Highlights
-
•
Peliosis lienalis is a rare pathological entity which may be associated with chronic myelomonocytic leukemia.
-
•
Increasing splenomegaly in patients with hematological malignancies should rise suspicion of impending splenic rupture.
-
•
Peliosis lienalis may be suspected with new inhomogeneous splenic parenchyma on sonography.
Abbreviations: CMML, chronic myelomonocytic leukemia; WHO, World Health Organization
Keywords: Splenic peliosis, Chronic myelomonocytic leukemia, Spontaneous splenic rupture, Case report
Abstract
Introduction
Atraumatic splenic rupture is a rare but life-threatening condition which may be associated with hematological malignancies.
Presentation of case
We present the case of a 63-year-old male patient with a history of chronic myelomonocytic leukemia and sarcoidosis under therapy with prednisone, who suffered an atraumatic splenic rupture with hemodynamic instability. He was managed with proximal splenic artery embolization and secondary open splenectomy. On pathology the diagnosis of peliosis lienalis was established.
Discussion
Peliosis is a rare pathological entity, which presents with multiple blood-filled cavities within parenchymatous organs and is of unknown etiology and pathogenesis. In retrospect a rapid increase in splenomegaly and inhomogeneous parenchyma of the spleen on sonography was realized.
Conclusion
Sonographic changes in size and parenchyma of the spleen in patients with hematological malignancies might help suspecting peliosis lienalis with impending splenic rupture and could alter clinical management towards a prophylactic splenectomy.
1. Introduction
Atraumatic splenic rupture is a rare entity with an estimated median age of 52 years [1]. In a systematic review of 845 patients the most frequent etiological groups were neoplastic, infectious and inflammatory non-infectious disorders [2]. The authors reported 24 patients with myeloproliferative disorders, 12 with myelodysplastic syndromes and 18 with peliosis lienalis as underlying etiologies [2]. Peliosis is a rare pathological entity, which presents with multiple blood-filled cavities within parenchymatous organs [3].
We found one case report, which described an 62-year-old male with an untreated chronic myelomonocytic leukemia (CMML) who suffered from an atraumatic splenic rupture in the context of a peliosis lienalis [4]. Our report adds sonographic appearance and dynamic of splenomegaly prior to the splenic rupture in a patient with CMML and peliosis lienalis on histopathological examination. These novel sonographic findings could influence clinical management towards a closer observation or a prophylactic splenectomy. Our patient was treated in a community hospital and the manuscript was prepared in accordance with the Surgical CAse REport (SCARE) guidelines [5,6].
2. Presentation of case
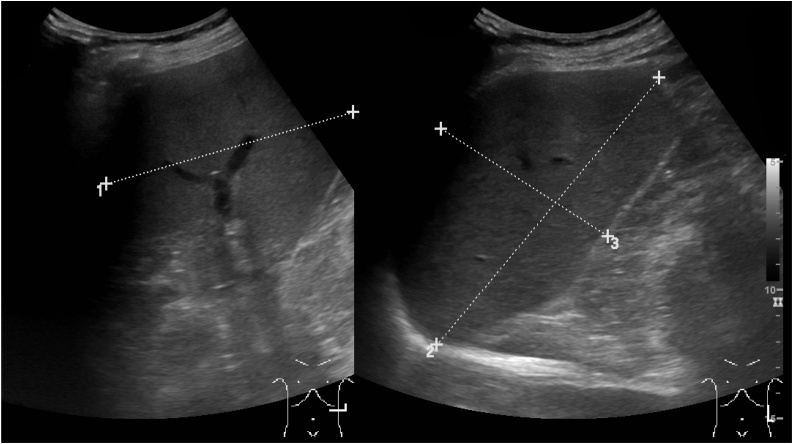
A 63-year-old white male patient was brought to our Emergency Department by ambulance with a sudden-onset neck pain followed by two episodes of a collapse at home. He did not report any fever, abdominal pain or trauma. The patient suffered from CMML-0 (<5% blasts in the bone marrow) without need for treatment. Abdominal sonography performed one-month prior showed a progressive splenomegaly (from 14 to 16 cm in length within seven months, Fig. 1) and a new inhomogeneous splenic parenchyma with small hypoechogenic lesions (Fig. 2). On further medical history, sarcoidosis was known and under treatment with 7.5 mg of prednisone. Due to an atrial fibrillation the patient was taking apixaban.
Fig. 1.
Sonography of the spleen eight months prior to the splenic rupture demonstrating normal parenchyma and a size of 10 × 14 × 8 cm.
Fig. 2.
Sonography of the spleen two months prior to the atraumatic-pathological splenic rupture. Several hypoechogenic small areas were newly present.
