Abstract
Background:
In the United States, methadone provision for opioid use disorder (OUD) occurs at opioid treatment programs (OTPs). Ohio recently enacted a policy to expand methadone administration to Federally Qualified Health Centers (FQHC). We compared how the provision of methadone at current OTPs or the proposed expansion to FQHCs and pharmacies meets the urban and rural need for OUD treatment.
Methods:
Cross-sectional geospatial analysis of zip codes within Ohio with at least one 2017 opioid overdose death stratified by Rural-Urban Commuting Area codes. Our primary outcome was the proportion of need by zip code (using opioid overdose deaths as a proxy for need) within a 15- or 30- minute drive time of an OTP
Results:
Among 581 zip codes, sixty four percent of treatment need was within a 15-minute drive time and 81%, within a 30-minute drive time. The proportion of need within a 15-minute drive decreased with increasing rural classification (urban 78%, suburban 20%, large rural 9%, and small rural 1%; p < .001). The portion of need within a 15-minute drive time increased with the addition of FQHCs (96%) and the addition of chain pharmacies (99%) relative to OTPs alone among all zip codes and for all urban-rural strata (p < .001).
Conclusion:
Over one-third of OUD treatment need was not covered by existing OTPs and coverage decreased with rural classification of zip codes. Most of the gap between supply and need could be mitigated with FQHC methadone provision, which would expand both urban and rural access.
Keywords: Opioid use disorder, Methadone, Treatment access, Geospatial analysis
1. INTRODUCTION
In 2017, over four thousand opioid overdose deaths occurred in Ohio, the second highest rate among states (39.2 per 100,000) (Scholl et al., 2019). Access to medications for opioid use disorder (MOUD), methadone, buprenorphine, and naltrexone, in all treatment settings is critical for reducing morbidity and mortality of opioid use disorder (OUD) (Leshner and Mancher, 2019). While rates of drug overdose deaths are similar within urban and rural counties (22.0 and 20.0 per 100,000, respectively), MOUD services are concentrated in urban settings (Barnett et al., 2019; Douthit et al., 2015; Hedegaard et al., 2019; Lister et al., 2019).
Methadone treatment for OUD is especially effective in reducing opioid overdose deaths, the spread of infectious disease, and criminal justice involvement among people with OUD (Leshner and Mancher, 2019). Methadone may best accommodate the needs of some patients with OUD, as it is associated with a greater treatment retention relative to buprenorphine and does not require discontinuation of opioids prior to initiation like naltrexone (Leshner and Mancher, 2019; Mattick et al., 2014). Within the US, methadone for OUD can only be provisioned at Substance Abuse and Mental Health Services Administration (SAMHSA) certified opioid treatment programs (OTPs), limiting methadone to specialized facilities. As a result, only a minority of US counties contain one or more OTP (Abraham et al., 2018; Calcaterra et al., 2019; Mojtabai et al., 2019) and travel represents a unique barrier for methadone treatment relative to other chronic diseases (Joudrey et al., 2019). Federal statutes require methadone administration (observed medication dosing) six days a week during the first 90 days of treatment with gradually increasing take home medication allowance thereafter. Many people face long drive times to the nearest OTP and this disparity is greater in rural versus urban communities (Joudrey et al., 2020, 2019).
With the rise in opioid overdose deaths in rural counties, there have been renewed calls for reforming methadone delivery within the US, including integrating methadone into primary care and utilization of alternative settings for administration (Calcaterra et al., 2019; Samet et al., 2018). International examples exist in Canada, Australia, and the United Kingdom which allow primary care prescribing and community pharmacy administration of methadone to expand access (Calcaterra et al., 2019). In the US, federal regulations allow healthcare facilities (i.e. pharmacies) affiliated with an OTP to operate as a medication unit for methadone administration (“42 CFR 8.12 - Federal opioid treatment standards.,” n.d.), but state regulatory restrictions have limited medication unit adoption (McBournie et al., 2019). Federally Qualified Health Centers (FQHC) were created to improve access to primary care services in under resourced communities, but federal and state regulations have prevented widespread FQHC methadone provision (Calcaterra et al., 2019; Samet et al., 2018). To expand methadone services, Ohio enacted a 2019 policy encouraging the utilization of FQHCs and other settings (i.e. jails or county health departments) as medications units for methadone administration but did not include pharmacies despite federal regulations allowing pharmacies to serve as medication units (Lawriter Ohio Laws and Rules, 2019; McBournie et al., 2019).
It is unknown how the utilization of existing health care facilities for methadone administration, such as Ohio’s new policy for FQHCs, could extend access to methadone treatment to urban and rural communities experiencing OUD treatment need. Prior research on geographic access to methadone has used the general population to represent OUD treatment need (Joudrey et al., 2019, 2020; Kleinman, 2020), and has not explored the extent to which the urban and rural distribution of OTPs overlaps with the need for OUD treatment. Therefore, we compared how the provision of methadone at current OTPs or the proposed addition of FQHCs and pharmacies overlaps with OUD treatment need, using opioid overdose deaths as a proxy measure.
