Abstract
Purpose
Percutaneous trans-pedicle screws represent a surgical option frequently performed in patients affected by thoracolumbar vertebral burst fractures (A3-A4). The aim of the study was to evaluate the early loss of kyphosis correction and its clinical correlations in a cohort of patients affected by burst spinal fracture treated with percutaneous trans-pedicle screws fixation.
Methods
The present investigation consists in a retrospective one center analysis. The primary outcome was the evaluation of the early loss of correction. Secondary outcomes were the bi-segmental kyphosis change, the clinical outcome and the correlation between clinical outcome and the loss of correction.
Results
Among 435 patients 97 were included in the study. A mean 3.3° of early loss of correction was observed between postoperative and 1 month follow-up evaluations. The mean anterior vertebral body height change was 3.8 mm. No statistical differences were found in clinical and functional outcomes between patients with >2° or <2° of kyphosis loss of correction.
Conclusion
No statistical differences were found between 1 e 6 months postoperative kyphosis loss of correction. The amount of loss of correction seems not to influence clinical outcomes after percutaneous trans-pedicle screw fixation in patients with vertebral burst fractures.
Keywords: Percutaneous pedicle screw fixation, Thoracolumbar fracture, Vertebral height, Vertebral kyphosis, Loss of correction
1. Introduction
Thoracolumbar burst fractures (TLBF) are nearly 60%1, 2, 3 of all spinal traumatic injuries affecting vertebral body anterior and middle columns.4 They occur mostly in young patients involved in motor vehicle or fall accidents. These fractures are often associated with kyphotic deformity and spinal canal encroachment.
The finest treatment for thoracolumbar type A fractures according to Magerl Classification,5 is still controversial. Many reviews and meta-analyses on surgical approaches have been issued, however no consensus exists in patients with incomplete (A3) and complete (A4) TLBF.6,7 Given the lack of neurological deficit and instability, the literature suggests that vertebral fracture can be treated conservatively. Although the latter approach has shown promising results, clinical practice revealed that surgical treatment leads to a better fracture reduction and long-term clinical outcomes.5,8
Since the introduction of the Posterior Transpedicular Screw Fixation (PTSF) system in the lasts decades, good radiologic and clinical outcomes have been reported. This surgical technique includes pedicle screw fixation one level proximal and one level caudal the fracture. Previous studies proved that minimally invasive surgery (MIS) not only reduces the iatrogenic tissue damage but also gives similar mechanical stability achieved with an open procedure.9 MIS consents also the correction of kyphotic deformities, early painless mobilization, and indirect decompression of the spinal canal.10, 11, 12, 13 However McLain et al.14 sustained that the kyphotic deformity correction represents an hot topic so that, even with a low degree of kyphosis some patients complained of discomfort or showed functional loss. No study in the Literature evaluated the timing of kyphosis los of correction after percutaneous PTSF. Therefore, the aim of the study was to evaluate the early loss of kyphosis correction and its clinical correlations in a cohort of patients affected by burst spinal fracture treated with percutaneous PTSF.
2. Materials and methods
2.1. Study design
The present investigation consists in a retrospective analysis on patients with burst vertebral fractures referred to the authors Emergency Department from January 2010 to November 2019, and treated with percutaneous pedicle screws fixation. The study respects national ethical standards and the Helsinki Convention. This research has been approved by the IRB of the authors’ affiliated institutions. Written informed consent for scientific purposes and clinical data collection was obtained according to institutional protocol.
2.2. Institutional database and data collection
Patients triaged for spinal injury at our Emergency Department were managed with a standardized data collection system. Demographic, clinical and radiographic data (age, sex, BMI, anamnestic records, Frankel score,15 type of vertebral fracture according AO spine classification,16 pain assessment) were registered for each patient. All patients surgically treated were clinically and radiographically (standard AP and lateral views X-Ray in standing position) evaluated postoperatively (2 days after surgery), 1 and 6 months after surgery, according to our institutional protocol. In all radiographs stored on Picture archiving and communication system (PACS) powered by Carestream Clinic Imaging Solutions, were calculated: the vertebral wedge angle (VWA) and the anterior vertebral body height (ABVH) of the fractured vertebra. The bi-segmental kyphosis change on the treated level was also evaluated through Cobb Angle (CA) measurement. Three experienced vertebral surgeon (M.G., G.Z. and D.A.S.) performed the above mentioned measurements. Clinical evaluation in all follow up visits was assessed by Oswestry Disability Index (ODI) and Visual analogue scale (VAS).