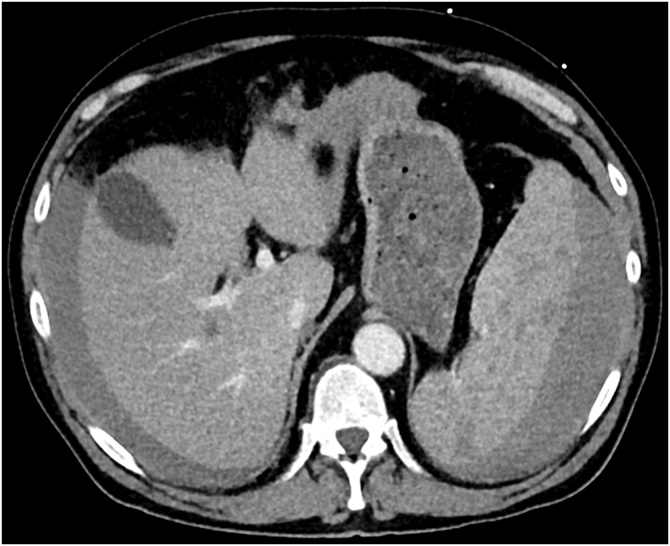
The patient presented afebrile with a blood pressure of 78/43 mmHg and a heart rate of 96/min. On examination we found a ballooned abdomen without signs of peritonitis. The computed tomography showed several hypodense lesions within the spleen and contrast blushes, which were interpreted as splenic rupture with ongoing bleeding (Fig. 3). Emergent diagnostic angiography revealed no active bleeding but a large subcapsular splenic hematoma. A selective embolization was not possible and therefore a proximal splenic artery embolization was performed. Five days after the embolization an open splenectomy was performed showing three liters of clotted blood within the abdominal cavity.
Fig. 3.
Contrast-enhanced axial abdominal computed tomography showing free fluid around the liver and the inhomogeneous splenic parenchyma.
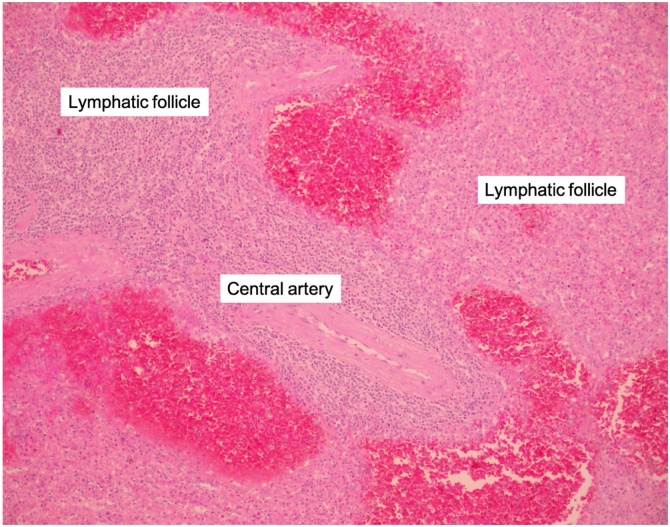
Pathology demonstrated a 19 × 14 × 6 cm 890 g spleen with multiple ruptures of the capsule. The cut surface revealed multiple well-demarcated round to oval, blood-filled cavities of about 40 cavities of 0.3 mm–3 mm per cm2, evenly distributed throughout the parenchyma (Fig. 4). They were preferentially located in the parafollicular zones, adjacent to periarteriolar lymphoid sheaths, and may be surrounded by white pulp. They lacked an endothelial lining (Fig. 5). There were no signs of locally bound immune complexes, leukemic tissue or sarcoidosis.
Fig. 4.
Histological section with multiple evenly distributed blood-filled cavities of about 0.5 to 3 mm; and some 40 per cm2.
Fig. 5.
Histopathology of a peliotic lesion of a blood-filled cavity around a lymphatic follicle with the central artery. Inset: Immunohistochemistry with CD34 antibodies revealing the absence of an endothelial lining of the blood-filled cavity (arrow heads).
The postoperative course was uneventful and we discharged the patient after 13 days in hospital. The sonography one year after the splenectomy showed no signs of a peliosis of the liver. One and a half years after the splenectomy the bone marrow showed progressive blasts with 16% and therefore a progression to a CMML-2 (defined as 10–19% blasts in the bone marrow) was diagnosed and a treatment with azacitidine started. At this point the patient presented with arthralgias due to the sarcoidosis without any other symptoms.
