Abstract
Introduction
Currently, the debate on the usefulness of Neutrophil to Lymphocyte Ratio (NLR) as a predictor of complications in acute diverticulitis (AD) remains open, especially, the relation to the severity of the disease, the clinical impact, and the necessity of minimally invasive or emergency surgical procedures. On the other hand, its diagnostic efficacy has not been studied even in our field. The objective of the present study was to determine the utility and diagnostic precision of NLR in complicated acute diverticulitis (cAD).
Methods
Descriptive, retrospective cohort and analytical study. Patients older than 18 years with a diagnosis of AD were included, from 2013 to 2018. Demographic variables, days of hospitalization, leukocyte count, neutrophils, lymphocytes, ESR, CRP, and NLR were analyzed. The sensitivity and specificity for the diagnosis of cAD were determined using ROC curves.
Results
325 patients were included. Of these 196 (60%) were men. The median age was 52 years. A total of 30 (9%) were categorized as cAD. The patients with cAD presented mean values in the leukocyte count (14.02 ± 4.49 × 109/l; p < 0.01), CRP (119.60 ± 87.67; p < 0.01) and NLR (7.61 ± 4.03; p < 0.01). An NLR cutoff value ≥ 4.2 was identified as the most appropriate to distinguish cAD, with a sensitivity of 80%, a specificity of 64%, NPV of 96%, and PPV of 18%.
Conclusion
NLR is a predictive marker of cAD, with a cut-off point of 4.2 being the best diagnostic approach.
Keywords: Acute diverticulitis, Neutrophil-to-lymphocyte ratio, C-reactive protein, Biomarkers
Highlights
-
•
About 10–15% of patients with acute diverticulitis (AD) can develop complications.
-
•
The neutrophil-lymphocyte ratio (NLR) is a useful biomarker in predicting of severity of AD.
-
•
The purpose was to determine the usefulness and diagnostic accuracy of NLR in complicated acute diverticulitis (cAD).
-
•
An NLR cutoff value ≥ 4.2 was identified as the most appropriate to distinguish cAD.
1. Introduction
Acute diverticulitis (AD) is present in 10–25% of patients with diverticular disease, being most common in the sigmoid colon, with around 200.000 hospitalizations yearly [1]. As much as one-fifth of patients are younger than 50 at the moment of diagnosis and around 5% under the age of 40 [2].
Confirming the diagnosis requires the utilization of imaging studies, therefore, the American Society of Colon and Rectal Surgeons (ASCRS) established that computed tomography (CT) is the standard method for the diagnosis of AD, with a sensitivity of 98% and a specificity of 99% [2,3]. The tomographic findings vary according to the severity of the diverticular disease, which is categorized through a modified Hinchey classification system [4]. Approximately 10–15% of AD patients may develop complications that imply the onset of abscesses, fistulas, stenosis, obstruction, and/or perforation [5].
Recently, interest has been raised in the role of biomarkers in diverticular disease as non-invasive, reliable, inexpensive tools that may help in the early diagnosis of complicated AD, such as C-reactive protein (CRP), a useful marker in the prediction of the level of inflammation and severity of AD [6].
Zahorec et al. identified the neutrophil-lymphocyte ratio (NLR) as an inflammation marker in critical patients, defining it as the absolute neutrophil count divided by the absolute lymphocyte count [7]. Over the last decade, NLR effectiveness has been recognized in various pathologies, both benign and malignant; finding that the levels of neutrophils rise as a part of the inflammatory cascade, whereas lymphocytes diminish during sepsis, making a novel subclinical biomarker with a prognostic value in oncological, cardiovascular and infectious diseases, among others [8]. The NLR may be obtained from the blood count data, which represents a lower cost regarding other known biomarkers [7,8]. It was also demonstrated that high values of NLR are associated with severe abdominal infections and worse outcomes, the reason why it started to be applied as a predictor to evaluate results in surgical patients [9].
Currently, the debate on the usefulness of NLR as a predictor of complications in AD remains open, especially, the relation to the severity of the disease, the clinical impact, and the necessity of minimally invasive or emergency surgical procedures [10].