2. MATERIALS AND METHODS
2.1. Setting and Data Sources
We obtained data on 2017 overdose deaths from the Ohio Department of Health Bureau of Vital Statistics. Overdose death data obtained from the Ohio Department of Health was not suppressed and included all 2017 events. Consistent with Ohio Department of Health definition of opioid overdose deaths, we included all unintentional deaths (International Statistical Classification of Diseases [ICD] −10 codes X40–X44) with associated multiple cause of death ICD-10 codes T40.0-T40.4 and T40.6(Ohio Department of Health, 2019). We excluded opioid overdose deaths without an associated zip code. We obtained street addresses for all OTPs within Ohio on May 18, 2019 from the SAMHSA Behavior Health Treatment Services locator, which derive from 2018 National Survey of Substance Abuse Treatment Services data (SAMHSA, n.d.). We obtained 2017 FQHC street addresses from the Health Resources and Services Administration data warehouse (Health Resources & Services Administration, n.d.). To represent the potential of methadone administration within one national pharmacy chain, we obtained street addresses for all Walmart pharmacies via Walmart’s online Store Finder service (Walmart, n.d.). Latitude and longitude coordinates of the population weighted center of each zip code were obtained from Zipcode.org (accessed May 22, 2020) which uses data from the United States Postal Service and United States Census Bureau (“ZipCode.org - Zip Codes for USA,” n.d.). The Institutional Review Board of Yale University approved this study.
2.2. Study population
We included all Ohio zip codes with opioid overdose deaths in 2017. We included all OTPs identified as providing methadone maintenance for OUD within the SAMHSA treatment locator, non-school based FQHCs, and Walmart pharmacies within the state of Ohio. OTP and FQHC street addresses were geocoded using Esri ArcGIS online geocoding service via a three-step process described previously (Joudrey et al., 2020, 2019). Street addresses matched to the center of a polygon (i.e. center of municipality) with a tied highest match score or a match score less than 80 were hand reviewed using Google Maps. Pharmacy locations were geocoded using Bing maps API and were hand reviewed using Google Maps. We excluded OTPs, FQHCs, and pharmacies when the location could not be confirmed.
2.3. Study Variables
We stratified zip codes based on their Rural-Urban Commuting Area (RUCA) codes into a four level urban-rural classification scheme: urban (codes 1), suburban (codes 2 to 3), large rural (codes 4 to 6), and small rural (codes 7 to 10) (Hailu and Wasserman, 2016). For each zip code, we generated a count of 2017 opioid overdose deaths.
Our primary outcome was the proportion of OUD treatment need (using opioid overdose deaths as a proxy) aggregated by zip code within a 15-minute drive time of a methadone treatment facility, namely an OTP, FQHC, or pharmacy. We determined this percentage using a maximal multiple coverage location problem (Appendix 1), which maximizes the coverage of need for services among a fixed number of facilities based on geographic proximity (Masog, 1981). Maximal coverage models have been previously used for applied public service problems, such as emergency medical or fire services but as of yet have not been applied to OTP services (Murray, 2016). Within our coverage model, the amount of need in each zip code was approximated by the total count of opioid overdose deaths. We chose opioid overdose deaths to represent need for two reasons: 1) it is a widely used measure of OUD related harm and 2) opioid overdose deaths represent the highest priority outcome for intervention and therefore its advantageous to prioritize treatment service locations around overdose deaths. In our primary analysis, OUD treatment need was covered if the nearest methadone facility was within a 15-minute drive time of the population weighted center point of the zip code. We selected a 15-minute drive time for our primary analysis given prior studies demonstrated reduced methadone treatment retention at short travel times and distances (Amiri et al., 2020, 2018; Friedmann et al., 2001; Greenfield et al., 1996; Schmitt et al., 2003). We calculated drive time using Bing Map Distance Matrix API (Microsoft, 2020), which calculates drive time by simulating automobile movement based on historical trip averages. We applied our coverage model to three conditions. First, coverage by existing services was calculated as the portion of OUD treatment need covered by OTP facilities. Second, to represent the potential of FQHC administration in accordance with Ohio’s new policy, we calculated the combined coverage of OTP and FQHC facilities. Finally, to represent the added potential of a chain pharmacy administration, we calculated the combined coverage of OTP, FQHC, and Walmart pharmacies.
As a secondary outcome, we counted the facilities used to deliver services in the coverage model. A facility was utilized if it was the closest within the coverage area. Coverage by OTPs was prioritized over coverage by FQHCs or pharmacies so that only zip codes outside of OTP service coverage were assigned to the nearest FQHC or pharmacy. To represent coverage for patients with greater ability to travel, we repeated our coverage models using a 30-minute drive time threshold. Additionally, because there may be OUD treatment need even in zip codes without an overdose death, we examined coverage of all zip codes by repeating our analysis while assigning one overdose death to each zip code with no overdose deaths.
2.4. Statistical Analysis
First, by RUCA urban-rural strata, we compared a count of zip codes and a count of the number of overdose deaths using a chi-square test. We then used a chi-square test to compare the portion of OUD treatment need covered by the three methadone treatment availability conditions (OTPs only, OTPs and FQHCs, and OTPs, FQHCs, and pharmacies) among all zip codes and across each urban-rural strata. We completed a sensitivity analysis to examine the impact of using alternative data to represent OUD treatment need. We repeated our analysis using 2017 Ohio emergency medical services overdose call locations by zip code obtained from the Ohio Department of Public Safety’s Division of Emergency Medical Services (Ohio Emergency Medical Services, n.d.). Among all 2017 emergency medical service calls in the state of Ohio, we included 24333 calls with overdose only as the call impression. These overdose calls were in 615 Ohio zip codes. All hypothesis tests were two-sided with an alpha 0.05. We completed our analyses in Python 3.6.