2.3. Participants and eligibility criteria
Patients with a type A3 and A4 vertebral fracture with indication for percutaneous PTSF treatment were potentially eligible for the study in a period between January 2015 and November 2019.
Inclusion criteria were: (I) Fractured vertebral between T11 and L2; (II) Bi-segmental dorsal stabilization; (III) Absence of neurological impairment (Frankel grade E); (IV) time between trauma and surgery minor than 7 days.
Exclusion criteria were: (I) Metastatic and/or primary vertebral lesions; (II) Previous spinal surgery; (III) Rheumatic diseases (e.g. ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis); (IV) Postoperative spinal infections; (V) Osteoporotic fractures; (VI) Multilevel fractures.
2.4. Surgical technique
All patients enrolled in the study were treated by a single surgical team in prone position and in general anesthesia. Fracture reduction and kyphosis correction were obtained due to hyperextension during patient positioning and verified with lateral view radiograph before surgery. Two minimal invasive system, Viper 2 (DePuy Synthes) and Precept (Nuvasive, San Diego, CA, US) were used. Fluoroscopy guidance was used to identify the correct entry point in the antero-posterior (AP) view. Four small incisions were made. A guide wire was placed through the pedicle under fluoroscopic guidance. A cannulated screw was inserted then following the wire direction until reaching the medial edge of the pedicle in the AP view. Consequently, the screw direction was verified using the lateral view. A further correction of the angular kyphosis at the fracurated level was obtained pre-banding the rod and by in situ compression and extension maneuvers during inners locking (Fig. 1).
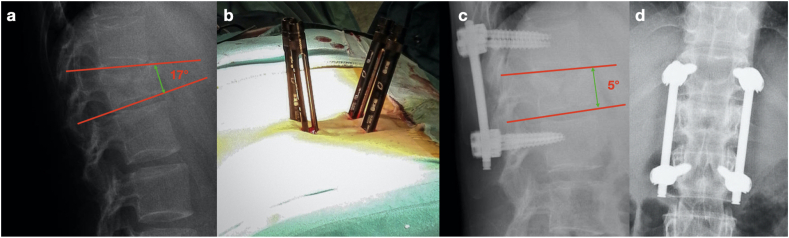
Fig. 1.
a, Lateral view spinal X-ray of a patient with L1 burst fracture and an angular Kyphosis of 17°. b. intraoperative images of percutaneous pedicle screws fixation. c,d postoperative Lateral view and antero-posterior view spinal X-Ray images showing 12° kyphotic deformity improvement.
2.5. Variables
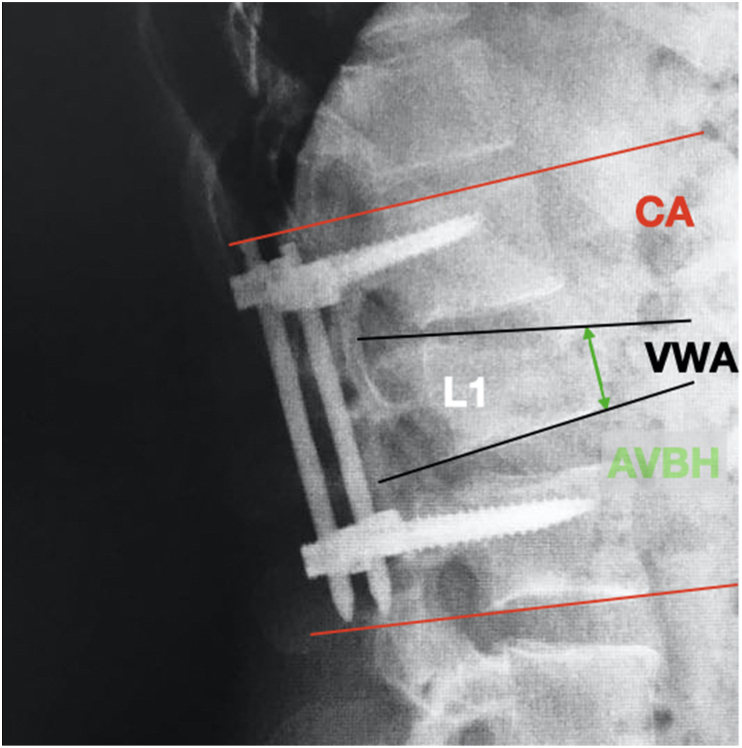
The primary outcome was the evaluation of early loss of correction (ELC, between postoperative and 1 month follow up standard X Ray) in term of angular kyphosis measured by VWA and AVBH of the fractured vertebra. Secondary outcomes were the bi-segmental kyphosis change measured by CA (Fig. 2), the clinical and functional outcomes during follow up visit and the correlation between clinical outcomes and the loss of correction.
