Abstract
Background
A diverse physician workforce improves the quality of care for all patients, and there is a need for greater diversity in orthopaedic surgery. It is important that medical students of diverse backgrounds be encouraged to pursue the specialty, but to do so, we must understand students’ perceptions of diversity and inclusion in orthopaedics. We also currently lack knowledge about how participation in an orthopaedic clinical rotation might influence these perceptions.
Questions/purposes
(1) How do the perceptions of diversity and inclusion in orthopaedic surgery compare among medical students of different gender identities, races or ethnicities, and sexual orientations? (2) How do perceptions change after an orthopaedic clinical rotation among members of demographic groups who are not the majority in orthopaedics (that is, cis-gender women, underrepresented racial minorities, other racial minorities, and nonheterosexual people)?
Methods
We surveyed students from 27 US medical schools who had completed orthopaedic rotations. We asked about their demographic characteristics, rotation experience, perceptions of diversity and inclusion in orthopaedics, and personal views on specialty choice. Questions were derived from diversity, equity, and inclusion climate surveys used at major academic institutions. Cis-gender men and cis-gender women were defined as those who self-identified their gender as men or women, respectively, and were not transgender. Forty-five percent (59 of 131) of respondents were cis-men and 53% (70 of 131) were cis-women; 49% (64 of 131) were white, 20% (26 of 131) were of underrepresented racial minorities, and 31% (41 of 131) were of other races. Eighty-five percent (112 of 131) of respondents were heterosexual and 15% (19 of 131) reported having another sexual orientation. We compared prerotation and postrotation perceptions of diversity and inclusion between majority and nonmajority demographic groups for each demographic domain (for example, cis-men versus cis-women). We also compared prerotation to postrotation perceptions within each nonmajority demographic group. To identify potential confounding variables, we performed univariate analysis to compare student and rotation characteristics across the demographic groups, assessed using an alpha of 0.05. No potential confounders were identified. Statistical significance was assessed at a Bonferroni-adjusted alpha of 0.0125. Our estimated response percentage was 26%. To determine limitations of nonresponse bias, we compared all early versus late responders and found that for three survey questions, late responders had a more favorable perception of diversity in orthopaedic surgery, whereas for most questions, there was no difference.
Results
Before rotation, cis-women had lower agreement that diversity and inclusion are part of orthopaedic culture (mean score 0.96 ± 0.75) compared with cis-men (1.4 ± 1.1) (mean difference 0.48 [95% confidence interval 0.16 to 0.81]; p = 0.004), viewed orthopaedic surgery as less diverse (cis-women 0.71 ± 0.73 versus cis-men 1.2 ± 0.92; mean difference 0.49 [95% CI 0.20 to 0.78]; p = 0.001) and more sexist (cis-women 1.3 ± 0.92 versus cis-men 1.9 ± 1.2; mean difference 0.61 [95% CI 0.23 to 0.99]; p = 0.002), believed they would have to work harder than others to be valued equally (cis-women 2.8 ± 1.0 versus cis-men 1.9 ± 1.3; mean difference 0.87 [95% CI 0.45 to 1.3]; p < 0.001), and were less likely to pursue orthopaedic surgery (cis-women 1.4 ± 1.4 versus cis-men 2.6 ± 1.1; mean difference 1.2 [95% CI 0.76 to 1.6]; p < 0.001). Before rotation, underrepresented minorities had less agreement that diversity and inclusion are part of orthopaedic surgery culture (0.73 ± 0.72) compared with white students (1.5 ± 0.97) (mean difference 0.72 [95% CI 0.35 to 1.1]; p < 0.001). Many of these differences between nonmajority and majority demographic groups ceased to exist after rotation. Compared with their own prerotation beliefs, after rotation, cis-women believed more that diversity and inclusion are part of orthopaedic surgery culture (prerotation mean score 0.96 ± 0.75 versus postrotation mean score 1.2 ± 0.96; mean difference 0.60 [95% CI 0.22 to 0.98]; p = 0.002) and that orthopaedic surgery is friendlier (prerotation 2.3 ± 1.2 versus postrotation 2.6 ± 1.1; mean difference 0.41 [95% CI 0.14 to 0.69]; p = 0.004), more diverse (prerotation 0.71 ± 0.73 versus postrotation 1.0 ± 0.89; mean difference 0.28 [95% CI 0.08 to 0.49]; p = 0.007), less sexist (prerotation 1.3 ± 0.92 versus postrotation 1.9 ± 1.0; mean difference 0.63 [95% CI 0.40 to 0.85]; p < 0.001), less homophobic (prerotation 2.1 ± 1.0 versus postrotation 2.4 ± 0.97; mean difference 0.27 [95% CI 0.062 to 0.47]; p = 0.011), and less racist (prerotation 2.3 ± 1.1 versus postrotation 2.5 ± 1.1; mean difference 0.28 [95% CI 0.099 to 0.47]; p = 0.003). Compared with before rotation, after rotation cis-women believed less that they would have to work harder than others to be valued equally on the rotation (prerotation 2.8 ± 1.0 versus postrotation 2.5 ± 1.0; mean difference 0.31 [95% CI 0.12 to 0.50]; p = 0.002), as did nonheterosexual students (prerotation 2.4 ± 1.4 versus postrotation 1.8 ± 1.3; mean difference 0.56 [95% 0.21 to 0.91]; p = 0.004). Underrepresented minority students saw orthopaedic surgery as less sexist after rotation compared with before rotation (prerotation 1.5 ± 1.1 versus postrotation 2.0 ± 1.1; mean difference 0.52 [95% CI 0.16 to 0.89]; p = 0.007).
