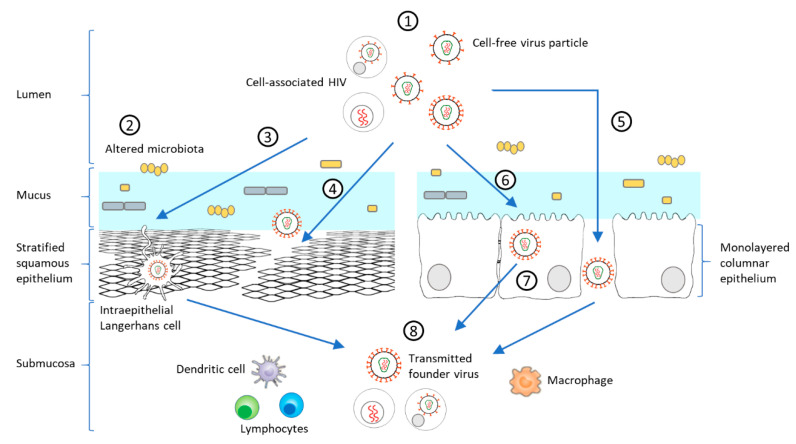
Figure 2.
Model of HIV-1 mucosal transmission. (1) Most HIV-1 infections begin at the rectal or genital mucosa, where infected fluid transmits the virus as cell-free virus particles or cell-associated forms (2) Among the risk factors facilitating mucosal transmission in the female genital tract, an altered microbiota, such as during bacterial vaginosis (BV) or sexually transmitted infections (STIs), can increase the anaerobic bacterial population, decreasing mucus pH and viscosity, and initiating a mucosal inflammatory response leading to disruption of the epithelial barrier. HIV-1 can pass through the epithelium via different mechanisms including (3) capture of intraepithelial LCs, (4) paracellular penetration following epithelium micro-laceration or (5) tight-junction disruption. (6) HIV-1 can also enter epithelial cells by micropinocytosis or endocytosis [89,90], which can lead to prolonged sequestration of the virus or a transient passage by transcytosis to the submucosa. (8) Following these different routes, HIV-1 can be present in the submucosa and exposed to immune target cells (lymphocytes, DCs, LCs, macrophages). Inflammatory responses heighten the recruitment of innate and adaptive immune cells, which promotes viral replication and dissemination [89,91,92,93]. These varied steps of mucosal transmission shape selection of the T/F virus.