Fig. 2.
Measurement of radiographic parameters on lateral views standard spinal X-Ray in a patient with L1 burst fracture. CA: Cobb Angle, VWA: Vertebral Wedge Angle, AVBH: Anterior Vertebral Body Height.
2.6. Statistical analysis
The Mann–Whitney U test for two independent ordinal variables. The Wilcoxon Signed-Rank Test was used for two dependent ordinal variables. The inter-rater reliability (IRR) between the three evaluators was calculated using a Fleiss’ kappa statistic. The significance was established for a value of p < 0.05. Dedicated software (GraphPad Software - Prism 8 for Mac) was employed. Only one decimal digit was reported, rounded up.
3. Results
3.1. Patients
Among all 435 patients treated only 97 were eligible for the study according inclusion and exclusion criteria and had a complete radiographic documentation. Mean age was 54.3 ( ±16.3) years. The male/female ratio was 1.1 (M:46; F:42). Within the 88 included patients, 30 (33.9%) were polytrauma. The injury mechanisms was traffic accident in 57 patients (64.4%), high falling injury in 17 cases (19.2%) and other causes in 14 patients (16.4%). Patient's features were reported in Table 1.
Table 1.
Patients data.
| Demographics | |
|---|---|
| Age | 54.3 ( ±16.3) |
| Sex | M:46; F:42 |
| BMI | 26.2, ±0.9 |
| Diabetes | 11, 12,4% |
| Smokers | 37, 41,8% |
| Other comorbidities | 27, 30.5% |
| Type of fracture (AO classification) | |
| A3 | 69, 77.9% |
| A4 | 19, 22.1% |
| Fractured Level | |
| D11 | 8, 9.2% |
| D12 | 50, 56.5% |
| L1 | 23,26.2% |
| L2 | 7, 8.1% |
| Polytrauma patients | 30, 33.9% |
| Associated lesions | |
| Long bone fractures | 21, 70% |
| Hepatic contusion | 4, 13.3% |
| Spleen rupture | 3, 10% |
| Pneumothorax | 5, 16.6% |
| Head injuries | 9, 30% |
| Traumatic mechanism | |
| Traffic accident | 57, 64.4% |
| High falling injury | 17, 19.2% |
| Other causes | 14, 16.4% |
3.2. Surgical results
In our series no intraoperative complications were found. Viper 2 (DePuy Synthes, Raynham, MA, US) and in Precept (Nuvasive, San Diego, CA, US) were used respectively in 43 (48.9%) and 45 cases (51,1%). The mean time between the trauma and surgery was 75±6 h. The mean operative time was 69.3 ( ±21.8) minutes. The mean x-ray exposure was 67±13 s. The mean blood loss was 120 ( ±71) ml. All screw placed were poly-axial. We did not observe hardware mobilization after the 6th month follow up. No patients needed additional anterior stabilization.
3.3. Radiological outcomes
VWA of the 88 vertebral fractures changed from mean preoperative value of 16.2 ( ±4.6)° to 7.4 ( ±3.1)° in the immediate postoperatively (p = 0.0041), to 10.7 ( ±2.8)° 1 month after surgery (p = 0.0373). AVBH changed from mean postoperatively value of 18.7( ±4.2) mm to 24.2. ( ±4.1) mm in the immediate postoperatively (p = 0.0029), to 20.4 ( ±3.7) mm 1 month after surgery (p > 0.05). No statistical differences were observed between 1 and 6 months. No statistical differences were noticed between treated levels kyphosis in all measurements (Table 2). All fractures were healed at 6 months follow up visit. The IRR was calculated using the Fleiss’ kappa (0.769, 95% CI: 0.663–0.887).