Conclusion
Even with an estimated 26% response percentage, we found that medical students of demographic backgrounds who are not the majority in orthopaedics generally perceived that orthopaedic surgery is less diverse and inclusive than do their counterparts in majority groups, but these views often change after a clinical orthopaedic rotation.
Clinical Relevance
These perceptions may be a barrier to diversification of the pool of medical student applicants to orthopaedics. However, participation in an orthopaedic surgery rotation is associated with mitigation of many of these negative perceptions among diverse students. Medical schools have a responsibility to develop a diverse workforce, and given our findings, schools should promote participation in a clinical orthopaedic rotation. Residency programs and orthopaedic organizations can also increase exposure to the field through the rotation and other means. Doing so may ultimately diversify the orthopaedic surgeon workforce and improve care for all orthopaedic patients.
Introduction
A diverse physician workforce is essential to providing high-quality care for all patients. This occurs in part through the direct patient experience, where, for example, patients seeing race-concordant physicians report more participation in decision-making [14]. Minority physicians may possess greater cultural competence than nonminority physicians when working with patients of like backgrounds [33], and physicians’ cultural sensitivity is essential to caring for diverse patients [24] and is positively correlated with patients’ views of the quality of interaction with their physician [34]. Diversity may also help address disparities in care, which are prevalent in orthopaedic surgery [2, 8, 35], as minority physicians care for a disproportionately high fraction of minority patients as well as those covered by Medicaid or the uninsured [22]. Finally, greater physician diversity may help address the underrepresentation of certain demographic groups in orthopaedic research [33]. Despite these benefits of physician workforce diversity, the need for greater gender and racial diversity in orthopaedics is well documented. [32, 33, 38]. The percentages of women and underrepresented racial and ethnic minorities are low not only among practicing orthopaedic surgeons, but also among residents, especially when compared with the diversity of medical school matriculants (Fig. 1) [3, 4, 11, 31]. In fact, the percentage of women orthopaedic residents is lower than any other surgical or medical specialty, at 15% [11, 31], and racial and ethnic minority representation in orthopaedic residency has decreased in recent years [1, 31]. Data are lacking on the diversity of sexual orientation among orthopaedic surgeons and trainees.
Fig. 1.
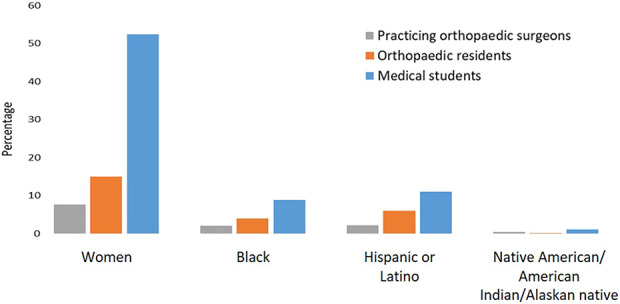
Prevalence of various demographic groups among practicing orthopaedic surgeons [3], orthopaedic residents [11, 31], and medical school matriculants [4].
The low numbers of women and racial and ethnic minorities in orthopaedic residency do not appear to reflect a lower quality of such applicants, but rather too few applicants from these groups [15, 32]. For comparison, orthopaedic applicants are less diverse in gender and race and ethnicity than general surgery applicants [15]. No difference exists between the gender distribution of orthopaedic applicants and that of orthopaedic residents [15], suggesting that women are accepted to residency in comparable proportions to men when women apply. Evidence is mixed as to whether minority applicants are accepted to residency at comparable rates to their white counterparts [15, 32]. Thus, the lack of diversity in orthopaedics is influenced by the low number of residency applicants from nonmajority demographic groups. To address the lack of diversity in orthopaedic surgery, it is imperative that we encourage students of diverse backgrounds to pursue orthopaedics. Doing so will require an understanding of how these students view the level of diversity and inclusion in orthopaedic surgery. It is evident that students of diverse backgrounds place importance on diversity, with studies showing that women applicants place greater importance on program diversity than men [23] and that lower application rates have been attributed to negative perceptions of gender diversity in the field [7, 19]. Women and underrepresented minority students are also more likely to apply to orthopaedics when coming from an institution with greater gender and racial diversity, respectively [29, 30]. Because student participation in musculoskeletal curricula has been shown to influence specialty choice [7, 10, 19, 20, 26], and because many students gain meaningful exposure through a clinical rotation, it is also useful to assess whether participation in an orthopaedic surgery clinical rotation improves perceptions of the level diversity and inclusion among nonmajority students. If so, the rotation may be used as a tool to encourage more students to pursue the specialty.
Therefore, we asked: (1) How do the perceptions of diversity and inclusion in orthopaedic surgery compare among medical students of different gender identities, races or ethnicities, and sexual orientations? (2) How do perceptions change after an orthopaedic clinical rotation among members of demographic groups who are not the majority in orthopaedics (that is, women, underrepresented racial minorities, other racial minorities, and nonheterosexual people)?
Materials and Methods
Survey Administration
After institutional review board exemption was obtained for this study, we developed a 21-item survey (Appendix 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A472) in a secure internet-based platform (REDCap version 9.1.20, Vanderbilt University Medical Center, Nashville, TN, USA).
We distributed the survey to 27 medical schools (24 MD-granting, three DO-granting) across the United States, including public and private, rural and urban, and small and large institutions [12, 36, 37]. Because there is no national repository of medical students completing orthopaedic rotations, we identified these schools based on our professional relationships with them and without knowledge of the orthopaedic rotations they offered. This process of institution identification is similar to that of a previous survey of medical students about their decisions to pursue orthopaedics [20].