3. RESULTS
3.1. Zip codes and treatment facilities
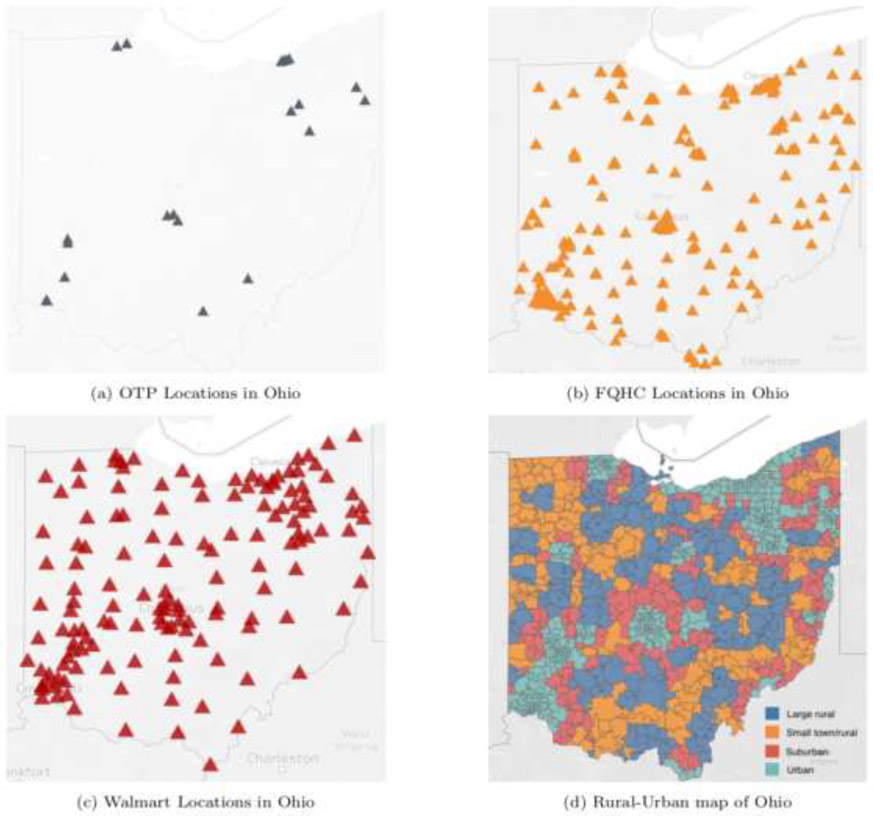
There were 4183 opioid overdose deaths with an associated zip code in 2017, of which 535 (13%) were within rural (large or small rural) zip codes. We excluded 115 overdose deaths without an associated zip code. Of the 1447 zip codes in Ohio, we excluded 859 with zero overdose deaths. Among included zip codes (n = 581), 144 (25%) were classified rural (Figure 1). Of the 22 OTP, 267 FQHCs, 145 pharmacy addresses, all were successfully geocoded.
Figure 1: Locations of opioid treatment programs, federally qualified health centers, and Walmart pharmacies, and Ohio zip codes by urban-rural classification.
astratified zip codes based on their Rural-Urban Commuting Area (RUCA) codes into a four-level urban-rural classification scheme: urban (codes 1), suburban (codes 2 to 3), large rural (codes 4 to 6), and small rural (codes 7 to 10)
3.2. Proportion of overdose deaths covered
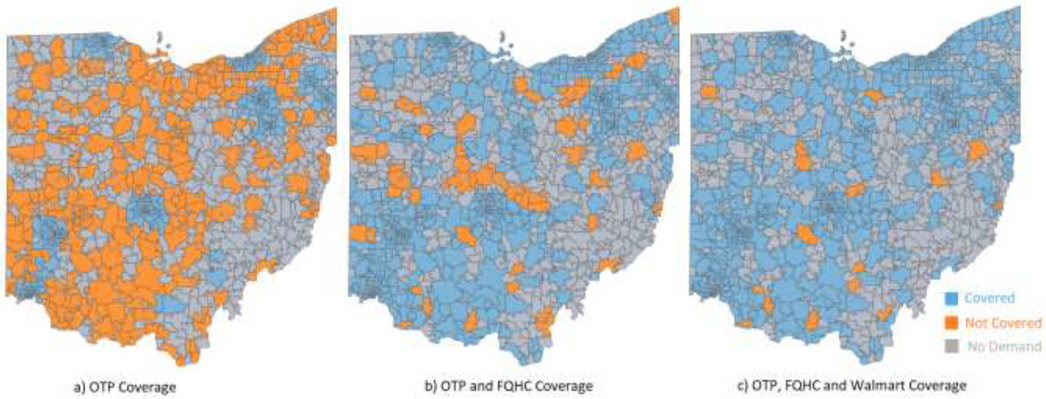
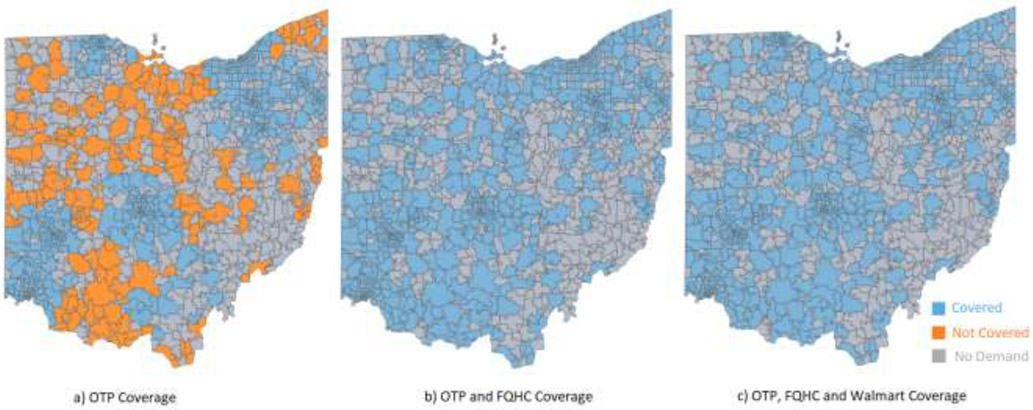
Among all zip codes with at least one opioid overdose death, 64% (n = 2684) of OUD treatment need was within a 15-minute drive time of an OTP and 81% (n = 3420) was within a 30-minute drive time (Table 1). The proportion of OUD treatment need within a 15-minute drive time increased with the addition of FQHCs facilities to 96% (n = 4001) and with the addition FQHCs and pharmacy facilities to 99% (n = 4153) relative to coverage by OTPs alone among all zip codes (Figure 2) and for all RUCA urban-rural strata (p < .001) (Table 2). All OUD treatment need was covered within a 30-minute drive time by OTPs and FQHCs combined (Figure 3).
