Abstract
Pharyngeal teratomas are very rare congenital tumours derived from pluripotent stem cells. Surgical resection is the main treatment to avoid breathing and feeding difficulties. This current case report describes two newborn infants with congenital oropharyngeal teratomas. In one of the infants, the tumour presented along with a cleft tongue and cleft palate. Prenatal diagnosis by ultrasonography did not identify the tumours because the masses were small and there was no polyhydramnios. Both cases were treated surgically and histological examination of the masses in both cases confirmed the diagnosis of a congenital epignathus. There were no complications such as infection, bleeding or residual recurrence following surgery. After 1-year follow-up, there was no recurrence of the epignathus in either case. Oropharyngeal teratoma is a very rare congenital tumour that may cause upper airway obstruction and feeding difficulties in the newborn, so it should be treated surgically in a timely manner.
Keywords: Oropharyngeal teratoma, tongue cracking, cleft palate
Introduction
Tumours of the oral cavity and nasopharynx in the newborn are not common. An epignathus refers to a teratoma of the oropharyngeal region composed of cells from the ectodermal, mesodermal and endodermal layers, which is found in approximately 1:35 000–1:200 000 live births.1 Epignathi that arise from the palate or pharynx and protrude from the mouth can result in life-threatening airway obstruction and feeding difficulties. This current case report presents two cases of an epignathus arising from the oral cavity in newborn infants. The clinical characteristics, diagnosis and treatment of this rare disease are also reviewed.
Case report 1
A 29-year-old female patient (gravida 1, para 1) was admitted to the Shanghai Children’s Hospital, Shanghai Jiao Tong University, Shanghai, China at 38 weeks of gestation in June 2019. She gave birth vaginally to a boy (birth weight, 3750g). After birth, the neonate was noted to have a mass inside the oral cavity (Figure 1). Fortunately, the mass did not cause severe respiratory distress, but it did cause feeding difficulties. On further clinical examination, the mass in the oral cavity appeared polypoidal and was partly covered with skin. The shape of this mass looked like a human foot. The mass was accompanied by cleft tongue and cleft palate. Magnetic resonance imaging (MRI) showed a mixed density tumour in the oropharynx, which was probably attached to the palate. Computed tomography (CT) showed evidence of cleft palate (Figure 2). Transoral surgical excision of the tumour was subsequently performed on day 72. The tumour was identified, the posterior nasopharyngeal wall was dissected and the cleft tongue was repaired at the same time. Inspection revealed a cleft palate, which was rescheduled to be repaired at 1 year of age. Histological examination of the mass confirmed the diagnosis of a congenital epignathus. There were no complications such as infection, bleeding or residual recurrence following surgery. As shown by photographs taken at 1 day and 3 months postoperation, the child had recovered well and was able to feed normally. There were no feeding or breathing difficulties (Figure 3). After 1-year follow-up, there was no recurrence of the epignathus.
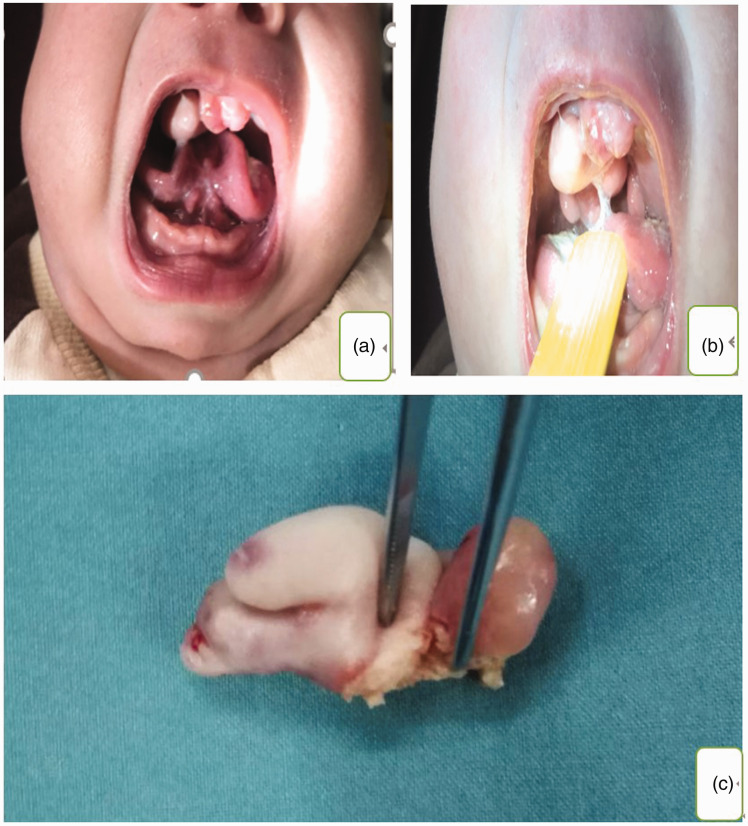
Figure 1.
Representative photographs showing a male newborn (case 1) with a cleft tongue (a) and a teratoma of the oropharynx in situ (b) and following resection during surgery (c). The colour version of this figure is available at: http://imr.sagepub.com.