Our survey was sent to medical students electronically via colleagues at each institution, and responses were collected between November 22, 2019 and December 20, 2019. Notably, colleagues distributing surveys at the institutions were not necessarily part of the orthopaedic community. To increase response percentage, a reminder notification was sent 1 week after the initial survey distribution. We included medical students in the United States who had completed an orthopaedic clinical rotation within the past 12 months and who were able to complete an English-language, internet-based survey. Students from any medical school year were allowed to participate, provided that they met the eligibility criteria. Although we expected most respondents to be third- and fourth-year students, we recognize that several institutions, including our own, start clinical rotations during the second year, making it highly possible that second-year students would respond. Some students also follow nontraditional pathways to and through medical school, and in rare cases, it is possible that a student who is technically in their first year may have completed an orthopaedic clinical rotation. Respondents were told that survey participation was voluntary, and that completion of the survey would serve as their consent to participate in our study. We described the amount of time needed to complete the survey and the purpose of it, and that responses would be confidential. We stated who the investigator was and provided contact information. We explained that five respondents would be randomly selected to receive a USD 25 gift card. This information was provided in both the survey invitation (Appendix 2; Supplemental Digital Content 2, http://links.lww.com/CORR/A473) as well as the introductory text to the survey itself (Appendix 3; Supplemental Digital Content 3, http://links.lww.com/CORR/A474). Neither adaptive questioning nor randomization of question order was used. Between six and 10 questions were displayed on each page of the survey, over four pages. Questions related to our major objectives required completion, and incomplete surveys were not included in our analysis. Respondents were able to review and change answers. We did not use cookies or track Internet Protocol addresses of survey respondents. Technical functionality was tested within our study group before distribution. Survey design and implementation were guided by the Checklist for Reporting Results of Internet E-Surveys [16, 17].
Survey Topics
We derived survey questions directly from diversity, equity, and inclusion climate surveys used at major academic institutions to maintain validity of the questions asked [16]. Questions were also chosen to be inclusive of multiple realms of diversity and inclusion to increase content validity. Questions on these climate surveys were informed by previous work of steering committees and working groups, which included feedback from students, staff, and faculty [12, 36, 37].
Demographic Characteristics
Respondents indicated their gender identity, race or ethnicity, and sexual orientation [36, 37]. Cis-men and cis-women were those who identified as men or women, respectively, as their gender identity and who did not identify as transgender. In our analysis of gender identity, we omitted data from two students who did not identify as cis-men or cis-women to preserve their anonymity. Our analysis compared three racial/ethnic groups: white, underrepresented racial or ethnic minority (Black, Hispanic or Latino, or Native American or Alaskan Native), and all others. All race and ethnicity options were consistent with those used in previous institutional diversity surveys [36, 37]. Hispanic and Latino, although not a race, was included as an underrepresented racial minority, consistent with previous work [12] and because recent research identified Hispanic and Latino individuals as being underrepresented in orthopaedics [1]. For sexual orientation [36, 37], we compared respondents who identified as heterosexual with all others. Respondents provided data on their year in medical school and the geographic region of their medical school [39].
We received complete surveys from 131 medical students. Of these, 45% (59 of 131) of respondents identified as cis-men and 53% (70 of 131) as cis-women; 49% (64 of 131) identified as white, 20% (26 of 131) identified as an underrepresented racial minority, and 31% (41 of 131) identified as another race; and 85% (112 of 131) identified as heterosexual and 15% (19 of 131) identified as having another sexual orientation.
Characteristics of Orthopaedic Clinical Rotations
Respondents reported the length of time since they completed their first orthopaedic rotation, the duration of the rotation, and US geographic region where the rotation occurred [39]. We aimed to include regional diversity of rotations because the proportion of women who are orthopaedic surgeons varies geographically [13].
Perceptions of Diversity and Inclusion in Orthopaedics
Respondents used a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) to indicate how they viewed the following two items before and after their rotation: Whether they believed that diversity and inclusion were part of orthopaedic surgery culture and whether they would need to work harder than others to be valued equally in their rotation. Respondents used a scale ranging from 0 to 5 to rate how they viewed orthopaedic surgery before and after their rotation according to the following descriptor pairs: hostile versus friendly, homogenous versus diverse, sexist versus non-sexist, homophobic versus non-homophobic, and racist versus nonracist.
Personal Views on Specialty Choice
Respondents used a 5-point scale ranging from 1 (very unlikely) to 5 (very likely) to indicate, before and after their rotation, how likely they were to pursue a career in orthopaedic surgery. They used a 5-point scale ranging from 1 (very unimportant) to 5 (very important) to indicate, before and after rotation, the importance of a specialty’s diversity in their choice of specialty. Respondents were asked whether they could identify a career mentor in orthopaedic surgery after their rotation.
Response Percentage
We were unable to calculate a precise response percentage because the exact number of students completing an orthopaedic surgery rotation at each medical school for the duration of the study eligibility period was unknown. However, we calculated an estimated response percentage of 26% based on the number of respondents to our survey, the average percentage of students completing an orthopaedic surgery rotation at our institution, and extrapolating this percentage to the class sizes at the institutions included in our survey with an orthopaedic surgery department [5]. To assess the nonresponse bias, we compared the responses of early versus late respondents, with the assumption that those who responded later were more similar to nonrespondents compared with those who responded earlier [21]. Early respondents were defined as those who responded within the first week of survey distribution, whereas late respondents were those who responded in the last 3 weeks of survey distribution. For this comparison, we used t-tests to compare the mean prerotation and postrotation rating score for all early responses versus all late respondents, for each survey question. Significance was assessed at an alpha of 0.05. We found that for three survey questions (likelihood of pursing orthopaedic surgery, homophobic versus nonhomophobic nature of field, and racist versus nonracist nature of field), late responders had a more favorable perception of diversity in orthopaedic surgery, whereas for the remainder of questions, there was no difference between early and late respondents (Appendix 4; Supplemental Digital Content 4, http://links.lww.com/CORR/A475).
