Abstract
COVID-19 has been associated with a hypercoagulable state and thrombotic events. Venous thromboembolism has been the most commonly reported type of thrombosis but also arterial thrombosis and disseminated intravascular coagulation in inpatients have been described frequently in several clinical experiences. Patients with COVID-19, because of its tendency to induce leucopenia and overlapping of bacterial infection, may experience sudden disseminated intravascular coagulation (DIC), as in the case that we report here. However, early diagnosis and treatment may be associated with positive resolution of these severe complications.
Keywords: COVID-19, DIC, sepsis, neutropenia, lymphocytopenia
1. Introduction
Coagulopathy with a trend towards a hypercoagulable state and thrombotic complications has been described since the first reports on COVID-19 were presented [1]. Disseminated intravascular coagulation (DIC) is an induced complication associated with several infections and it has been reported also as a complication in patients with COVID-19 [2]. DIC, in fact, occurs when the viral damage is associated with endothelial damage that may also induce ischemia of tissues and organs [3]. However, DIC is also a well-known complication of bacterial sepsis [4,5] that may be a consequence of viral infections and/or of immunodeficiencies such as lymphocytopenia or neutropenia [6,7,8]. SARS-CoV-2 is one virus which is able to induce lymphocytopenia [9], while neutropenia has been rarely reported [10].
We here report a case of a 63-year-old male who, during hospitalization for COVID-19, developed sudden neutropenia that induced bacterial sepsis and associated DIC.
2. Case History
LR, a 63-year-old male, required hospitalization for bilateral ground glass pneumonia due to SARS-CoV-2 infection (i.e., COVID-19). In the emergency room, he presented with fever and dyspnea, and a nasopharyngeal swab revealed positivity for SARS-CoV-2 infection; his laboratory values were typical of COVID-19, with an increase in C reactive protein (CRP), lactate deydrogenase (LDH), d-dimer, fibrinogen and with a reduced count of lymphocytes (Table 1). His treatment was based on full doses of systemic antibiotics (i.e., piperacilline-tazobactam 13.5 g daily; full doses of dexamethasone (i.e., 6 mg daily), prophylactic doses of enoxaparin (i.e., 4000 U daily), systemic intravenous fluconazole (i.e., 100 mg daily), oxygen therapeutic support with high-flow nasal cannula (HFNC)) [11]. The patient underwent this treatment without side effects for 10 days, with an improvement in his overall respiratory performance, improvement in pulse oximetry and regression of fever; his laboratory markers also revealed an improvement, as reported in Table 1, and Doppler ultrasound scan excluded deep vein thrombosis of the lower limbs.
Table 1.
Laboratory test results of described patient.
| Laboratory Test | Day 1 | Day 3 | Day 7 | Day 10 | Day 11 | Day 12 | Day 13 | Day 14 | Day 15 | Day 16 | Day 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| LDH (U/L) | 765 | 802 | 631 | 501 | 690 | 860 | 712 | 614 | 603 | 501 | 389 |
| CRP (mg/L) | 123 | 147 | 96 | 49 | 85 | 114 | 91 | 62 | 39 | 9 | 6 |
| Procalcitonin (ng/mL) | 0.31 | 0.26 | 0.19 | 0.16 | 1.5 | 2.3 | 1.9 | 1.1 | 0.8 | 0.6 | 0.2 |
| WBC (mmcube) | 13,150 | 14,200 | 9180 | 5691 | 1900 | 1400 | 4203 | 7802 | 9201 | 9650 | 9730 |
| Neutrophils | 11,980 | 13,000 | 8120 | 4260 | 1215 | 890 | 3120 | 6123 | 8123 | 8003 | 8115 |
| Lymphocytes | 900 | 850 | 750 | 906 | 650 | 500 | 790 | 990 | 900 | 1100 | 1110 |
| Platelets | 206 | 401 | 352 | 263 | 63 | 46 | 79 | 112 | 115 | 126 | 169 |
| Prothrombin time (INR) | 1.08 | 1.02 | 1.03 | 1.06 | 1.42 | 1.75 | 1.53 | 1.3 | 1.1 | 1.06 | 1.09 |
| Fibrinogen (mg/dL) | 612 | 602 | 630 | 590 | 260 | 202 | 301 | 402 | 289 | 302 | 236 |
| D-dimer (ng/dL) | 650 | 712 | 502 | 509 | 46,000 | 65,023 | 54,000 | 12,361 | 4526 | 2103 | 960 |
LDH: Lactate dehydrogenase; CRP: C reactive protein; WBC: white blood cells.