On the other hand, its diagnostic efficacy has not been studied even in our field. Up until now, there are only four studies published in Ireland [11], Israel [12,13], and South Korea [14]. The purpose of the study was to determine the usefulness and diagnostic accuracy of NLR in complicated acute diverticulitis (cAD).
2. Methods
2.1. Study population
A descriptive, retrospective cohort and analytical study were undertaken. Medical histories and an electronic database from the General Surgery Service were reviewed. All the patients over the age of 18 with AD diagnosis through CT were included, from January 2013 until January 2018 in a University Hospital of Cordoba, Argentina, with third-level reference.
Patients were excluded if they had chronic diseases, susceptible to modify the immune-inflammatory response, extra-abdominal infections, immunosuppression, and neoplasias, and those who supplied incomplete data in their electronic clinical histories.
This study was exempted from approval and informed consent by the Institutional Review Board of the Clínica Universitaria Reina Fabiola and was registered with ClinicalTrials.gov (NCT04663490) which can be found via the following link: https://clinicaltrials.gov/show/NCT04663490. The research has been reported in line with the STROCSS [15].
2.2. Study of variables
Demographic variables (sex and age), days of inpatient stay, level of severity in the diverticular process (objectified by CT) were analyzed. It was recorded the value of serum leukocyte, neutrophil, and lymphocyte concentration, Erythrocyte Sedimentation Rate (ESR), CRP, and NLR at the moment of consultation on call.
2.3. Variable definition
NLR: It can be obtained from the blood count (the absolute neutrophil count divided by the absolute lymphocyte count).
CRP: normal value under 5 mg/dL.
2.4. Statistical analysis
The categorical variables were expressed as frequency (percentage), the continuous variables as mean value (standard deviation, SD) or median (range) according to the distribution of data; Mann Whitney test was used to compare the continuous variables, Chi-square and Fisher's tests were used to compare categorical variables among patients with simple acute diverticulitis (sAD) and cAD. A value of p < 0.05 was considered statistically significant.
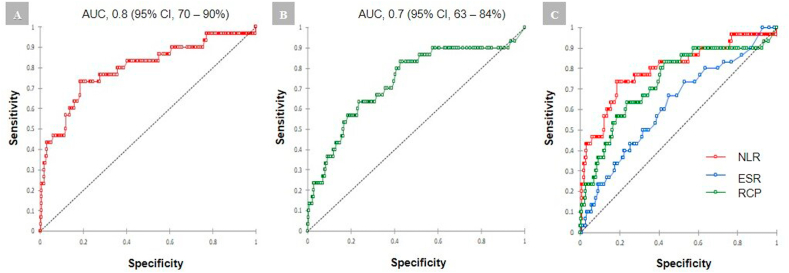
ROC (Receiver Operating Characteristic) curves were used as diagnostic tests to evaluate the diagnostic accuracy of NLR as a predictor of complicated AD, determining sensitivity (Se), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV). Youden index was used to find the cut-off point with the best diagnostic yield for NLR in cAD. SPSS 26 software and GraphPad 7 software was used for statistical analysis.