Statistical Analysis
We compared respondent demographic and clinical rotation characteristics across gender identity, racial and ethnic, and sexual orientation groups using chi-square goodness-of-fit and Fisher exact tests for categorical variables and one-way ANOVA for quantitative variables. To identify potential confounding variables, we used univariate analysis to compare student and rotation characteristics across demographic groups, including year in medical school, medical school region, orthopaedic rotation region, rotation length, and time since completion of rotation. Significance for inclusion of confounders was assessed at an alpha of 0.05. We found no differences in these baseline characteristics across the groups, and thus did not incorporate these variables in our final analyses (Appendix 5; Supplemental Digital Content 5, http://links.lww.com/CORR/A476).
The mean scores for perceptions of diversity and inclusion in orthopaedics and personal views on specialty choice before and after rotation were described for the overall cohort, as well as for the gender identity, race and ethnicity, and sexual orientation groups (Appendix 6; Supplemental Digital Content 6, http://links.lww.com/CORR/A477). We used t-tests to compare the mean rating scores between the majority and nonmajority groups for each demographic domain (that is, men versus women, white versus underrepresented racial minority, white versus other race or ethnicity, and heterosexual versus nonheterosexual) (Appendix 6). Within each nonmajority demographic group (that is, cis-women, underrepresented racial minority, and nonheterosexual), we compared prerotation scores with postrotation scores using paired t-tests. For the ability to find a mentor, we compared proportions of respondents answering yes between the majority and nonmajority groups for each diversity category using chi-square goodness-of-fit (Appendix 6). Logistic regression analysis was used to assess whether a respondent’s gender, race or ethnicity, or sexual orientation was associated with prerotation to postrotation improvement in perceptions of diversity and inclusion in orthopaedics, as well as personal views about specialty choice, compared with the majority demographic for each demographic domain as a baseline. Because no potential confounders were found in the baseline comparison of student and rotation characteristics across diversity groups, none were included in these regression models.
To assess significance, we used Bonferroni adjustment for multiple comparisons [9]. For each survey question, a maximum experiment-wise error rate (MEER) α of 0.05 was used. In assessing comparison of prerotation scores between demographic groups, each comparison was treated as an independent hypothesis (for example, cis-male versus cis-female or white versus underrepresented racial minority) for a total of four independent hypotheses. Thus, each test comparing prerotation scores across demographic groups was considered statistically significant if p values were less than the MEER α divided by four, or 0.0125. This same approach was taken in comparing postrotation scores between demographic groups. In assessing the change in prerotation versus postrotation within each nonmajority demographic group, the comparison within each nonmajority demographic group was considered an independent hypothesis (such as, pre- versus postrotation in cis-women or pre- versus postrotation in underrepresented racial minority). Thus, in comparing prerotation versus postrotation scores within each nonmajority demographic group, each test result was considered statistically significant if p values were less than MEER α divided by four, or 0.0125. We took the same approach in assessing the significance of the logistic regression models, which assessed whether nonmajority demographic status was associated with higher likelihood of improvement in perceptions. Although we performed Bonferroni adjustment for multiple comparisons, it should be noted that this approach results in a stringent threshold when assessing significance. This allows for a more rigorous assessment of significance, but there may be some associations that are significant at alpha equal to 0.05 but not our Bonferroni-adjusted alpha, which may warrant further exploration.
Data were stored on the REDCap platform and analyzed using R software, version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Diversity and Inclusion Perceptions by Demographic Group, Before and After Rotation
Nonmajority demographic groups had worse perceptions of the level of diversity and inclusion in orthopaedic surgery before the rotation compared with majority demographic groups, with many of these differences ceasing to exist postrotation. Before the orthopaedic rotation, cis-women had worse perceptions compared with cis-men. This included lower agreement with the statement that diversity and inclusion are part of orthopaedic culture (mean score 0.96 ± 0.75) compared with cis-men (1.4 ± 1.1; mean difference 0.48 [95% confidence interval 0.16 to 0.81]; p = 0.004) (Fig. 2A), view of orthopaedic surgery as less diverse (cis-women 0.71 ± 0.73 versus cis-men 1.2 ± 0.92; mean difference 0.49 [95% CI 0.20 to 0.78]; p = 0.001) (Fig. 2B), and view of orthopaedic surgery as more sexist (cis-women 1.3 ± 0.92 versus cis-men 1.9 ± 1.2; mean difference 0.61 [95% CI 0.23 to 0.99]; p = 0.002) (Fig. 2C). These differences between cis-men and cis-women ceased to exist in comparison of postrotation scores. Prerotation, cis-women more strongly agreed that they would have to work harder than others to be valued equally on their rotation (2.8 ± 1.0) compared with cis-men (1.9 ± 1.3; mean difference 0.87 [95% CI 0.45 to 1.3]; p < 0.001) (Fig. 2D). This difference persisted in comparison of postrotation scores, where cis-women showed higher agreement with this sentiment (2.5 ± 1.0) than cis-men (2.0 ± 1.3; mean difference 0.54 [95% CI 0.12 to 0.95]; p = 0.0117) (Fig. 2D). Cis-women prerotation were less likely to pursue orthopaedic surgery (1.4 ± 1.4) compared with cis-men (2.6 ± 1.1; mean difference 1.2 [95% CI 0.76 to 1.6]; p < 0.001) (Fig. 2E). This difference persisted, with cis-women less likely to pursue orthopaedic surgery postrotation (1.6 ± 1.6) compared with cis-men (2.5 ± 1.5; mean difference 0.91 [95% CI 0.36 to 1.5]; p = 0.001) (Fig. 2E). Prerotation, underrepresented minorities had less agreement that diversity and inclusion are part of orthopaedic surgery culture (0.73 ± 0.72) compared with white students (1.5 ± 0.97; mean difference 0.72 [95% CI 0.35 to 1.1]; p < 0.001) (Fig. 2A). This difference did not exist postrotation (Fig. 2A). No differences were found between demographic groups on perceptions of friendliness of orthopaedic surgery (Fig. 2F), how homophobic orthopaedic surgery is perceived to be (Fig. 2G), how racist orthopaedic surgery is perceived to be (Fig. 2H), or the importance of diversity in selecting a specialty (Fig. 2I).