Table 1.
The proportion of zip code opioid use disorder treatment need (represented by opioid overdose deaths) within a 15- and 30-minute drive time of a methadone treatment facility in 2017
| Coverage requirement |
Potential facility locations | Total number of zip codes covered (n = 581) |
Total number of OD covered (n = 4183) |
Total number of locations used | p-valuesa |
|---|---|---|---|---|---|
| 15-min coverage | OTP Only | 256 (44%) | 2684 (64%) | 22 OTP | p<.001 |
| OTP and FQHC | 520 (90%) | 4001 (96%) | 22 OTP, 82 FQHC | ||
| OTP, FQHC, and Pharmacy | 563 (97%) | 4153 (99%) | 22 OTP, 47 FQHC, 45 Pharmacies | ||
| 30-min coverage | OTP Only | 398 (69%) | 3420 (81%) | 22 OTP | p<.001 |
| OTP and FQHC | 581 (100%) | 4183 (100%) | 22 OTP, 28 FQHC | ||
| OTP, FQHC, and Pharmacy | 581 (100%) | 4183 (100%) | 22 OTP, 11 FQHC, 16 Pharmacies |
OD: Treatment need represented by opioid overdose deaths, OTP: Opioid Treatment Program, FQHC: Federally Qualified Health Centers
Chi-Square Test is applied to calculate p-values for the comparisons OTP only, OTP and FQHC, and OTP, FQHC, and Walmart pharmacy
Figure 2:
Zip code opioid use disorder treatment need (represented by opioid overdose deaths) within a 15-minute drive time of a methadone treatment facility in 2017
Table 2.
The proportion of zip code opioid use disorder treatment need by urban-rural classification (represented by opioid overdose deaths) within a 15- and 30-minute drive time of a methadone treatment facility in 2017
| Total number of covered | ||||||
|---|---|---|---|---|---|---|
| Coverage requirement |
Potential facility locations |
Urbana zip code (n = 350) |
Suburban zip code (n = 87) |
Large rural zip code (n = 88) |
Rural zip code (n = 56) | p-values |
| OTP Only | 244 (70%) | 7 (8%) | 4 (5%) | 1 (2%) | p < .001 | |
| OTP and FQHC | 338 (97%) | 71 (82%) | 70 (80%) | 41 (73%) | p < .001 | |
| OTP, FQHC, and Pharmacy | 350 (100%) | 81 (93%) | 80 (91%) | 52 (93%) | p < .001 | |
| 15-min coverage | Urban OD (n = 3361) | Suburban OD (n = 287) |
Large rural OD (n = 427) |
Rural OD (n = 108) | ||
| OTP Only | 2617 (78%) | 57 (20%) | 9 (2%) | 1 (1%) | p < .001 | |
| OTP and FQHC | 3311 (99%) | 253 (88%) | 357 (84%) | 80 (74%) | p < .001 | |
| OTP, FQHC, and Pharmacy | 3361 (100%) | 273 (95%) | 418 (98%) | 101 (94%) | p < .001 | |
| Urban zip code (n = 350) |
Suburban zip code (n = 87) |
Large rural zip code (n = 88) |
Rural zip code (n = 56) | p-values | ||
| OTP Only | 318 (91%) | 45 (52%) | 24 (27%) | 11 (20%) | p < .001 | |
| OTP and FQHC | 350 (100%) | 87 (100%) | 88 (100%) | 56 (100%) | p < .001 | |
| OTP, FQHC, and Pharmacy | 350 (100%) | 87 (100%) | 88 (100%) | 56 (100%) | p < .001 | |
| 30- min coverage | Urban OD (n = 3361) | Suburban OD (n = 287) |
Large rural OD (n = 427) |
Rural OD (n = 108) | p-values | |
| OTP Only | 3113 (93%) | 201 (70%) | 80 (19%) | 26 (24%) | p < .001 | |
| OTP and FQHC | 3361 (100%) | 287 (100%) | 427 (100%) | 108 (100%) | p < .001 | |
| OTP, FQHC, and Pharmacy | 3361 (100%) | 287 (100%) | 427 (100%) | 108 (100%) | p < .001 | |
OD: Treatment need represented by opioid overdose death, OTP: Opioid Treatment Program, FQHC: Federally Qualified Health Centers
stratified zip codes based on their Rural-Urban Commuting Area (RUCA) codes into a four-level urban-rural classification scheme: urban (codes 1), suburban (codes 2 to 3), large rural (codes 4 to 6), and small rural (codes 7 to 10)
Figure 3: Zip code opioid use disorder treatment need (represented by opioid overdose deaths) within a 30-minute drive time of a methadone treatment facility in 2017.
