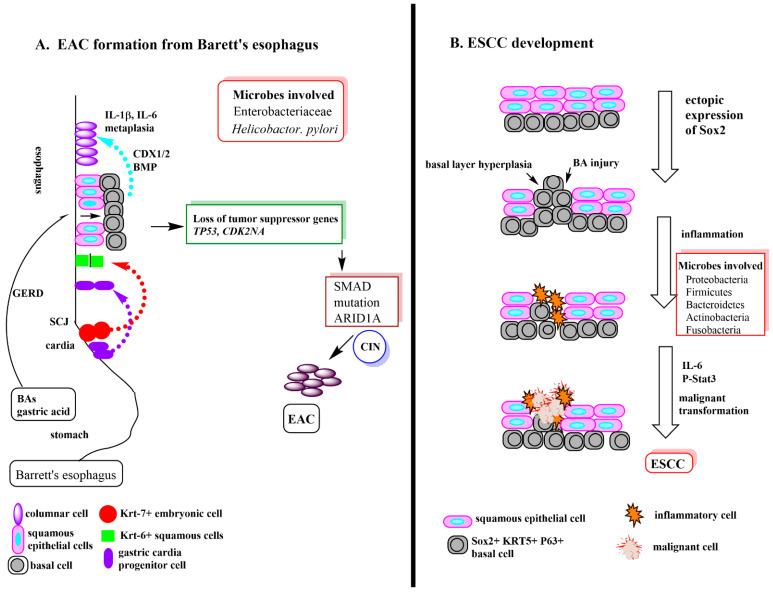
Figure 2.
(A) The formation of Barrett’s esophagus and transition to esophageal adenocarcinoma. There are several popular theories as to how Barrett’s esophagus is formed. The three most current are pictured diagrammatically in this figure. (1) The purple arrow indicates the migration of gastric cardia progenitor cells to the esophagus due to inflammation driven expansion of these cells. (2) The red arrow indicates the inflammation driven migration of Krt-7+ squamous epithelial cells at the SCJ junction to replace the normal Krt-6+ in the esophagus. (3) The blue arrow indicates what happens after GERD damage opens up squamous cell junctions and allow acid damage of the basal cells. In response to damage the basal cells express CDX1 and BMP to cause the basal cells to transform into metaplastic columnar cells along with further increased damage due to inflammation. Once Barrett’s esophagus is established, further inflammation induced damage of the columnar cells leads to cell mutations, notably, loss of tumor suppressor genes, TP53 and CDK2NA which in turn, increases mutation of SMAD (leads to dysregulated cell growth) and the expression of AT-rich interactive domain-containing protein 1A, ARID1A) (part of a protein complex responsible for activating genes normally silenced by chromatin structure). The final result is chromosome instability (CIN) and malignant transformation to EAC [19]. Abbreviations: AT-rich interactive domain-containing protein 1A (ARID1A), bile acid (BA), bone morphogenetic protein (BMP, growth factor), caudal homeobox gene 1 (CDX1), chromosomal instability (CIN), cyclin-dependent kinase inhibitor 2A (CDKN2A, tumor suppressor), esophageal adenocarcinoma (EAC), gastric acid esophageal reflux disease (GERD), interleukin (IL) (IL-1β, IL-6, inflammatory cytokines), squamocolumnar junction (SCJ), tumor protein 54 (TP53, tumor suppressor) (B) ESCC development. The development of esophageal squamous cell carcinoma (ESCC) begins with the ectopic expression of Sox2 in basal cells. Sox2 is critical for maintaining self-renewal and appropriate proportion of basal cells in adult tracheal epithelium. However, its overexpression gives rise to extensive epithelial hyperplasia. BA injury to basal cells leads to more basal cell hyperplasia and inflammation. Increased levels of the inflammatory cytokine, IL-6, and increased levels of activated P-Stat3 results in malignant transformation to ESCC. Abbreviations: Signal transducer and activator of transcription 3 (STAT3), SRY (sex determining region Y)-box 2 (Sox2) Reference for microbiota involvement [15].