Fig. 2.

A-I Perceptions of diversity and inclusion in orthopaedic surgery among various demographic groups before and after a clinical rotation. t-tests were used to compare scores between majority and nonmajority groups for each diversity category (cis-men versus cis-women, white versus underrepresented racial minority, white versus other race/ethnicity, and heterosexual versus nonheterosexual). (A) Prerotation, cis-women and underrepresented racial minorities believed less than cis-men and white students, respectively, that diversity and inclusion are part of orthopaedic surgery culture. (B) Prerotation, cis-women believed that orthopaedic surgery is less diverse than did cis-men. (C) Prerotation, cis-women believed that orthopaedic surgery is more sexist than cis-men. (D) Prerotation and postrotation, cis-women believed they would have to work harder than others to be valued equally on the rotation compared with cis-men. (E) Prerotation and postrotation, cis-women indicated lower likelihood of pursuing orthopaedic surgery compared with cis-men. There were no differences between demographic groups within each diversity category on: (F) friendliness of orthopaedic surgery, (G) how homophobic orthopaedic surgery is perceived to be, (H) how racist orthopaedic surgery is perceived to be, or (I) the importance of diversity in selecting a specialty. aSignificance was assessed at Bonferroni-adjusted α = 0.0125.
Improvement in Perceptions of Diversity and Inclusion Among Nonmajority Groups
Nonmajority demographic groups saw improvement in perceptions of diversity and inclusion in orthopaedic surgery after the rotation. Cis-women believed more after rotation that diversity and inclusion are part of orthopaedic surgery culture (prerotation mean score 0.96 ± 0.75; postrotation mean score 1.2 ± 0.96; mean difference 0.60 [95% CI 0.22 to 0.98]; p = 0.002). Cis-women also reported after their rotation that, compared with prerotation sentiment, orthopaedic surgery is friendlier (prerotation 2.3 ± 1.2 versus postrotation 2.6 ± 1.1; mean difference 0.41 [95% CI 0.14 to 0.69]; p = 0.004), more diverse (prerotation 0.71 ± 0.73 versus postrotation 1.0 ± 0.89; mean difference 0.28 [95% CI 0.08 to 0.49], p = 0.007), less sexist (prerotation 1.3 ± 0.92 versus postrotation 1.9 ± 1.0; mean difference 0.63 [95% CI 0.40 to 0.85]; p < 0.001), less homophobic (prerotation 2.1 ± 1.0 versus postrotation 2.4 ± 0.97; mean difference 0.27 [95% CI 0.062 to 0.47]; p = 0.011), and less racist (prerotation 2.3 ± 1.1 versus postrotation 2.5 ± 1.1; mean difference 0.28 [95% CI 0.099 to 0.47]; p = 0.003). Compared with the prerotation period, postrotation, cis-women believed less that they would have to work harder than others to be valued equally on the rotation (prerotation 2.8 ± 1.0 versus postrotation 2.5 ± 1.0; mean difference 0.31 [95% CI 0.12 to 0.50]; p = 0.002). Cis-women were more likely than cis-men to see improvement in the belief that they would have to work harder than others to be valued equally on the rotation (odds ratio 4.3 [95% CI 1.7 to 13]; p = 0.003). Underrepresented minority students saw orthopaedic surgery as less sexist after their rotation compared with before it (prerotation 1.5 ± 1.1 versus postrotation 2.0 ± 1.1; mean difference 0.52 [95% CI 0.16 to 0.89]; p = 0.007). Students of other race groups (nonwhite and non-underrepresented minority) believed more after rotation that diversity and inclusion are part of orthopaedic surgery culture (prerotation 1.1 ± 0.99 versus postrotation 1.5 ± 1.1; mean difference 0.31 [95% CI 0.07 to 0.54]; p = 0.012) and that orthopaedic surgery is less sexist postrotation than prerotation (prerotation 1.5 ± 1.2 versus postrotation 2.0 ± 1.1; mean difference 0.47 [95% CI 0.22 to 0.72]; p < 0.001). Finally, nonheterosexual students were less likely to believe that they would have to work harder than others to be valued equally on their rotation after their rotation compared with prerotation (prerotation 2.4 ± 1.4 versus postrotation 1.8 ± 1.3; mean difference 0.56 [95% CI 0.21 to 0.91]; p = 0.004).