Table 2.
Radiological and clinical outcomes.
| Preoperative | Post op) | 1 m | 6 m | P value *,** value compared |
|
|---|---|---|---|---|---|
| VWA | 16.2( ±4.6)°* | 7.4 ( ±3.1)°*,** | 10.7 ( ±2.8)°** | 10.2 (±)3.3° | *p = 0.0041,**p = 0.0373 |
| AVBH | 18.7( ±4.2) mm* | 24.2. ( ±4.1) mm* | 20.4 ( ±3.7) mm | 19.7±2.9 mm | *p = 0.0029 |
| SK (CA) | 11.4( ±3.1)° | 9.1 ( ±5.9)° | 10.9( ±7.1)° | 10.9±3.6° | p > 0.05 |
| ODI | 78.1 ( ±16.7)* | 56.2 ( ±9.7) | 36.8±7.1 | 18.8 ( ±5.4)* | *p = 0.0132 |
| VAS | 8.7 ( ±1.2)* | 7.3 ( ±2.2) | 4.5( ±1.4) | 2.1(±0.9)* | *p = 0.002 |
VWA: Vertebral Wedge Angle, AVBH: Anterior Vertebral Body Height SK: Segmental Kyphosi, CA.
Cobb Angle; ODI: Oswestry Disability Index, VAS: Visual Analogue Scale.
3.4. Clinical and functional outcomes
All treated patients were mobilized one day after surgery wearing a three point Thoraco-Lumbo-Sacral Orthosis (TLSO). TLSO was used for 3 months. Mean hospital stay was 8,1 ( ±7.4) days. VAS score showed a progressive decreasing trend from preoperative measurement (8.7± 1.2) to 6 months follow up (2.1± 0.9) values (p = 0.002) (Table 2). The ODI improved from a pre-operative score of 78.1 ( ±16.7) to a postoperative score of 56.2 ( ±9.7) (p < 0.001), with a downward trend over all the follow up visits (36.8±7.1 and 18.8±5.4 respectively 1 and 6 months after surgery, p = 0.0132) (Table 2).
3.5. Subgroup analysis
Stratifying the treated patients based on the implanted instrumentation (Viper and Precept), no statistical differences were found regarding radiographical, clinical and functional evaluations.
The VWA increase was >2° within 1 and 6 months follow up X-Ray in 54 (61%) patients. However no statistical differences were observed in VAS and ODI values between patients with and without VWA increase >2°.
4. Discussion
Thoracolumbar junction fractures (TLJF) represents nowadays a frequent condition. Gold standard for surgical management of TLJF fracture site is still unclear. However for patients affected by TLJF with loss of vertebral height >50% and/or an angular kyphosis superior to 15°, a surgical correction of segmental sagittal alignment could be required.17 A conservative treatment could indeed lead to persistent inability and back pain as showed by Willen et al.18 The use of a percutaneous technique in emergency setting showed clear advantages in surgical bleeding control, early mobilization, less postoperative pain and scar formation. In one hand the segmental kyphosis correction after percutaneous PTSF seems to be comparable to open pedicle screw insertion technique,19 but in the other exposes the surgeon and the patient to a higher mean dose of radiation as showed by Kocis et al.20
Phan et al.21 in a recent meta-analysis compared patients undergoing open or percutaneous screw fixation after vertebral burst fractures and observed in these last: minor hospital stay and shorter operative time. In addition no differences were found in terms of postoperative kyphosis CA, VWA and AVBH. Many factors could influence the kyphotic loss of correction after percutaneous TPSF in patients with TLBF, including the elastic mechanical properties of the bone, discs, muscles, and instrumentation itself 22.
Sasso et al. 23 sustained that the loss of correction may be produced by the lack of anterior column reconstruction during posterior procedures, which cause high bending loads on the pedicle screws. In our series we observed an early mean VWA loss of 3.3° and a mean AVBH change of 3.8 mm while we did not observe a delayed loss of correction or structural failure due to the lack of bony fusion after 6 months. Nevertheless no statistical differences were found between patients with >2° or <2° VWA loss of correction in clinical and functional outcomes. In our opinion the widespread use of poly-axial screws in short construct is the main reason for early loss of correction. In fact the construct weakest link seems to be the screw-tulip junction (STJ) 24.