3. Results
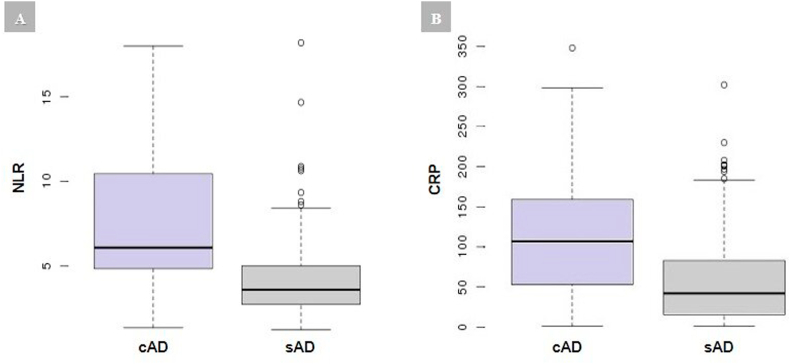
Out of 350 total patients diagnosed with AD, 25 were excluded (8 due to lack of CT, 8 oncological patients, and 9 due to incomplete clinical histories). Three hundred and twenty-five patients were included, 60% of these (n = 196) were male, with a median age of 52 years (range: 25–92). The time of evolution from the onset of symptoms to the consultation had a median of 48 ± 32.94 h. Ninety-one percent (n = 295) were categorized as sAD and 9% (n = 30) presented cAD. Seventy-three percent (n = 236) of patients were hospitalized, the rest of them were treated on an outpatient basis. The median length of hospital stay was greater in cAD (6.60 vs 2.16; p < 0.01) (Table 1). Patients with cAD presented significant values in the median of leukocyte count (14.02 vs 11.93 × 109/L; p < 0.01), neutrophil count (81.37 vs 72.37%; p < 0.01) and lymphocyte count (13.9 vs 20.83%; p < 0.01) (Fig. 1). Concerning the biomarkers in cAD, the mean number was twice as high in CRP (119.60 vs 56.36; p < 0.01) and in NLR (7.61 vs 4.04; p < 0.01). No difference was found in ESR of cAD and sAD (Fig. 2). When evaluating the diagnostic accuracy of NLR, a cutoff value of 4.2 was found (AUC = 0.8; CI 95% = 70–90) as the most appropriate to distinguish complicated acute diverticulitis (Fig. 3). To predict severity, Se of 80% (CI 95% = 58–70), Sp of 64% (95% CI = 58–70), NPV of 96% and PPV of 19% were obtained. Table 2 shows the cutoff points for NLR.
Table 1.
Demographic and clinical characteristics of the patients.
| Characteristic | cAD (n = 30) |
sAD (n = 295) |
p |
|---|---|---|---|
| Sex: | 0.31 | ||
| Male | 50 (50%) | 181 (61%) | |
| Female | 50 (50%) | 114 (39%) | |
| Age (years) | 56 (40–80) | 51 (25–92) | 0.25 |
| BMI (Kg / m2) | 30.7 (28.5–33.5) | 28.3 (26.4–31.2) | 0.21 |
| Onset of symptoms until consultation (Hours) | 8 (2–96) | 48 (4–96) | <0.01 |
| Hinchey: | <0.01 | ||
| Stage IA | 0 (0%) | 295 (100%) | |
| Stage IB | 10 (33.3%) | 0 (0%) | |
| Stage II | 6 (20%) | 0 (0%) | |
| Stage III | 11 (3.7%) | 0 (0%) | |
| Stage IV | 3 (10%) | 0 (0%) | |
| Outpatient / hospital management: | <0.01 | ||
| Interned | 30 (9.2%) | 206 (63.7%) | |
| Ambulatory | 0 (0) | 89 (27.1%) | |
| Hospitalization (days) | 6.5 (4–10) | 3 (0–6) | <0.01 |
| Treatment: | <0.01 | ||
| Medical (Diet + AB) | 11 (36.7%) | 295 (100%) | |
| Percutaneous Drainage + AB | 5 (16.7%) | 0 (0%) | |
| Surgery | 14 (46.6%) | 0 (0%) | |
| Follow – up time (months) | 32 (28.2–37.4) | 28 (24.3–33.1) | 0.22 |
Data are expressed as median with percentiles (25 and 75) or n (%).
sAD, simple acute diverticulitis; cAD, complicated acute diverticulitis; AB, antibiotics. Significant associations are indicated in bold text.
Fig. 1.
cAD (Complicated acute diverticulitis, light gray box) vs sAD (Simple acute diverticulitis, dark gray box). A: white blood cell count. B: neutrophil count. C: lymphocyte count.
Fig. 2.
cAD (Complicated acute diverticulitis, light gray box) vs sAD (Simple acute diverticulitis, dark gray box). A: Neutrophil to lymphocyte ratio (NLR). B: C - reactive protein (CRP).
Fig. 3.
ROC curves to determine the sensitivity (true positives) and specificity (true negatives) for the diagnosis of cAD. A: ROC curve for NLR. B: ROC curve for CRP. C: ROC curve for NLR, CRP, and ESR.
Table 2.