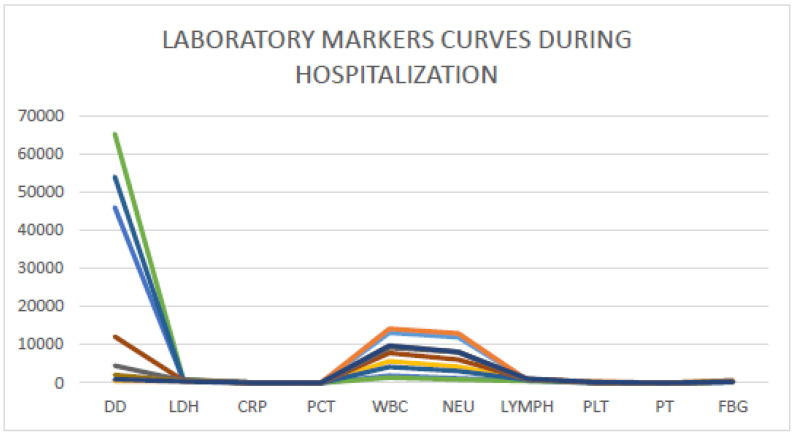
Starting from day 11, the patient experienced chills twice daily, with new occurrence of fever, and new laboratory screening revealed sudden neutropenia with associated increase in d-dimer (i.e., 56,000 mcg/dL) and decrease in platelets (i.e., 46.000 mmcube). CRP showed a new strong increase and also procalcitonin showed a relevant and pathological increase. Assessment of clinical signs and symptoms was repeated on the following day and laboratory data confirmed the previously observed trend (Table 1) (Figure 1). Furthermore, several blood cultures were performed while the patient was experiencing chills in order to detect bacterial sepsis but none of them identified a bacterial pathogen.
Figure 1.
Laboratory markers curves during the hospitalization of reported patients. DD: d-dimer; LDH: lactate dehydrogenase; CRP: C reactive protein; PCT: procalcitonin; WBC: white blood cells; NEU: neutrophils; LYMPH: lymphocytes; PLT: platelets; PT: prothrombin time; FBG: fibrinogen.
We implemented a withdrawal of enoxaparin and desamethazone and we began pulse therapy with intravenous 3 g methylprednisolone on the first day, 2 g on the second day and 1 g on the third, with an associated a single shot of subcutaneous growth colony factor lenograstrin (i.e., 34 Millions UI/mL daily) in order to improve the count of neutrophils. We also started treatment of DIC with 2 units twice daily of fresh frozen plasma for three consecutive days in order to restore induced coagulopathy and prevent microthromboses of tissues and organs.
From the first day of treatment, the patient showed a clinical improvements concerning chills and fever and progressive improvements were recorded in laboratory markers, as reported in Table 1 and Figure 1.
After three days of the new therapeutic approach, all treatments were interrupted (also antibiotics and antimycotics) and clinical surveillance was performed for two additional days; then, the patient was dismissed, with improved clinical condition with normal laboratory markers and with improved lung performance (Table 1) on day 17 of his hospitalization.
3. Discussion
DIC is always a consequence of another underlying disease or infection [12]. Bacterial sepsis is more frequently associated with DIC because the bacterial wall is able to induce hyperactivation of the clotting system by several mechanisms [4,5,12]; however, hyperactivation of the clotting system with a trend toward DIC has been described during viral infections of COVID-19 since the first reports were presented from China [1,2]. SARS- CoV-2 is able to induce a hypercoagulable state via cytokine storm [13] and the induction of the peptidase cascade as angiotensin-converting enzyme (ACE) as complement toward the kallikrein system, which may activate clotting factor XII and so the intrinsic pathway of coagulation [14,15,16]. The hyperaction of the peptidases and clotting system, present also in other forms of DIC, induces an increase in d-dimer and the progressive consumption of clotting factors until the decrease in fibrinogen and platelets results in multiple bleedings and shock.
On the other hand, SARS-CoV-2 may also induce alteration of white blood cells and lymphocytopenia has been frequently reported in the first phases of infection. However, in severe clinical forms of COVID-19, neutropenia is also described and neutropenia is frequent in febrile patients with bacterial sepsis for other reasons.
In the case that we reported, the occurrence of neutropenia was quickly followed by the clinical complications of DIC and systemic sepsis. The early identification of both complications permitted us to begin treatment rapidly for neutropenia and DIC with early restoration of all clinical and laboratory parameters including neutrophils, platelets and procalcitonin.
The management of this case may contribute to the improved clinical screening of patients with COVID-19 and associated DIC, because early identification and treatment could allow good outcomes following these severe complications.