The stress resistance of the STJ has been thoroughly tested among constructs manufacturers so much that a specific stress/failure value was defined. Stanford et al. reported a variable load failure in their experimental model showing great discrepancy in the structural failure depending on the screws design 24,25. Despite the great advantage of poly-axial screw fixation in minimal invasive percutaneous surgery, we believe that the STJ static load failure should be considered when choosing an instrumentation for spinal trauma surgery.
4.1. Limitations
The present investigation had some limitations. In fact, we did not conduct a comparative study between percutaneous fixed monoaxial and poly-axial screws fixation systems. The present report was a retrospective monocentric study, therefore a observational multicenter study should be performed to corroborate our hypothesis. Another limitation could be the short follow up, but this condition is due to the study design aimed at investigating the ELC.
5. Conclusion
Thoracolumbar burst fractures can be effectively managed by a percutaneous fixation allowing early mobilization and faster recovery. No statistical difference were found between 1 e 6 months postoperative kyphosis loss of correction while the only statistical differences were found between postoperative and 1 month radiological evaluation. The observed loss of correction is in our opinion is not directly attributable to a lack of arthrodesis, therefore the stress resistance of the STJ of the chosen instrumentation should be carefully considered. The loss of VWA correction seems not to influence clinical outcomes after percutaneous PTFS in patients with vertebral burst fractures at 6 month follow up visit.
Compliance with ethical standards
All procedures performed were in accordance with the 1964 Helsinki declaration. This research has been approved by the IRB of the authors’ affiliated institutions. Written informed consent for scientific purposes and clinical data collection was obtained according to institutional protocol.
Funding
None.
Authors’ contributions
AP – conception, methodology, drafting, revision; MBB, DAS – drafting, editing, revision; GZ– conception, methodology, revision; LP – supervision, editing, revision; MG, FCT – methodology, drafting, revision, conception, supervision, editing
Declaration of competing interest
Authors declare that they have no conflict of interest.
Acknowledgements
None.
References
- 1.Leucht P., Fischer K., Muhr G., Mueller E.J. Epidemiology of traumatic spine fractures. Injury. 2009;40:166–172. doi: 10.1016/j.injury.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 2.Dai L.Y., Jiang L.S., Jiang S.D. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. a five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009;91:1033–1041. doi: 10.2106/JBJS.H.00510. [DOI] [PubMed] [Google Scholar]
- 3.Dai L.Y., Yao W.F., Cui Y.M., Zhou Q. Thoracolumbar fractures in patients with multiple injuries: diagnosis and treatment-a review of 147 cases. J Trauma. 2004;56:348–355. doi: 10.1097/01.TA.0000035089.51187.43. [DOI] [PubMed] [Google Scholar]
- 4.Denis F., Armstrong G.W., Searls K., Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984;189:142–149. [PubMed] [Google Scholar]
- 5.Magerl F., Aebi M., Gertzbein S.D., Harms J., Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 6.Verheyden A.P., Hölzl A., Ekkerlein H. Recommendations for the treatment of thoracolumbar lumbar spine injuries. Unfallchirurg. 2011;114:9–16. doi: 10.1007/s00113-010-1934-1. [DOI] [PubMed] [Google Scholar]
- 7.Rometsch E., Spruit M., Hartl R. Does Operative or nonoperative treatment achieve better results in A3 and A4 spinal fractures without neurological defcit? Systematic literature review with meta-analysis. Global Spine J. 2017;7:350–372. doi: 10.1177/2192568217699202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siebenga J., Leferink V.J., Segers M.J. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine. 2006;31:2881–2890. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 9.Tamburrelli F.C., Meluzio M.C., Burrofato A., Perna A., Proietti L. Minimally invasive surgery procedure in isthmic spondylolisthesis. Eur Spine J. 2018;27:237–243. doi: 10.1007/s00586-018-5627-8. [DOI] [PubMed] [Google Scholar]