Cut-off points for the neutrophil to lymphocyte ratio.
| NLR | Se | Sp | PPV | NPV | LR+ | LR- |
|---|---|---|---|---|---|---|
| 3.4 | 83% | 45% | 13% | 96% | 1.52 | 0.37 |
| 3.8 | 83% | 55% | 16% | 97% | 1.86 | 0.30 |
| 4.2 | 80% | 65% | 19% | 97% | 2.25 | 0.31 |
| 4.6 | 77% | 71% | 21% | 97% | 2.26 | 0.33 |
| 5.0 | 73% | 76% | 23% | 97% | 3.01 | 0.35 |
| 5.4 | 73% | 82% | 29% | 97% | 4.01 | 0.33 |
| 5.8 | 60% | 85% | 30% | 96% | 4.12 | 0.47 |
NLR, neutrophil-lymphocyte ratio; Se, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value; LR +, positive probability index; LR -, negative probability index. Values selected as predictors of complication are indicated with bold text.
NLR showed statistical significance regarding the requirement of any procedure (percutaneous drainage or surgery), with a median of 9.67 (2.69–18); p < 0.01 (Table 3).
Table 3.
Characteristics of patients with cAD requiring invasive procedures.
| Characteristic | cAD (n = 30) | Hospitalization (days) |
|---|---|---|
| Percutaneous drainage | 5 (17%) | 6 (5–8) |
| Open (Hartmann) | 7 (23%) | 8 (4–10) |
| Laparoscopy: | 7 (23%) | |
| Peritoneal lavage and drainage | 2 (29%) | 7,5 (7–8) |
| ARP with a protective ostomy | 3 (42%) | 7 (6–9) |
| ARP without a protective ostomy | 2 (29%) | 6,5 (6–7) |
Data are expressed as median with percentiles (25 and 75) or n (%).
cAD, complicated acute diverticulitis; ARP, primary resection anastomosis.
Out of the total patients who presented a NLR value < 4.2 (n = 193), only 3.1% (n = 6) required a CT in the case of cAD; that is to say, 96.9% had an unnecessary CT. From these, only half (n = 3) presented cAD with poor evolution.
4. Discussion
Currently, few works make it possible to determine the role of NLR in complicated acute diverticulitis. NLR has been identified as a reliable predictor of adverse outcomes in many benign and malignant diseases, such as heart disease, esophageal cancer, colorectal cancer, and hepatocellular carcinoma.
Neutrophils and lymphocytes have demonstrated to show a better immune response than the total leukocyte count [16].
In our series, 9% (n = 30) of patients presented with complications, similar to the data reported by Bharucha A et al. who studied 3222 patients for over 27 years, finding that 12% (n = 386) were categorized as cAD with one or more complications. Being the most frequent boil or abscess followed by peritonitis, obstruction, and fistula [17].
Patients with cAD had a leukocyte count mean of 14.0 × 109/L ± 4.4; p < 0.01, an expected value which has been demonstrated in the literature [11].
CRP value also showed a significant difference between cAD vs sAD (119.60 vs 56.36; p < 0.01). Its best yield was found with a cutoff value of 55 (AUC = 0.7; CI 95% = 63–84) observing a Se: 70% and a Sp: 62%.
About NLR value, the difference between cAD and sAD was almost twice as high (7.61 vs 4.04; p < 0.01). Most existing studies that evaluated the usefulness of NLR as a predictor marker of severity used a cutoff point ≥5 to determine adverse outcomes, both in benign and malignant diseases [16].
In this research, it was demonstrated that a cutoff point of 4.2 has a Se: 80%, Sp: 64.1%, NPV: 96% and PPV: 18%.
These results are similar to those published by Reynolds I et al. who found a value of NLR >5.34 (Se: 90.48%, Sp: 55%), with the best diagnostic yield to define severity in a cohort prospective of 101 patients with AD, with a high predictive value for the necessity of minimally invasive procedures (percutaneous drainage) or emergency surgical procedure [10]. They also found that NLR had lower accuracy than CRP and leukocyte count for diagnosing complications.
