Figure 6.
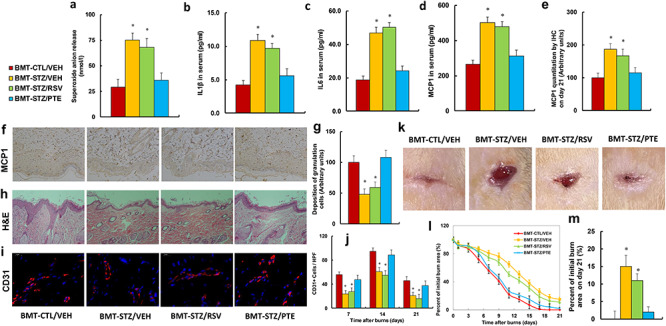
BMT of PTE-treated diabetic HSCs accelerates diabetic wound healing by ameliorating diabetes-induced oxidative stress and inflammation. Experimental rats were randomly separated into 4 groups as follows: rats with BMT of HSCs from CTL/VEH (BMT-CTL/VEH); rats with BMT of HSCs from STZ/VEH (BMT-STZ/VEH); rats with BMT of HSCs from STZ/RSV (BMT-STZ/RSV); and rats with BMT of HSCs from STZ/PTE (BMT-STZ/PTE). The rats were subjected to a model of cutaneous burn injury and the wound-healing process was evaluated, followed by biomedical analysis. (a) Superoxide anion release from wound tissues, n = 5. (b) IL1β in serum, n = 5. (c) IL6 in serum, n = 5. (d) MCP1 in serum, n = 5. (e) MCP1 quantitation by IHC from wound tissues on day 21, n = 5. (f) Representative pictures for (e). (g) Deposition of granulation cells from (h), n = 8. (h) H&E staining of wound tissues on day 21 after burn injury with occurrence of granulation cells in the wounds. (i) Representative pictures for evaluation of vascularity (assessed by CD31 IHC) for (j). (j) Numbers of CD31-positive vessels per high-power field on day 21 after burn injury, n = 8. (k) Photographs of representative wounds on day 21 after burn injury. (l) Graphical depiction of wound areas on different days after burn injury, n = 8. (m) Quantitation of burn area on day 21, n = 8. For bars in graphs marked with an asterisk, p < 0.05 vs CTL/VEH group. Data are expressed as mean ± SEM. BMT bone marrow transplantation, PTE pterostilbene, HSCs hematopoietic stem cells, CTL control, VEH vehicle, STZ streptozotocin, RSV resveratrol, IL1β interleukin-1β, IL6 interleukin-6, MCP1 monocyte chemoattractant protein-1, IHC immunohistochemistry