Author Contributions
P.D.M., A.F., A.R., M.I. and L.F. managed the patient; P.D.M., A.F., D.I., M.R.P., C.S., G.L. analyzed the case history; L.I. performed laboratory tests and quality check. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of BUONCONSIGLIO FATEBENFRATELLI HOSPITAL OF NAPLES, ITALY.
Informed Consent Statement
Patient consent was waived.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tang N., Bai H., Xiong D., Sun Z. Specific coagulation markers may provide more therapeutic targets in COVID-19 patients receiving prophylactic anticoagulant. J. Thromb. Haemost. 2020;18:2428–2430. doi: 10.1111/jth.14988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seitz R., Schramm W. DIC in COVID-19: Implications for prognosis and treatment? J. Thromb. Haemost. 2020;18:1798–1799. doi: 10.1111/jth.14878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Semeraro N., Ammollo C.T., Semeraro F., Colucci M. Sepsis, thrombosis and organ dysfunction. Thromb. Res. 2012;129:290–295. doi: 10.1016/j.thromres.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Di Micco B., Metafora S., Colonna G., Cartenì M., Ragone R., Macalello M.A., Di Micco P., Baroni A., Catalanotti P., Tufano M.A. Porins from Salmonella typhimurium accelerate human blood coagulation in vitro by selective stimulation of thrombin activity: Implications in septic shock DIC pathogenesis. J. Endotoxin Res. 2001;7:211–217. doi: 10.1177/09680519010070030301. [DOI] [PubMed] [Google Scholar]
- 5.Di Micco B., Di Micco P., Lepretti M., Stiuso P., Donnarumma G., Iovene M.R., Capasso R., Tufano M.A. Hyperproduction of fibrin and inefficacy of antithrombin III and alpha2 macroglobulin in the presence of bacterial porins. Int. J. Exp. Pathol. 2005;86:241–245. doi: 10.1111/j.0959-9673.2005.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White L., Ybarra M. Neutropenic Fever. Hematol. Oncol. Clin. N. Am. 2017;31:981–993. doi: 10.1016/j.hoc.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Toma A., Fenaux P., Dreyfus F., Cordonnier C. Infections in myelodysplastic syndromes. Haematologica. 2012;97:1459–1470. doi: 10.3324/haematol.2012.063420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pagano L., Caira M. Risks for infection in patients with myelodysplasia and acute leukemia. Curr. Opin. Infect. Dis. 2012;25:612–618. doi: 10.1097/QCO.0b013e328358b000. [DOI] [PubMed] [Google Scholar]
- 9.Henry B.M. COVID-19, ECMO, and lymphopenia: A word of caution. Lancet Respir. Med. 2020;8:e24. doi: 10.1016/S2213-2600(20)30119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fu J., Kong J., Wang W., Wu M., Yao L., Wang Z., Jin J., Wu D., Yu X. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: A retrospective study in Suzhou China. Thromb. Res. 2020;192:3–8. doi: 10.1016/j.thromres.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Procopio G., Cancelliere A., Trecarichi E.M., Mazzitelli M., Arrighi E., Perri G., Serapide F., Pelaia C., Lio E., Busceti M.T., et al. Oxygen therapy via high flow nasal cannula in severe respiratory failure caused by Sars-Cov-2 infection: A real-life observational study. Ther. Adv. Respir. Dis. 2020;14:1–10. doi: 10.1177/1753466620963016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levi M., Sivapalaratnam S. Disseminated intravascular coagulation: An update on pathogenesis and diagnosis. Expert Rev. Hematol. 2018;11:663–672. doi: 10.1080/17474086.2018.1500173. [DOI] [PubMed] [Google Scholar]
- 13.Soy M., Keser G., Atagündüz P., Tabak F., Atagündüz I., Kayhan S. Cytokine storm in COVID-19: Pathogenesis and overview of anti-inflammatory agents used in treatment. Clin. Rheumatol. 2020;39:2085–2094. doi: 10.1007/s10067-020-05190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polycarpou A., Howard M., Farrar C.A., Greenlaw R., Fanelli G., Wallis R., Klavinskis L.S., Sacks S. Rationale for targeting complement in COVID-19. EMBO Mol. Med. 2020;12:e12642. doi: 10.15252/emmm.202012642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang X., Li S., Niu S. ACE2 and COVID-19 and the resulting ARDS. Postgrad. Med. J. 2020;96:403–407. doi: 10.1136/postgradmedj-2020-137935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoevenaar M., Goossens D., Roorda J. Angiotensin-converting enzyme 2, the complement system, the kallikrein-kinin system, type-2 diabetes, interleukin-6, and their interactions regarding the complex COVID-19 pathophysiological crossroads. J. Renin Angiotensin Aldosterone Syst. 2020;21:1470320320979097. doi: 10.1177/1470320320979097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.