Discussion
Diversity among physicians leads to better overall patient care through improved quality of physician-patient interactions [14, 24, 33, 34], increased treatment of underserved populations [22] amidst disparities in orthopaedic surgery [2, 8, 35], and potentially greater inclusivity of underrepresented groups in research [33]. The need for greater diversity in orthopaedic surgery has been well documented [31, 33, 38]. Encouraging medical students from diverse backgrounds to pursue orthopaedics is an important component of improving diversity in the field, but to do so, we must establish an understanding of students’ perceptions of diversity and inclusion in orthopaedics. Furthermore, although many students gain exposure to the field through a clinical orthopaedic rotation, we lack knowledge on how participation in such a rotation might affect these perceptions. Even with an estimated response percentage of 26%, we found that before an orthopaedic clinical rotation, cis-women and underrepresented racial minorities had worse views on the level of diversity and inclusion in orthopaedic surgery compared with cis-men and white students, respectively. Many of these differences ceased to exist after the rotation. Nonmajority demographic groups saw prerotation to postrotation improvement in several views on diversity and inclusion in orthopaedics. These findings suggest that increasing exposure of diverse students to orthopaedic surgery through clinical rotations may improve perceptions these students hold of orthopaedics and may promote diversification by making these students more likely to pursue the field.
Limitations
This study has several limitations. Because our survey was delivered to a large number of medical schools with an unknown number of eligible respondents during the study period, we were unable to calculate an exact response percentage. However, we calculated an estimated response percentage of 26%. To evaluate the nonresponse bias, we compared all early versus late responders, the latter of whom are likely more representative of nonresponders [21]. We found that for only three survey questions (likelihood of pursing orthopaedic surgery, homophobic versus nonhomophobic nature of field, and racist versus nonracist nature of field), late responders had a more favorable perception of diversity in orthopaedic surgery, whereas for the remainder of questions, there was no difference (Appendix 4). It should be noted that of those three questions, only the question regarding likelihood of pursuing orthopaedic surgery demonstrated significant findings in our study results when comparing scores across demographic groups. It is possible that for this question, our findings were overinflated as a result of this nonresponse bias. On the other hand, the questions related to the nonhomophobic/homophobic and nonracist/racist nature of the field, although possibly suffering from nonresponse bias, are less likely to influence our study results that compare demographic groups. Given the limited number of questions that showed differences in the early versus late responder analysis, we believe that nonresponse bias does not meaningfully alter the interpretability of our results. Nonetheless, future studies should strive to achieve higher response percentages.
It was also important for us to consider the possibility of selection bias, where students of nonmajority demographic backgrounds may have been more likely to complete the survey than students from majority backgrounds. One of the primary goals of our study was to evaluate the prerotation to postrotation change in scores within the nonmajority groups. Even if these groups self-selected to some extent, we felt that we were able to still meet this goal, given that these may be exactly the students in whom we are trying to assess the effect of the rotation. Thus, we do not feel that this selection bias would substantially alter our conclusions. We were also still able to conduct our analysis comparing across majority and nonmajority demographic groups, although here it is possible that some findings may have been overinflated if nonmajority demographic students with worse perceptions were more likely to complete the survey. Our results may have been affected by recall bias because we could not control for the timing of rotations. It is also possible that students who more recently completed a rotation might feel compelled to provide a more favorable review. To address whether recency of the rotation may have served as a potential confounder, we compared time since rotation completion across the demographic groups and found no difference. Nonetheless, future studies could prospectively follow students and have surveys completed in short timeframes before and after the rotation. The low number of responses from students identifying as nonheterosexual limited our analysis of this demographic group, and we likely did not achieve sufficient power to identify significant results for this group. Thus, any lack of significant findings concerning sexual orientation in our study should not be interpreted as definitively indicating that differences do not exist. Future work could incorporate a greater number of medical schools to increase the number of nonheterosexual and underrepresented racial minority students who are included. We did not separately analyze students identifying with more than one nonmajority demographic; rather, we focused on the independent associations of each demographic variable. Although this approach likely improved interpretability of our results, future studies could separately study individuals who report intersectionality between demographic groups. Our survey was distributed to 27 medical schools. Even though we tried to be as representative as possible with the schools included, incorporating both MD- and DO-granting institutions, schools of varying sizes, and in different regions, a survey distributed to all medical students would be by definition maximally representative of US medical students. Future studies could explore avenues by which to capture this large survey population.
Diversity and Inclusion Perceptions by Demographic Group, Before and After Rotation
Nonmajority demographic students have worse views of the level of diversity and inclusion in orthopaedic surgery compared with their majority counterparts, particularly when cis-women are compared with cis-men, and especially before participation in an orthopaedic clinical rotation. As we seek to diversify orthopaedic surgery for the sake of patient care, these findings highlight the need to target recruitment efforts toward students of diverse backgrounds. This is an area where orthopaedic organizations can take an active role. For example, nationally, emphasis should be placed on “pipeline programs” that promote students from diverse backgrounds to explore orthopaedics. These programs include the Perry Initiative [25] and Nth Dimensions [18, 27]. Scholarships for members of nonmajority demographic groups can also contribute, including the Ruth Jackson Orthopaedic Society’s scholarships for women students to attend the annual meeting of the American Academy of Orthopaedic Surgeons, and diversity scholarships for rotating students. These initiatives provide orthopaedic exposure to students of diverse backgrounds. Our finding that cis-women hold worse views compared with cis-men are broadly consistent with prior studies assessing women’s perceptions of orthopaedics [7, 19, 28]. These studies found that women’s interest was diminished by the “predominantly male nature of the field,” [7] and that lack of acceptance by senior faculty served as a potential deterrent [19]. Our study takes these findings one step further by directly assessing diversity-related metrics from diversity, equity, and inclusion climate surveys used at major academic institutions, as well as by assessing perceptions before and after the clinical rotation. In terms of racial/ethnic and sexual orientation diversity, we found that before the rotation, underrepresented racial minority students believed less that diversity and inclusion are part of orthopaedic surgery culture compared with white students, and we did not see differences between heterosexual and nonheterosexual students. Prior evidence is lacking about underrepresented racial minority and nonheterosexual students’ perceptions of diversity and inclusion in orthopaedics. Our study is one of the first to assess these demographic groups and provides a foundation for future studies to further explore barriers that these students may face. Future work should focus on increasing response percentages among these groups. Given that diversity plays a role in the decision to pursue orthopaedic surgery, at least for women and underrepresented minorities [23, 29, 30], and that nonmajority demographic groups tend to have worse views on diversity in orthopaedics, it is important that we take steps to improve these views.
