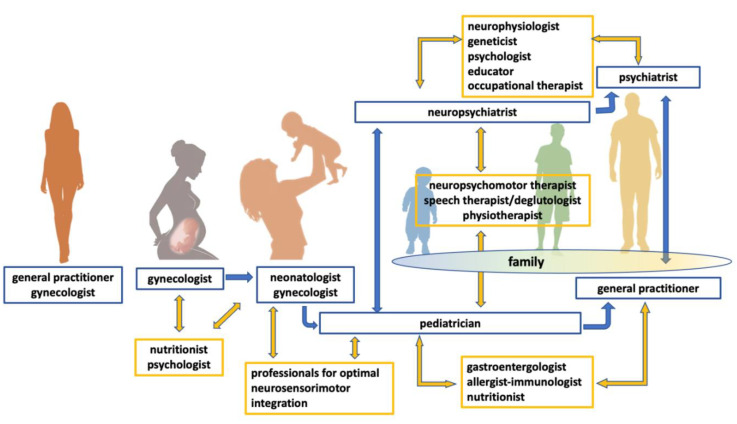
Figure 2.
Mother’s health is the premise for a successful intrauterine life. During pregnancy, the gynecologist ensures the best control of risk factors and the enhancement of protective factors, largely related to proper maternal nutrition and supplementation. After birth, the baby–mother dyad is supported by the neonatologist–gynecologist duo. The qualified support for the well-being of the mother is integrated by neonatal care, which includes the best conditions of neurosensory-motor integration aimed at the physiological postnatal neuronal wiring. With variable times and modalities—mostly depending on the outcome of the pregnancy and the characteristics of the newborn—the child’s care is subsequently entrusted to the pediatrician, who provides suggestions for a positive physical and neuro-psychomotor development. In case of clinical abnormalities, the pediatrician prompts diagnostic pathways and early interdisciplinary interventions based on clinical and laboratory findings. In the event of motor and/or socio-communicative abnormalities, the pediatrician consults the neuropsychiatrist, who shall consider whether to include standardized diagnostic tools for ASD in the clinical assessment. The diagnosis of ASD is followed by further diagnostic evaluations (neurophysiologist, geneticist), functional assessment, and timely psychoeducational evidence-based interventions. The neuropsychiatrist orchestrates the cooperation of numerous professionals (psychologist, educator, occupational therapist), monitors the results, and tailors the supports according to the evolving skills and needs. In parallel with the neuropsychiatrist, the pediatrician prompts a clinical assessment according to the expected comorbidities in ASD, involving in particular gastroenterologist, allergist-immunologist, and nutritionist. A close collaboration with the neuropsychiatrist allows the best integration of physical and neuropsychiatric aspects, involving at the same time professionals linked both to the pediatric and the neuropsychiatric sides. The transition towards adulthood requires a handover on both levels of intervention, from the pediatrician to the general practitioner for the biological features, and from the neuropsychiatrist to the psychiatrist for the psychiatric sphere. The connection between the two levels (body and mind) is maintained even in adulthood. It should be noted that the above described structured model acquires worth and meaning if it places in the center the person with ASD and his/her family, as the main stakeholders of a flexible model, able to adapt to the evolving needs and favoring the highest level of feasible well-being.