3. Discussion
Peliosis was first described in the liver in 1861 by Wagner [7]. To describe the appearance of the liver section surface, the Greek word “pelios” was inaugurated, meaning “black-bluish with suggillation”. The exact etiology is unknown and pathogenesis of peliosis is speculated to be underlying vascular malformations that are made apparent by local alterations of vascular pressure [8]. Another hypothesis is a focal cell necrosis that leads to destruction of the reticulum framework, which allows cyst-formations from the inflow of blood from adjacent sinusoids [9]. The first description of peliosis of the spleen was by Cohnheim in 1866 [10]. Associations of peliosis were described with hematologic neoplasms [4,11], cirrhosis [12] or in patients who have been received anabolic androgenic steroids [13]. But peliosis lienalis is also described without any comorbidities [14]. Gugger and Gebbers reported immune complexes at the margin of the lesions for the first time in two patients [15]. One of the women was under long-term treatment with steroids. However, we could not display any immune complexes although our patient was under a minimal steroid dose. In our case an association with the CMML is possible. By the revised 2016 World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia, CMML is classified as a clonal hematopoietic stem cell disorder with features of both myelodysplastic or myeloproliferative neoplasms [16]. In a cohort of 373 patients with 2016 WHO-defined CMML the median patient age was 71 years with a male dominance of 66% [17]. A palpable hepato- and/or splenomegaly was frequent (27%), and an isolated splenomegaly was present in 14%. However, the rate of atraumatic splenic rupture in CMML is low and described in case reports [4,18,19]. A retrospective study of 555 patients with CMML demonstrated a 7% rate of splenectomy in the time period from 1980 until 2018 [20]. In 8 (21%) patients the indication was a splenic rupture with six atraumatic and two traumatic ruptures. Peliosis lienalis as the cause for an atraumatic rupture in the context of a diagnosed CMML is even rarer. We found only one report of a 62-year-old man with CMML and splenomegaly. The 800 g splenectomy specimen showed a large subcapsular hematoma and evenly distributed 3−40 mm cyst-like spaces filled with fresh or clotted blood which led to the diagnosis of peliosis lienalis [4].
The diagnosis of peliosis lienalis before histopathology is rarely possible. However, certain changes within the spleen on sonography or computed tomography could rise a suspicion [21]. In our case, there was a change noted within the splenic parenchyma a month prior to the rupture (Fig. 1, Fig. 2). This sonographic finding together with a progressive splenomegaly in patients with CMML have not been published before and we believe that this could alter the management of these patients towards more frequent observation or prophylactic splenectomy.
4. Conclusion
In conclusion, we would like to stress the differential diagnosis of peliosis lienalis in patients with atraumatic splenic rupture. A progression of splenomegaly with inhomogeneous parenchyma on sonography in patients with hematological malignancies could be an early hint of a peliosis lienalis with impending rupture.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
No funding.
Ethical approval
This type of study does not require any ethical approval by our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Registration of research studies
Not applicable.
Guarantor
Lukas Werner Widmer.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Lukas Werner Widmer: Conceptualization, Investigation, Writing - original draft, Visualization. David Ardüser: Investigation, Writing - review & editing. Rebecca Kraus: Conceptualization, Writing - review & editing, Supervision. Jan-Olaf Gebbers: Resources, Writing - original draft, Visualization. Peter Villiger: Writing - review & editing, Supervision.
Acknowledgements
We acknowledge the Department of Radiology and the Institute of Pathology at the Cantonal Hospital Graubünden for the provision of the figures.
References
- 1.Elvy A., Harbach L., Bhangu A. Atraumatic splenic rupture: a 6-year case series. Eur. J. Emerg. Med. 2011;18:124–126. doi: 10.1097/MEJ.0b013e32833ddeb5. [DOI] [PubMed] [Google Scholar]
- 2.Renzulli P., Hostettler A., Schoepfer A.M., Gloor B., Candinas D. Systematic review of atraumatic splenic rupture. Br. J. Surg. 2009;96:1114–1121. doi: 10.1002/bjs.6737. [DOI] [PubMed] [Google Scholar]
