Figure 2. Summary of Reported Expert Ordering Patterns for Dementia with Lewy Body Diagnosis in the U.S.
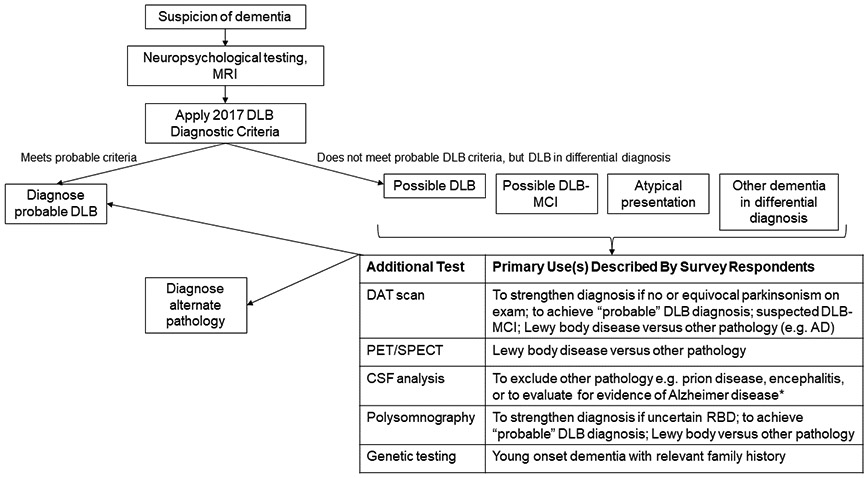
Most surveyed dementia with Lewy body (DLB) experts reported that neuropsychological testing and structural imaging are part of a routine dementia evaluation and the results (along with other history, examination) inform the assessment of potential DLB. Individuals who meet criteria for probable DLB often need no further work-up. Survey respondents indicated that they most commonly performed further testing for individuals presenting with “possible” DLB, mild cognitive impairment or atypical or uncertain presentations. This summary reflects U.S.-based expert ordering patterns and relevance to other clinical scenarios is uncertain.
*Testing for AD CSF biomarkers is performed more commonly for research than clinical purposes in the context of suspected DLB. Commercial AD assays are available for clinical care but are not always covered by insurance. A negative AD CSF assay result in the setting of possible DLB versus AD could help support a DLB diagnosis, but issues of assay standardization and limited knowledge of how these CSF analytes manifest in Lewy body disease are barriers for routine clinical use.
MRI: magnetic resonance imaging; DLB: dementia with Lewy bodies; MCI: mild cognitive impairment, DAT: dopamine transporter; AD: Alzheimer disease, PET: positron emission tomography, SPECT: single-photon emission computed tomography, CSF: cerebrospinal fluid, RBD: REM sleep behavior disorder