In another retrospective cohort study of 225 patients admitted with AD, Mari A et al. compared NLR and platelet count, to determine the correlation of CAD and Hinchey classification, showing that a cutoff point >6.68 presented a Se: 68.75% and Sp:79.21% [13]; thus NLR presented a higher yield as a diagnostic test in cAD, but lower sensitivity than reported in this study.
The most recent work made by Zager et al. (2020) was a retrospective cohort that included 456 patients whit a median follow-up of 64.3 months show that high levels of NLR (>5.4) were associated with shorter intervals between episodes of acute diverticulitis, likewise to a higher number of readmissions, with longer hospital stay; this is similar to our population of the study, where the NLR value was found to be directly related to the onset of symptoms. In most patients with recurrent episodes of acute diverticulitis, biomarkers were elevated both in the first episode and in recurrent attacks. This suggests that NLR might be related to an inflammatory load [12].
Concerning computed tomography, it continues to be the gold standard for the diagnosis of AD, representing a cost of US $ 115 for each CT performed. Considering the analysis of NLR for the severity of the diverticular process, it is possible to say that 187 CT wouldn't have been necessary having been identified as Ads, with an additional cost of US $ 21.505. On the contrary, the cost of NLR is US $ 4 per patient that means the US $ 1300 for all the population studied, which clearly shows its elevated cost-effectiveness.
The above-mentioned studies about the association of NLR in acute diverticulitis were performed in populations of Europe and Asia. We found no references for its application in our environment. We consider that NLR meets many of the criteria for the ideal biomarker and it is easily obtained from a full hemogram of a blood sample taken routinely during the initial evaluation of the patients attending on-call service. Besides, it implies no additional costs.
Limitations: The retrospective nature of the study and the size of the sample, although it is the second study with the highest number of patients.
Recommendations: To improve and go further the NLR, it is appropriate to perform a prospective randomised study that allows the validation of the test, as well as the comparison of its usefulness with another biomarker as CRP.
5. Conclusion
NLR might help predict complicated acute diverticulitis, being the cutoff point ≥4.2 the one that granted the best diagnostic approximation. The routine application of this simple inexpensive test on-call might facilitate the triage of priorities in urgencies, as well as avoid a tomographic study in low-risk patients selected with compliant clinic and ultrasound. Furthermore, our results validate previous studies in terms of the association between NLR and cAD.
Funding
No source to be stated.
Informed consent
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
No ethical approval sought as anonymized retrospective data.
Sources of funding
No source to be stated.
Author contribution
René M. Palacios Huatuco: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript.
Diana A. Pantoja Pachajoa: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, critical revision of manuscript.
Nicolás Bruera: acquisition of data, analysis and interpretation of data.
Agustín E. Pinsak: acquisition of data, analysis and interpretation of data.
Florencia Llahi: acquisition of data, analysis and interpretation of data.
Alejandro M. Doniquian: analysis and interpretation of data, critical revision of manuscript.
Fernando A. Alvarez: study conception and design, analysis and interpretation of data, critical revision of manuscript.
Matías Parodi: analysis and interpretation of data, critical revision of manuscript.
Registration of research studies
1Name of the registry: Neutrophil to Lymphocyte Ratio as a Predictor of Complicated Acute Diverticulitis.
2Unique Identifying number or registration ID: NCT04663490.
3Hyperlink to your specific registration (must be publicly accessible and will be checked): https://clinicaltrials.gov/ct2/show/NCT04663490.
Guarantor
René M. Palacios Huatuco: manuelpalacioshuatuco@gmail.com.
Diana A. Pantoja Pachajoa: dianaalejandrapantoja@gmail.com.