- 10.Korovessis P.G., Baikousis A., Stamatakis M. Use of the Texas Scottish Rite Hospital instrumentation in the treatment of thoracolumbar injuries. Spine. 1997;22:882–888. doi: 10.1097/00007632-199704150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Shen W.J., Liu T.J., Shen Y.S. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine. 2001;26:1038–1045. doi: 10.1097/00007632-200105010-00010. [DOI] [PubMed] [Google Scholar]
- 12.Sjostrom L., Karlstrom G., Pech P., Rauschning W. Indirect spinal canal decompression in burst fractures treated with pedicle screw instrumentation. Spine. 1996;21:113–123. doi: 10.1097/00007632-199601010-00026. [DOI] [PubMed] [Google Scholar]
- 13.Proietti L., Scaramuzzo L., Schirò G.R., Sessa S., D'Aurizio G., Tamburrelli F.C. Posterior percutaneous reduction and fixation of thoraco-lumbar burst fractures. Orthop Traumatol Surg Res. 2014;100:455‐460. doi: 10.1016/j.otsr.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 14.McLain R.F., Sparling E., Benson D.R. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993;75:162–167. doi: 10.2106/00004623-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 15.van Middendorp J.J., Goss B., Urquhart S., Atresh S., Williams R.P., Schuetz M. Diagnosis and prognosis of traumatic spinal cord injury. Global Spine J. 2011;1:1‐8. doi: 10.1055/s-0031-1296049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schnake K.J., Schroeder G.D., Vaccaro A.R., Oner C. AOSpine classification systems (subaxial, thoracolumbar) J Orthop Trauma. 2017;31:S14‐S23. doi: 10.1097/BOT.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 17.Jiang W.Q., Ke Z.Y., Wu K., Chen X.L., Lou Z.Q. Effect of RTS versus percutaneous conventional pedicle screw fixation on type A thoracolumbar fractures: a retrospective cohort study. Eur Spine J. 2020 doi: 10.1007/s00586-020-06418-3. [DOI] [PubMed] [Google Scholar]
- 18.Willén J., Anderson J., Toomoka K., Singer K. The natural history of burst fractures at the thoracolumbar junction. J Spinal Disord. 1993;3:39‐46. [PubMed] [Google Scholar]
- 19.Tamburrelli F.C., Perna A., Proietti L., Zirio G., Santagada D.A., Genitiempo M. The feasibility of long-segment fluoroscopy-guided percutaneous thoracic spine pedicle screw fixation, and the outcome at two-year follow-up. Malays Orthop J. 2019;13:39‐44. doi: 10.5704/MOJ.1911.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kocis J., Kelbl M., Kocis T., Návrat T. Percutaneous versus open pedicle screw fixation for treatment of type A thoracolumbar fractures. Eur J Trauma Emerg Surg. 2020;46:147‐152. doi: 10.1007/s00068-018-0998-4. [DOI] [PubMed] [Google Scholar]
- 21.Phan K., Rao P.J., Mobbs R.J. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg. 2015;135:85‐92. doi: 10.1016/j.clineuro.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 22.Ricciardi L., Stifano V., Proietti L. Polli FM intraoperative and postoperative segmental Lordosis mismatch: analysis of 3 fusion techniques. World Neurosurg. 2018;115:e659–e663. doi: 10.1016/j.wneu.2018.04.126. [DOI] [PubMed] [Google Scholar]
- 23.Sasso R.C., Renkens K., Hanson D., Reilly T., McGuire R.A., Jr., Best N.M. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech. 2006;19:242–248. doi: 10.1097/01.bsd.0000211298.59884.24. [DOI] [PubMed] [Google Scholar]
- 24.Fogel G.R., Reitman C.A., Liu W., Esses S.I. Physical characteristics of polyaxial-headed pedicle screws and biomechanical comparison of load with their failure. Spine. 2003;28:470–473. doi: 10.1097/01.BRS.0000048652.45964.2E. [DOI] [PubMed] [Google Scholar]
- 25.Stanford R.E., Loefler A.H., Stanford P.M., Walsh W.R. Multiaxial pedicle screw designs: static and dynamic mechanical testing. Spine. 2004;29:367‐375. doi: 10.1097/01.brs.0000092369.50397.85. [DOI] [PubMed] [Google Scholar]