Improvement in Perceptions of Diversity and Inclusion Among Nonmajority Groups
Participation in an orthopaedic surgery clinical rotation is associated with improved views of diversity and inclusion among students of nonmajority demographic backgrounds. This finding provides a method by which to encourage medical students of diverse backgrounds to pursue orthopaedic surgery. Our data, and those of previous studies, support the importance of participation in an orthopaedic rotation or other musculoskeletal curriculum [7, 10, 19, 20, 26]. Rotations in the third and fourth years of medical school have the largest influence on specialty choice among students [20], and women, more often than men, choose orthopaedics as a career after beginning clinical rotations [19], further highlighting the value of rotations. Our study builds on these findings by clearly demonstrating the association between rotations and improving perceptions of diversity and inclusion of the field among students of diverse backgrounds. Future studies should prospectively follow students completing their orthopaedic rotations and survey students before and after the rotations, rather than at a single postrotation point.
Multiple stakeholders can make use of our findings to promote student participation in orthopaedic rotations. Medical schools and national medical school organizations have a responsibility to encourage increased diversity in various medical and surgical specialties. Indeed, one of the missions of the American Association of Medical Colleges is that: “Medical schools and teaching hospitals are committed to developing a culturally competent, diverse, and well-prepared health care workforce” [6]. Recognizing that space in medical school curricula is limited, and that there is an immense need for increased diversity in orthopaedics—especially compared with other specialties [1, 31, 33, 38]—and the impact of diversity on patient care [14, 22, 24, 33, 34], medical schools should explore ways to increase clinical exposure to orthopaedics and musculoskeletal health. At our institution for example, orthopaedic surgery is offered as a 2-week elective during the 8-week core surgery rotation. Although ideally some time on an orthopaedic service should be a required curricular component, schools should at least offer an orthopaedic elective during the surgery or other core rotation. Orthopaedic departments and residency programs also play a role in improving medical student exposure. This effect of the rotation may not be intrinsic to the rotation itself, but rather a result of the efforts of residents and attending physicians to improve students’ perceptions of orthopaedic culture. Departments can also find innovative ways to interface with medical students. At our institution, the orthopaedic surgery department hosts a case-based workshop guiding students through basic procedures on cadavers during the first-year medical student anatomy course. The session serves not only an educational purpose but also allows students to interact with residents and faculty. Through these efforts, we hope to see higher numbers of diverse applicants pursuing orthopaedic surgery.
Discussion
Even with an estimated response percentage of 26%, we found that cis-women and underrepresented racial minority medical students held more negative perceptions of the extent of diversity and inclusion in orthopaedics than did cis-men and white students, respectively. However, participation in an orthopaedic rotation was associated mitigation of many of these negative perceptions among women, underrepresented racial minorities, and nonheterosexual students. Given the impact of a diverse workforce on patient care, the responsibility of medical schools and medical school organizations to promote a diverse workforce, and the great need for diversity in orthopaedics, we encourage medical schools to require a short clinical orthopaedic rotation. Orthopaedic departments, residency programs, and national organizations should also work to increase student exposure to the field, including through interactive sessions during the preclinical years, promotion of pipeline programs, and provision of scholarships to diverse students. It is our hope that these steps will help increase the diversity of orthopaedic surgery and ultimately, further improve patient care.
Supplementary Material
Acknowledgments
We thank the Johns Hopkins Institute for Clinical and Translational Research for providing feedback throughout the duration of this research. We thank Dr. Gayane Yenokyan for her input on the statistical analysis.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The institution of one of the authors (RR) has received, during the study period, funding from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health, and the National Institutes of Health Roadmap for Medical Research, via grant number TL1 TR003100.
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Adelani MA, Harrington MA, Montgomery CO. The distribution of underrepresented minorities in U.S. orthopaedic surgery residency programs. J Bone Joint Surg Am. 2019;101:e96. [DOI] [PubMed] [Google Scholar]
- 2.Amen TB, Varady NH, Rajaee S, Chen AF. Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the U.S.: a comprehensive analysis of trends from 2006 to 2015. 2020;102:811-820. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Orthopaedic Surgeons Department of Clinical Quality and Value. Orthopaedic practice in the U.S. 2018. Available at: https://www.aaos.org/quality/practice-management/aaos-orthopaedic-surgeon-census/. Accessed June 10, 2020.
- 4.Association of American Medical Colleges 2019. Fall applicant, matriculant, and enrollment data tables. Available at:https://www.aamc.org/system/files/2019-12/2019%20AAMC%20Fall%20Applicant%2C%20Matriculant%2C%20and%20Enrollment%20Data%20Tables_0.pdf. Accessed April 29, 2020.
- 5.Association of American Medical Colleges Applicant, matriculant, & graduation, by medical school tables. Available at: https://www.aamcdiversityfactsandfigures2016.org/report-section/medical-schools/#tablepress-33. Accessed September 14, 2020.
- 6.Association of American Medical Colleges Mission areas. Available at https://www.aamc.org/what-we-do/mission-areas. Accessed September 14, 2020.
