-based sample. Human Reproduction 26(8): 2101–2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greil AL, Slauson-Blevins KS and McQuillan J (2010b) The experience of infertility: A review of recent literature. Sociology of Health & Illness 32(1): 140–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning K and Strauss B (2002) Psychological and Psychosomatic Aspects of Involuntary Childlessness: State of Research at the End of the 1990’s. 2002. Ashland, OH: Hogrefe & Huber. [Google Scholar]
- Hjelmstedt A, Andersson L, Skoog-Svanberg A, et al. (1999) Gender differences in psychological reactions to infertility among couples seeking IVF- and ICSI-treatment. Acta Obstetricia et Gynecologica Scandinavica 78(1): 42–48. [PubMed] [Google Scholar]
- Inhorn MC, Ceballo R and Nachtigall R (2009) Marginalized, invisible, and unwanted: American minority struggles with infertility and assisted conception In: Culley L, Hudson N and van Rooij R (eds) Marginalized Reproduction: Ethnicity, Infertility, and Reproductive Technologies. London: Earthscan, pp. 181–197. [Google Scholar]
- Jacob MC, McQuillan J and Greil AL (2007) Psychological distress by type of fertility barrier. Human Reproduction 22(3): 885–894. [DOI] [PubMed] [Google Scholar]
- Johansson M and Berg M (2005) Women’s experiences of childlessness 2 years after the end of in vitro fertilization treatment. Scandinavian Journal of Caring Sciences 19(1): 58–63. [DOI] [PubMed] [Google Scholar]
- Kendall C, Afable-Munsuz A, Speize I, Avery A, et al. (2005) Understanding pregnancy in a population of inner-city women in New Orleans: Results of qualitative research. Social Science & Medicine 60(2): 297–311. [DOI] [PubMed] [Google Scholar]
- Klemetti R, Raitannen J, Sihvo S, et al. (2010) Infertility, mental disorders and well-being— A nationwide survey. Acta Obstetricia et Gynecologica Scandinavica 89(5): 677–682. [DOI] [PubMed] [Google Scholar]
- McCarty C, House M, Harman J, et al. (2006) Effort in phone survey response rates: The effects of vendor and client-controlled factors. Field Methods 18(2): 172–188. [Google Scholar]
- McQuillan J, Bedrous A, Clark A, et al. (2012) Motherhoods and meanings among Black. Hispanic, Asian, and White Women in the United States. Presented at the annual meeting of the Eastern Sociological Society, 25 February. [Google Scholar]
- McQuillan J, Greil AL and Shreffler KM (2011) Pregnancy intentions among women who do not try: Focusing on women who are okay either way. Maternal and Child Health Journal 15(2): 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuillan J, Greil AL, Shreffler KM, et al. (2008) The importance of motherhood among women in the contemporary United States. Gender & Society 22(4): 477–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuillan J, Greil AL, White L, et al. (2003) Frustrated fertility: Infertility and psychological distress among women. Journal of Marriage & Family 65(4): 1007–1018. [Google Scholar]
- Mathews TJ and Hamilton BE (2009) Delayed childbearing: More women are having their first child later in life. NCHS Data Brief 29: 1–8. [PubMed] [Google Scholar]
- Matthews R and Martin-Matthews A (1986) Infertility and involuntary childlessness: The transition to non-parenthood. Journal of Marriage and the Family 48(3): 641–649. [Google Scholar]
- Roberts D (1997) Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York: Vintage Books. [DOI] [PubMed] [Google Scholar]
- Schmidt L (2009) Social and psychological consequences of infertility and assisted reproduction—What are the research priorities? Human Fertility 12(1): 14–20. [DOI] [PubMed] [Google Scholar]
- Sexton MB, Byrd MR and von Kluge S (2010) Measuring resilience in women experiencing infertility using the CD-RISC: Examining infertility-related stress, general distress, and coping styles. Journal of Psychiatric Research 44(4): 236–241. [DOI] [PubMed] [Google Scholar]
- Skogrand L, Barrios-Bell A and Higginbotham B (2009) Stepfamily education for Latino families: Implications for practice. Journal of Couple & Relationship Therapy 8(2): 113–128. [Google Scholar]
- Stryker S (1980) Symbolic Interactionism: A Social Structural Version. Menlo Park, CA: Benjamin/ Cummings. [Google Scholar]
- Szkupinski-Quiroga S (2002) Disrupted Bodies: The Effect of Infertility on Racialized Identities. Unpublished doctoral dissertation, University of California, San Francisco and Berkeley, CA. [Google Scholar]
- Szkupinski-Quiroga S (2007) Blood is thicker than water: Policing donor insemination and the reproduction of Whiteness. Hypatia 22(2): 143–161. [Google Scholar]
- US Census Bureau (2011) 2011 Statistical abstract. Available at: http://www.census.gov/compendia/statab/cats/income_expenditures_poverty_wealth/household_income.html (accessed January 2011).
- Verhaak CM, Smeenk JMJ, Evers AWM, et al. (2007) Women’s emotional adjustment to IVF: A systematic review of 25 years of research. Human Reproduction Update 13(1): 27–36. [DOI] [PubMed] [Google Scholar]
- White L, McQuillan J, Greil AL, et al. (2006) Infertility: Testing a helpseeking model. Social Science & Medicine 62(4): 1031–1041. [DOI] [PubMed] [Google Scholar]