OD: Overdose, OTP: Opioid Treatment Program, FQHC: Federally Qualified Health Centers
Covered zip codes had the population weighted center point within a 15- or 30- minute drive time of a methadone treatment facility determined using a maximal multiple coverage location problem, which maximizes the coverage of need for services among a fixed number of facilities based on geographic proximity. No need zip codes contained no opioid overdose deaths in 2017
The portion of OUD treatment need covered by OTPs within a 15-minute drive time decreased with increasing rural zip code classification [urban 78% (n = 2617), suburban 20% (n = 57), large rural 9% (n = 2), small rural 1% (n = 1); p < .001]. Coverage of treatment need within a 15-minute drive time by OTPs and FQHCs combined and OTPs, FQHCs, and pharmacies combined also decreased with increasing rural zip code classification (p < .001) (Table 2). Coverage of OUD treatment need within a 30-minute drive time by OTPs decreased with increasing rural zip code classification (p. < 001), but coverage by OTPs and FQHCs and OTPs, FQHCs, and pharmacies did not vary by urban-rural classification given all treatment need was within the 30-minute coverage area (Table 2). Among non-urban zip codes, FQHC methadone administration extended 15-minute coverage to an additional 623 (76%) overdose deaths. Among urban zip codes, FQHC methadone administration extended 15-minute coverage to an additional 794 (21%) overdose deaths.
Within our 15-minute coverage model, all OTPs were used to deliver services to zip codes experiencing opioid overdose deaths (Table 1, Appendix Figure 1, and Appendix Figure 2). The addition of FQHCs to the coverage model resulted in the utilization of 82 (31%) FQHCs for methadone treatment and the addition of FQHCs and pharmacies resulted in the utilization of 47 (18%) FQHCs and 45 (31%) pharmacies for methadone treatment. Inclusion of all zip codes demonstrated 44% of Ohio zip codes were within a 15-minute drive time of an OTP, including 70% of urban and 5% of non-urban (suburban, large rural, and small rural) zip codes. (Appendix Table 1 and Appendix Figure 3)
In our sensitivity analysis, using emergency medical service overdose data to represent OUD treatment need did not change coverage comparisons across facility conditions and RUCA urban-rural strata (Appendix Table 2, Appendix Figure 4, and Appendix Figure 5). The portion of overdose deaths and overdose calls covered were similar among all zip codes and across RUCA urban-rural strata.
4. DISCUSSION
In this cross-sectional geospatial analysis from 581 zip codes within the state of Ohio, over one-third of OUD treatment need, represented by opioid overdose deaths, was not within a 15-minute drive time of OTP services. Coverage of OUD treatment need decreased with increasing rural classification so that the majority of non-urban (suburban, large rural, and small rural) opioid overdose deaths were outside of a 15-minute drive time to an OTP. OTP service coverage of OUD treatment need was so limited that nearly 20% opioid overdose deaths were within zip codes outside of our less conservative 30-minute coverage model. Most of this gap between supply and need for methadone treatment would be mitigated if recent changes in Ohio methadone policy resulted in broad adoption of FQHC methadone administration. Our coverage model indicates that the addition of administration at a chain pharmacy on top of OTP and FQHC methadone provision only resulted in a modest expansion in coverage of OUD treatment need, but pharmacies or other facilities may be required to ensure all people, including those with limited transportation options or in the most rural communities, have reasonable access to methadone as recommended by the National Academy of Sciences (Leshner and Mancher, 2019).
These results are consistent with previous evidence of a shortage of OTP facilities and of disproportionately long drive times to the nearest OTP in rural communities relative to urban communities (Abraham et al., 2018; Joudrey et al., 2019, 2020; Kleinman, 2020). By overlaying OUD treatment need and supply of methadone, these results demonstrate the extent to which this shortage in supply results in a gap in “coverage” of methadone. Previous research suggested adoption of methadone provision among FQHCs or pharmacies, consistent with methadone provision in Canada, Australia, and the United Kingdom, could reduce the urban-rural disparity in drive times to methadone facilities in the United States (Joudrey et al., 2019, 2020; Kleinman, 2020). These results suggest if Ohio’s recent methadone policy resulted in universal adoption of methadone administration within FQHCs, then methadone services would cover zip codes containing over 96% of the opioid overdose deaths. States like Ohio could prioritize implementation of FQHC methadone administration to expand methadone treatment access to most communities experiencing opioid overdoses. However, states utilizing FQHCs for methadone expansion may still need to identify additional options for local administration, such as pharmacies or mobile medication units, especially if not all FQHCs implement methadone administration.