- 3.Tsokos M., Erbersdobler A. Pathology of peliosis. Forensic Sci. Int. 2005;149:25–33. doi: 10.1016/j.forsciint.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Diebold J., Audouin J. Peliosis of the spleen. Report of a case associated with chronic myelomonocytic leukemia, presenting with spontaneous splenic rupture. Am. J. Surg. Pathol. 1983;7:197–204. http://www.ncbi.nlm.nih.gov/pubmed/6344667 [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A., Thoma A., Bashashati M., Vasudevan B., Beamish A., Challacombe B., De Wilde R.L., Machado-Aranda D., Laskin D., Muzumdar D., D’cruz A., Manning T., Healy D., Pagano D., Goel P., Ranganathan P., Pai P.S., Raja S., Ather M.H., Kadioäžlu H., Nixon I., Mukherjee I., Gómez Rivas J., Raveendran K., Derbyshire L., Valmasoni M., Chalkoo M., Raison N., Muensterer O., Bradley P., Roberto C., Afifi R., Rosin D., Klappenbach R., Wynn R., Giordano S., Basu S., Surani S., Suman P., Thorat M., Kasi V. The SCARE 2018 Statement: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2018 doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., De Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K., Kasivisvanathan V., Mei Z. The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Wagner E. Ein Fall Von Blutcysten in der leber. Arch. Heilkd. 1861;2:369–370. [Google Scholar]
- 8.Vignaux O., Legmann P., De Pinieux G., Chaussade S., Spaulding C., Couturier D., Bonnin A. Hemorrhagic necrosis due to peliosis hepatis: imaging findings and pathological correlation. Eur. Radiol. 1999;9:454–456. doi: 10.1007/s003300050691. [DOI] [PubMed] [Google Scholar]
- 9.Bagheri S.A. Peliosis hepatis associated with androgenic-anabolic steroid therapy. Ann. Intern. Med. 1974;81:610. doi: 10.7326/0003-4819-81-5-610. [DOI] [PubMed] [Google Scholar]
- 10.Cohnheim J. Tod Durch Berstung Von Varicen Der Milz. Virchows Arch. A Pathol. Anat. 1866;37:413–415. [Google Scholar]
- 11.Warfel K.A., Ellis G.H. Peliosis of the spleen. Report of a case and review of the literature. Arch. Pathol. Lab. Med. 1982;106:99–100. http://www.ncbi.nlm.nih.gov/pubmed/7036940 [PubMed] [Google Scholar]
- 12.Tsokos M., Püschel K. Isolated peliosis of the spleen. Am. J. Forensic Med. Pathol. 2004;25:251–254. doi: 10.1097/01.paf.0000127401.89952.65. [DOI] [PubMed] [Google Scholar]
- 13.Hirose H., Ohishi A., Nakamura H., Sugiura H., Umezawa A., Hosada Y. FATAL SPLENIC RUPTURE IN ANABOLIC STEROID- induced PELIOSIS in a patient with Myelodysplastic Syndrome. Br. J. Haematol. 1991;78:128–130. doi: 10.1111/j.1365-2141.1991.tb04398.x. [DOI] [PubMed] [Google Scholar]
- 14.Rhu J., Cho J. Ruptured splenic peliosis in a patient with no comorbidity: a case report. World J. Clin. Cases. 2020;8:535–539. doi: 10.12998/wjcc.v8.i3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gugger M., Gebbers J.O. Peliosis of the spleen: An immune-complex disease? Histopathology. 1998;33:387–389. doi: 10.1046/j.1365-2559.1998.00493.x. [DOI] [PubMed] [Google Scholar]
- 16.Arber D.A., Orazi A., Hasserjian R., Borowitz M.J., Le Beau M.M., Bloomfield C.D., Cazzola M., Vardiman J.W. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–2406. doi: 10.1182/blood-2016-03-643544.The. [DOI] [PubMed] [Google Scholar]
- 17.Hoversten K., Vallapureddy R., Lasho T., Finke C., Ketterling R., Hanson C., Gangat N., Tefferi A., Patnaik M.M. Nonhepatosplenic extramedullary manifestations of chronic myelomonocytic leukemia: clinical, molecular and prognostic correlates. Leuk. Lymphoma. 2018;0:1–4. doi: 10.1080/10428194.2018.1452212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goddard S.L., Chesney A.E., Reis M.D., Ghorab Z., Brzozowski M., Wright F.C., Wells R.A. Pathological splenic rupture: a rare complication of chronic myelomonocytic leukemia. Am. J. Hematol. 2007;82:405–408. doi: 10.1002/ajh.20812. [DOI] [PubMed] [Google Scholar]
- 19.Jiménez Herráez M.C., Larrocha Rabanal C., Fernández de Castro M., Viloria Vicente A. [Pathological rupture of the spleen in a case of chronic myelomonocytic leukemia] Sangre (Barc). 1991;36:168. http://www.ncbi.nlm.nih.gov/pubmed/1866659 [PubMed] [Google Scholar]
- 20.Pophali P., Horna P., Lasho T.L., Finke C.M., Ketterling R.P., Gangat N., Nagorney D., Tefferi A., Patnaik M.M. Splenectomy in patients with chronic myelomonocytic leukemia: indications, histopathological findings and clinical outcomes in a single institutional series of thirty-nine patients. Am. J. Hematol. 2018 doi: 10.1002/ajh.25246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davidson J., Tung K. Splenic peliosis: an unusual entity. Br. J. Radiol. 2010;83:126–128. doi: 10.1259/bjr/71300465. [DOI] [PMC free article] [PubMed] [Google Scholar]