Fernando A. Alvarez: fernando.alvarez@hospitalitaliano.org.ar.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2021.01.076.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Weizman A.V., Nguyen G.C. Diverticular disease: epidemiology and management. Can. J. Gastroenterol. 2011 doi: 10.1155/2011/795241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feingold D., Steele S.R., Lee S., Kaiser A., Boushey R., Buie W.D., Rafferty J.F. Practice parameters for the treatment of sigmoid diverticulitis. Dis. Colon Rectum. 2014 doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 3.Barat M., Dohan A., Pautrat K., Boudiaf M., Dautry R., Guerrache Y., Pocard M., Hoeffel C., Eveno C., Soyer P. Acute colonic diverticulitis: an update on clinical classification and management with MDCT correlation. Abdom. Radiol. 2016 doi: 10.1007/s00261-016-0764-1. [DOI] [PubMed] [Google Scholar]
- 4.Wasvary H., Turfah F., Kadro O., Beauregard W. Same hospitalization resection for acute diverticulitis. Am. Surg. 1999 [PubMed] [Google Scholar]
- 5.Bates D.D.B., Fernandez M.B., Ponchiardi C., von Plato M., Teich J.P., Narsule C., Anderson S.W., Gupta A., LeBedis C.A. Surgical management in acute diverticulitis and its association with multi-detector CT, modified Hinchey classification, and clinical parameters. Abdom. Radiol. 2018 doi: 10.1007/s00261-017-1422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Käser S.A., Fankhauser G., Glauser P.M., Toia D., Maurer C.A. Diagnostic value of inflammation markers in predicting perforation in acute sigmoid diverticulitis. World J. Surg. 2010 doi: 10.1007/s00268-010-0726-7. [DOI] [PubMed] [Google Scholar]
- 7.Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Lek. Listy. 2001 [PubMed] [Google Scholar]
- 8.Zahorec R. Neutrophil-to-lymphocyte ratio. Sixteen-year-long history since publication of our article in Bratislava Medical Journal. Bratislava Med. J. 2017 doi: 10.4149/BLL_2017_062. [DOI] [PubMed] [Google Scholar]
- 9.Miyamoto R., Inagawa S., Sano N., Tadano S., Adachi S., Yamamoto M. The neutrophil-to-lymphocyte ratio (NLR) predicts short-term and long-term outcomes in gastric cancer patients. Eur. J. Surg. Oncol. 2018 doi: 10.1016/j.ejso.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Reynolds I.S., Heaney R.M., Khan W., Khan I.Z., Waldron R., Barry K. The utility of neutrophil to lymphocyte ratio as a predictor of intervention in acute diverticulitis. Dig. Surg. 2017 doi: 10.1159/000450836. [DOI] [PubMed] [Google Scholar]
- 11.Hogan J., Sehgal R., Murphy D., O'Leary P., Coffey J.C. Do inflammatory indices play a role in distinguishing between uncomplicated and complicated diverticulitis? Dig. Surg. 2016 doi: 10.1159/000447250. [DOI] [PubMed] [Google Scholar]
- 12.Zager Y., Horesh N., Dan A., Aharoni M., Khalilieh S., Cordoba M., Nevler A., Gutman M., Rosin D. Associations of novel inflammatory markers with long-term outcomes and recurrence of diverticulitis. ANZ J. Surg. 2020 doi: 10.1111/ans.16220. [DOI] [PubMed] [Google Scholar]
- 13.Mari A., Khoury T., Lubany A., Safadi M., Farraj M., Farah A., Kadah A., Sbeit W., Mahamid M. Neutrophil-to-Lymphocyte and platelet-to-lymphocyte ratios are correlated with complicated diverticulitis and Hinchey classification: a simple tool to assess disease severity in the emergency department. Emerg. Med. Int. 2019 doi: 10.1155/2019/6321060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang H.S., Cha Y.S., Park K.H., Hwang S.O. Delta neutrophil index as a promising prognostic marker of emergent surgical intervention for acute diverticulitis in the emergency department. PloS One. 2017 doi: 10.1371/journal.pone.0187629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Jeon T.J., Park J.Y. Clinical significance of the neutrophil-lymphocyte ratio as an early predictive marker for adverse outcomes in patients with acute pancreatitis. World J. Gastroenterol. 2017 doi: 10.3748/wjg.v23.i21.3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bharucha A.E., Parthasarathy G., Ditah I., Fletcher J.G., Ewelukwa O., Pendlimari R., Yawn B.P., Melton L.J., Schleck C., Zinsmeister A.R. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am. J. Gastroenterol. 2015 doi: 10.1038/ajg.2015.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.