These results expand upon previous research demonstrating the county density of OTPs and buprenorphine waivered providers were poorly matched to county rates of opioid overdose deaths in the United States (Haffajee et al., 2019; Jones et al., 2018). We address limitations of prior studies, specifically the size and heterogeneity of counties as a geographic unit of analysis and find evidence of a gap in OTP coverage of opioid overdose deaths in Ohio using the zip code as the geographic unit. Further, our drive time analyses are informed by road network data and historical trip averages as a measure of geographic access as compared to the density OTPs within counties (Haffajee et al., 2019). Previous national examinations of OTP supply and county opioid overdose deaths suggests states within the census bureau divisions of the East North Central (Midwest), Mountain, and South Atlantic may contain a similar or greater gap in methadone treatment supply and need and this should be the focus of further research (Haffajee et al., 2019; Kleinman, 2020).
By examining both supply and need for methadone treatment, these results suggest policies, like Ohio’s, will improve methadone access in both urban and rural communities experiencing opioid overdose deaths. Despite a 71% increase in the portion of opioid overdose deaths covered in non-urban zip codes, there was a greater absolute increase in the number of opioid overdose death covered in urban settings with FQHC methadone administration. This suggests policymakers should not overlook the benefit of methadone facility expansion in urban communities given the greater density of OUD treatment need. Patients in urban communities may also walk or ride a bus to an OTP, creating the need for a higher methadone facility density relative to rural communities to reduce travel burden. Further research is needed on how mode of transportation may impact access to methadone. The results also suggest opportunities for targeted facility expansion as gains in access required methadone administration in less than one-third of FQHCs. Opening additional methadone administration facilities may also provide alternatives to facilities with wait lists and this should be the focus of future research.
Implementation barriers such as cost, lack of knowledge, and stigma of methadone treatment may prevent broad adoption of methadone administration among Ohio FQHCs and blunt the impact of Ohio’s policy (McGinty et al., 2020; Tuchman, 2008). These results suggest states like Ohio will need to take additional actions if methadone treatment services are to reach all communities experiencing opioid overdose deaths. Methadone administration adoption by FQHCs may take place slowly, following a similar trajectory as DATA 2000 waiver adoption (Mojtabai et al., 2019). Implementation interventions will need to be developed and tested to support adoption. Our study focused on FQHCs not just because of the Ohio medication unit policy, but also because FQHCs are positioned to lead adoption. Characteristics of FQHCs which may support adoption include: the frequent co-location of pharmacies within FQHCs providing additional clinical space and expertise for methadone administration, an existing addiction workforce within FQHCs in the form of DATA 2000 waivered health professionals, and the FQHC mandate to serve underresourced or marginalized communities where people with OUD are overrepresented (Rodis et al., 2019). Methadone administration within FQHCs does not necessarily require additional staff as either nursing or pharmacy professionals can fill this role (“42 CFR 8.12 - Federal opioid treatment standards.,” n.d.). However, novel training programs will need to be developed to facilitate adoption among these health professionals. Per federal regulations, medication units do not provide counseling as this service is provided by the central OTP (“42 CFR 8.12 - Federal opioid treatment standards.,” n.d.).
Because some stakeholders may be concerned about diversion of methadone for OUD with the adoption of medication units within the United States, monitoring for diversion should be a part of programing and research. There are reasons to believe methadone administration within FQHCs and pharmacies are unlikely to change diversion rates. Because medication units must still provide observed methadone administration just like an OTP, they do not represent a change in medication administration procedures. In prior decades, the United States experienced a rise in methadone-related overdose deaths, but subsequent research demonstrated these events were associated with methadone prescribing for pain rather than methadone prescribing for OUD (Faul et al., 2017; Kuehn, 2012). Methadone for pain remains available within community pharmacies across the U.S.
Here we present data examining adoption of methadone administration within a chain pharmacy, but other options exist. A Drug Enforcement Agency proposal would allow states to operate new mobile methadone administration units in affiliation with a central OTP (McBournie et al., 2019). The utilization of FQHCs, pharmacies, and mobile services as methadone administration units does not change federal statutes requiring in-person evaluation at a central OTP prior to methadone initiation and (SAMHSA, 2020) has not modified this requirement in the context of the coronavirus disease 2019 (COVID) pandemic. Therefore, long drive times to OTPs may still prevent patient engagement, especially in rural communities, even with medication unit policies like Ohio’s. Finally, concerns about patient congregation at OTPs during COVID lead SAMHSA to increase allowances of take-home doses (SAMHSA, 2020); future research should examine how expansion of take-home doses may modify the travel burden and treatment outcomes associated with methadone.
4.1. Limitations
This study has several limitations. These results likely overestimate the coverage of methadone treatment services, as we do not account for the travel impedance from public transportation, traffic, weather, or construction. Additionally, not all OTPs may be accepting new methadone patients. Informed by federal methadone statutes and previous research, we present the supply of methadone treatment at a 15- and 30-minute drive, but further research on the relationship between drive time and individual level methadone treatment outcomes is needed to further specify the current gap in treatment. Opioid overdose deaths were aggregated to the level of zip code and our results should not be used for predictions of individual patient coverage. There may be year to year variation in the location of opioid overdose deaths and the location of overdose events will evolve over time. Opioid overdose deaths may underestimate treatment need in some zip codes. These results for the state of Ohio may not generalize to states with a higher density of OTPs such as states in the northeastern US. While our use of alternative data (EMS calls) to represent OUD treatment need was consistent with our primary analysis, the geography of OUD prevalence may differ from the geography of opioid overdose deaths or calls.