- 7.Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34:e919-932. [DOI] [PubMed] [Google Scholar]
- 8.Bederman SS, Rosen CD, Bhatia NN, Kiester PD, Gupta R. Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. Clin Orthop Relat Res. 2012;470:1090-1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bender R, Lange S. Adjusting for multiple testing--when and how? J Clin Epidemiol. 2001;54:343-349. [DOI] [PubMed] [Google Scholar]
- 10.Bernstein J, DiCaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004;86:2335-2338. [DOI] [PubMed] [Google Scholar]
- 11.Brotherton SE, Etzel SI. Graduate medical education, 2018-2019. JAMA. 2019;322:996-1016. [DOI] [PubMed] [Google Scholar]
- 12.Case Western Reserve University Office of Inclusion D, and Equal Opportunitiy. Case Western Reserve University 2010‐2011 climate survey: results on common questions. Available at: https://case.edu/diversity/sites/case.edu.diversity/files/2018-04/Climate.pdf. Accessed April 29, 2020.
- 13.Chapman TR, Zmistowski B, Prestowitz S, Purtill JJ, Chen AF. What is the geographic distribution of women orthopaedic surgeons throughout the United States? Clin Orthop Relat Res. 2020;478:1529-1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583-589. [DOI] [PubMed] [Google Scholar]
- 15.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010;92:2328-2335. [DOI] [PubMed] [Google Scholar]
- 16.Dobbs MB, Gebhardt MC, Gioe TJ, et al. Editorial: How does CORR® evaluate survey studies? 2017;475:2143-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). 2004;6:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrington MA, Rankin EA, Ladd AL, Mason BS. The orthopaedic workforce is not as diverse as the population it serves: where are the minorities and the women? AOA Critical Issues Symposium. J Bone Joint Surg Am. 2019;101:e31. [DOI] [PubMed] [Google Scholar]
- 19.Hill JF, Yule A, Zurakowski D, Day CS. Residents' perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013;95:e1441-1446. [DOI] [PubMed] [Google Scholar]
- 20.Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94:e78. [DOI] [PubMed] [Google Scholar]
- 21.Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307:1805-1806. [DOI] [PubMed] [Google Scholar]
- 22.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. 1996;334:1305-1310. [DOI] [PubMed] [Google Scholar]
- 23.Kroin E, Garbarski D, Shimomura A, Romano J, Schiff A, Wu K. Gender differences in program factors important to applicants when evaluating orthopaedic surgery residency programs. J Grad Med Educ. 2019;11:565-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kundhal KK, Kundhal PS. MSJAMA. Cultural diversity: an evolving challenge to physician-patient communication. JAMA. 2003;289:94. [DOI] [PubMed] [Google Scholar]
- 25.Lattanza LL, Meszaros-Dearolf L, O'Connor MI, et al. The Perry Initiative's medical student outreach program recruits women into orthopaedic residency. Clin Orthop Relat Res. 2016;474:1962-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.London DA, Calfee RP, Boyer MI. Impact of a musculoskeletal clerkship on orthopedic surgery applicant diversity. Am J Orthop (Belle Mead NJ). 2016;45:E347-E351. [PubMed] [Google Scholar]
- 27.Mason BS, Ross W, Ortega G, Chambers MC, Parks ML. Can a strategic pipeline initiative increase the number of women and underrepresented minorities in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1979-1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Connor MI. Medical school experiences shape women students' interest in orthopaedic surgery. Clin Orthop Relat Res. 2016;474:1967-1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okike K, Phillips DP, Johnson WA, O'Connor MI. Orthopaedic faculty and resident racial/ethnic diversity is associated with the orthopaedic application rate among underrepresented minority medical students. J Am Acad Orthop Surg. 2020;28:241-247. [DOI] [PubMed] [Google Scholar]
- 30.Okike K, Phillips DP, Swart E, O'Connor MI. Orthopaedic faculty and resident sex diversity are associated with the orthopaedic residency application rate of female medical students. J Bone Joint Surg Am. 2019;101:e56. [DOI] [PubMed] [Google Scholar]
- 31.Poon S, Kiridly D, Mutawakkil M, et al. Current trends in sex, race, and ethnic diversity in orthopaedic surgery residency. J Am Acad Orthop Surg. 2019;27:e725-e733. [DOI] [PubMed] [Google Scholar]
- 32.Poon S, Nellans K, Rothman A, et al. Underrepresented minority applicants are competitive for orthopaedic surgery residency programs, but enter residency at lower rates. J Am Acad Orthop Surg. 2019;27:e957-e968. [DOI] [PubMed] [Google Scholar]
- 33.Ramirez RN, Franklin CC. Racial diversity in orthopedic surgery. Orthop Clin North Am. 2019;50:337-344. [DOI] [PubMed] [Google Scholar]
- 34.Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713-1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schoenfeld AJ, Tipirneni R, Nelson JH, Carpenter JE, Iwashyna TJ. The influence of race and ethnicity on complications and mortality after orthopedic surgery: a systematic review of the literature. Med Care. 2014;52:842-851. [DOI] [PubMed] [Google Scholar]
- 36.Sellers R. University of Michigan campus climate survey on diversity, equity and inclusion, Ann Arbor, Michigan, 2016. Available at: https://diversity.umich.edu/wp-content/uploads/2017/11/DEI-STUDENT-REPORT-FINAL.pdf. Accessed April 29, 2020. [Google Scholar]
- 37.The University of Chicago CCC. The University of Chicago Spring 2016 campus climate survey, diversity and inclusion: survey results. Available at: https://provost.uchicago.edu/sites/default/files/documents/reports/Spring2016ClimateSurveyReport.pdf. Accessed April 29, 2020.
- 38.Tougas C, Valtanen R, Bajwa A, Beck JJ. Gender of presenters at orthopaedic meetings reflects gender diversity of society membership. J Orthop. 2020;19:212-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United States Census Bureau Census regions and divisions of the United States. Available at: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed April 29, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