5. CONCLUSIONS
Over one-third of OUD treatment need in Ohio was not covered by existing OTPs, and the portion of need covered decreased with increasing rural zip code classification. Most of this gap between the supply and need for treatment could be mitigated if Ohio’s policy resulted in broad adoption of FQHC administration, expanding access in both urban and rural communities. However, states like Ohio may require additional methadone administration facilities for universal coverage in the most rural communities or in the setting of incomplete FQHC adoption.
Supplementary Material
HIGHLIGHTS.
Cross-sectional geospatial analysis of Ohio zip codes
Over one-third of opioid use disorder treatment need was not covered
The gap between supply and need could be mitigated with FQHC methadone provision
Acknowledgments
FUNDING SOURCE
Funding for this publication was provided by grant number 5K12DA033312 (P.J.J.) and 1DP2DA049282-01 and 2R37DA15612-16 (G.S.G.) from the National Institute on Drug Abuse, a components of the National Institutes of Health (NIH). In the past 36 months, Dr. Wang received research support through Yale University from the Bureau of Justice Administration to study reentry by linking correctional and community health system data (2015-RY-BX-K002) and the Substance Abuse and Mental Health Services Administration to study how to improve the health of women just released from corrections. Dr. Wang currently receives research support through Yale University from the National Cancer Institute of National Institute of Health (1R01CA230444), the National Heart, Lung, and Blood Institute (1R01HL137696), the National Institute of Minority Health and Disparities (1R01MD010403), and the National Institute of Drug Abuse (1UG1DA050072) to study incarceration and cancer, cardiovascular disease, gun violence, and opioid use disorder. She also receives funding from the William T. Grant Foundation to study health related barriers and facilitators to reducing criminal legal contact and from the California Health Care Foundation to evaluate the Transitions Clinic Network in California.
ROLE OF FUNDING SOURCE
The contents of this study are solely the responsibility of the authors and do not necessarily represent the official view of NIH. The above funders played no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
ABBREVIATIONS
- FQHC
Federally Qualified Health Center
- ICD
International Statistical Classification of Diseases
- OTP
opioid treatment program
- OUD
opioid use disorder
- RUCA
Rural-Urban Commuting Area
- SAMHSA
Substance Abuse and Mental Health Services Administration
- US
United States
- MOUD
medications for opioid use disorder
Footnotes
CONFLICT OF INTEREST
The authors have no declarations or conflict of interests to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 42 CFR 8.12 - Federal opioid treatment standards. [WWW Document], n.d. URL https://www.govregs.com/regulations/expand/title42_chapterI_part8_subpartC_section8.12#title42_chapterI_part8_subpartC_section8.12 (accessed 11.4.20).
- Abraham AJ, Andrews CM, Yingling ME, Shannon J, 2018. Geographic disparities in availability of opioid use disorder treatment for Medicaid enrollees. Health services research 53, 389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amiri S, Lutz R, Socías E, McDonell MG, Roll JM, Amram O, 2018. Increased distance was associated with lower daily attendance to an opioid treatment program in Spokane County Washington. Journal of substance abuse treatment 93, 26–30. [DOI] [PubMed] [Google Scholar]
- Amiri S, Lutz RB, McDonell MG, Roll JM, Amram O, 2020. Spatial access to opioid treatment program and alcohol and cannabis outlets: analysis of missed doses of methadone during the first, second, and third 90 days of treatment. The American Journal of Drug and Alcohol Abuse 46, 78–87. 10.1080/00952990.2019.1620261 [DOI] [PubMed] [Google Scholar]
- Barnett ML, Lee D, Frank RG, 2019. In Rural Areas, Buprenorphine Waiver Adoption Since 2017 Driven By Nurse Practitioners And Physician Assistants. Health Affairs 38, 2048–2056. 10.1377/hlthaff.2019.00859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcaterra SL, Bach P, Chadi A, Chadi N, Kimmel SD, Morford KL, Roy P, Samet JH, 2019. Methadone Matters: What the United States Can Learn from the Global Effort to Treat Opioid Addiction. J GEN INTERN MED 34, 1039–1042. 10.1007/s11606-018-4801-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douthit N, Kiv S, Dwolatzky T, Biswas S, 2015. Exposing some important barriers to health care access in the rural USA. Public Health 129, 611–620. 10.1016/j.puhe.2015.04.001 [DOI] [PubMed] [Google Scholar]
- Faul M, Bohm M, Alexander C, 2017. Methadone Prescribing and Overdose and the Association with Medicaid Preferred Drug List Policies — United States, 2007–2014. MMWR Morb Mortal Wkly Rep 66, 320–323. 10.15585/mmwr.mm6612a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Stein MD, 2001. Transportation and retention in outpatient drug abuse treatment programs. Journal of substance abuse treatment 21, 97–103. [DOI] [PubMed] [Google Scholar]
- Greenfield L, Brady JV, Besteman KJ, De Smet A, 1996. Patient retention in mobile and fixed-site methadone maintenance treatment. Drug & Alcohol Dependence 42, 125–131. [DOI] [PubMed] [Google Scholar]
- Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE, 2019. Characteristics of US Counties With High Opioid Overdose Mortality and Low Capacity to Deliver Medications for Opioid Use Disorder. JAMA Netw Open 2, e196373–e196373. 10.1001/jamanetworkopen.2019.6373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailu A, Wasserman C, 2016. Guidelines for Using Rural-Urban Classification Systems for Community Health Assessment. [Google Scholar]
- Health Resources & Services Administration, n.d. Data Explorer [WWW Document]. Data Explorer. URL https://data.hrsa.gov/tools/data-explorer (accessed 5.22.20). [Google Scholar]
- Hedegaard H, Miniño AM, Warner M, 2019. Urban–rural differences in drug overdose death rates, by sex, age, and type of drugs onvolved, 2017. [PubMed] [Google Scholar]
- Jones CW, Christman Z, Smith CM, Safferman MR, Salzman M, Baston K, Haroz R, 2018. Comparison between buprenorphine provider availability and opioid deaths among US counties. Journal of substance abuse treatment 93, 19–25. [DOI] [PubMed] [Google Scholar]
- Joudrey PJ, Chadi N, Roy P, Morford KL, Bach P, Kimmel S, Wang EA, Calcaterra SL, 2020. Pharmacy-based methadone dispensing and drive time to methadone treatment in five states within the United States: A cross-sectional study. Drug and Alcohol Dependence 211, 107968 10.1016/j.drugalcdep.2020.107968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joudrey PJ, Edelman EJ, Wang EA, 2019. Drive times to opioid treatment programs in urban and rural counties in 5 US states. Jama 322, 1310–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman RA, 2020. Comparison of Driving Times to Opioid Treatment Programs and Pharmacies in the US. JAMA Psychiatry. 10.1001/jamapsychiatry.2020.1624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn BM, 2012. Methadone Overdose Deaths Rise With Increased Prescribing for Pain. JAMA 308, 749 10.1001/jama.2012.9289 [DOI] [PubMed] [Google Scholar]
- Lawriter Ohio Laws and Rules, 2019. 5122-40-15 Medication units [WWW Document]. Lawriter Ohio Laws and Rules; URL http://codes.ohio.gov/oac/5122-40-15v1 (accessed 7.9.20). [Google Scholar]
- Leshner AI, Mancher M, 2019. Medications for Opioid Use Disorder Save Lives. National Academies of Sciences, Enginneering, and Medicine. [PubMed] [Google Scholar]
- Lister JJ, Weaver A, Ellis JD, Himle JA, Ledgerwood DM, 2019. A systematic review of rural-specific barriers to medication treatment for opioid use disorder in the United States. The American Journal of Drug and Alcohol Abuse 1–16. [DOI] [PubMed] [Google Scholar]
- Masog TG, 1981. Modelling techniques for a flexible emergency aid location system (PhD Thesis). University of Texas at Austin. [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2014. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane database of systematic reviews. [Google Scholar]
- McBournie A, Connolly E, Duncan A, Rising J, 2019. Methadone Barriers Persist, Despite Decades of Evidence. Health Affairs Blog. [Google Scholar]
- McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, Barry CL, 2020. Medication for Opioid Use Disorder: A National Survey of Primary Care Physicians. Annals of Internal Medicine. 10.7326/M19-3975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Microsoft, 2020. Bing Maps API [WWW Document]. URL https://www.microsoft.com/en-us/maps/choose-your-bing-maps-api (accessed 5.22.20).
- Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M, 2019. Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities. Health Affairs 38, 14–23. 10.1377/hlthaff.2018.05162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray AT, 2016. Maximal Coverage Location Problem: Impacts, Significance, and Evolution. International Regional Science Review 39, 5–27. 10.1177/0160017615600222 [DOI] [Google Scholar]
- Ohio Department of Health, 2019. 2018 Ohio Drug Overdose Data: General Findings. [Google Scholar]
- Ohio Emergency Medical Services, n.d. State of Ohio EMS Data Center [WWW Document]. URL https://www.ems.ohio.gov/data-center.aspx (accessed 5.26.20).
- Rodis JL, Capesius TR, Rainey JT, Awad MH, Fox CH, 2019. Pharmacists in Federally Qualified Health Centers: Models of Care to Improve Chronic Disease. Prev Chronic Dis 16 10.5888/pcd16.190163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Botticelli M, Bharel M, 2018. Methadone in Primary Care—One Small Step for Congress, One Giant Leap for Addiction Treatment. New England Journal of Medicine 379, 7–8. [DOI] [PubMed] [Google Scholar]
- SAMHSA, 2020. Opioid Treatment Program (OTP) Guidance [WWW Document]. URL https://www.samhsa.gov/sites/default/files/otp-guidance-20200316.pdf
- SAMHSA, n.d. Behavioral Health Treatment Services Locator [WWW Document]. URL https://findtreatment.samhsa.gov/ (accessed 8.27.20).
- Schmitt SK, Phibbs CS, Piette JD, 2003. The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addictive Behaviors 28, 1183–1192. 10.1016/S0306-4603(02)00218-6 [DOI] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G, 2019. Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity and Mortality Weekly Report 67, 1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuchman E, 2008. A model-guided process evaluation: Office-based prescribing and pharmacy dispensing of methadone. Evaluation and Program Planning 31, 376–381. 10.1016/j.evalprogplan.2008.04.011 [DOI] [PubMed] [Google Scholar]
- Walmart, n.d. Store Finder [WWW Document]. Walmart.com. URL https://www.walmart.com/store/finder?location=06510&distance=50 (accessed 5.22.20).
- ZipCode.org - Zip Codes for USA [WWW Document], n.d. URL https://zipcode.org/ (accessed 5.22.20).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.