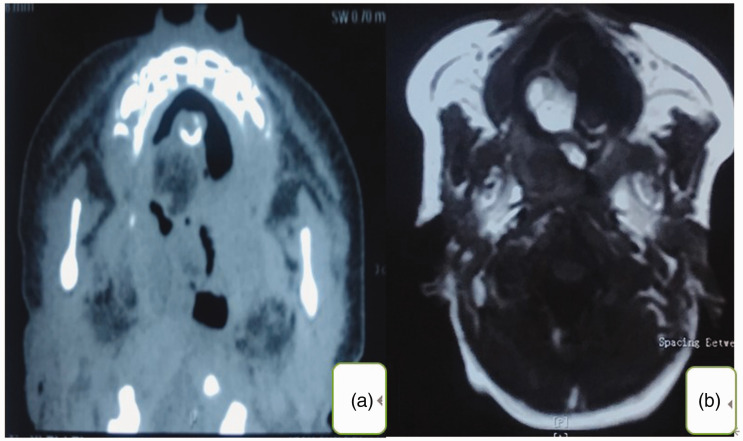
Figure 2.
Representative preoperative computed tomography (a) and magnetic resonance imaging (b) scans of a male newborn (case 1) with a teratoma of the oropharynx.
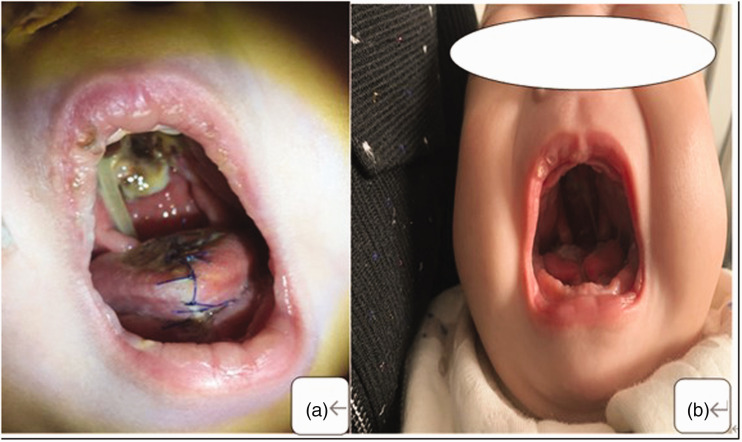
Figure 3.
Representative photographs showing a male infant (case 1) at 1 day (a) and 3 months (b) after the surgical removal of a teratoma of the oropharynx. The colour version of this figure is available at: http://imr.sagepub.com.
Case report 2
A prenatal ultrasound performed at 20 weeks of gestation in a 25-year-old female patient (gravida 1, para 1) revealed a fetus with an oral mass. In April 2019 at 38 weeks of gestation, the patient was admitted to the Shanghai Children’s Hospital and gave birth vaginally to a boy (birth weight, 3150g). At birth, a mass arose from the oropharynx. Fortunately, the mass did not cause severe respiratory distress, but it did cause feeding difficulties. A successful staged resection of an oropharyngeal teratoma was performed (Figure 4). Histological examination showed a mixed mature and immature (10%) true teratoma with no evidence of malignant changes. The diagnosis of a congenital epignathus was confirmed. There were no complications such as infection, bleeding or residual recurrence following surgery. After 1-year follow-up, there was no recurrence of the epignathus.
Figure 4.
Representative photographs showing a male newborn (case 2) with a mass arising from the oropharynx that protruded from the mouth (a) and the teratoma of the oropharynx that was subsequently surgically resected (b, c). The colour version of this figure is available at: http://imr.sagepub.com.
The clinical protocol used for both cases was established according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of Shanghai Children’s Hospital, Shanghai Jiao Tong University (no. [2019].5). The parents or legal guardians of the two cases provided written informed consent for publication of the clinical data and images presented in this case report.
Discussion
Teratoma is a common germ cell tumour in children, but the cause of teratoma remains unclear.2 It is commonly located in the midline of the body and the surrounding tissues.3 Teratomas usually occur in the sacrococcygeal, mediastinum, retroperitoneum, ovary and testis.4 The incidence rate of teratomas in newborns is 1:35 000–1:200 000.1 The incidence of oral pharyngoma accounts for approximately 2% of the total number of teratomas; and for 2.4% of all childhood oral jaw facial tumours.5 Teratomas can affect the face, pharynx, nose, eye socket, hard palate and neck.6 A review of the literature shows that the incidence of head and neck teratomas in children is equally distributed between the two sexes.7 According to the composition of the teratoma and the extent of the tissue maturity, teratomas are divided into the following categories: (i) benign teratomas; (ii) mixed teratomas containing undeveloped (embryonic) tissue; (iii) malignant teratomas.8 Benign and mixed teratomas have a tendency to become malignant.9 Neonatal pharynx teratomas are mostly benign, but the rate of malignancy increases with age,10 so once diagnosed, they need to be surgically removed as soon as possible. The purpose of surgical resection is to completely remove the tumour tissue and to correct any feeding difficulties and airway obstruction.
Neonatal pharyngeal teratomas are characterized by causing feeding difficulties or respiratory distress. The severity of the symptoms depends on the size and location of the tumour within the oral cavity. In these two current cases, each newborn had difficulty feeding immediately after birth. If the tumour is too large and deep in the posterior part of the tongue and parapharyngeal space, it can also compress the airway and cause airway obstruction.
Prenatal diagnosis is important because newborns that are born with pharyngeal teratomas that compress the airways can experience postnatal asphyxiation, brain damage and even death.5 It was observed in these current cases that if the tumour body was larger than the mouth, it was easy to identify it on prenatal ultrasound examination. However, if the tumour site was deeper, prenatal ultrasound may not be able to identify the tumour. Prenatal ultrasound examination is an essential and reliable method for identifying fetal oropharyngeal teratomas. Three-dimensional colour ultrasound can clearly show the relationship between the tumour and the oral space.11 Patients with congenital head and neck teratomas often have too much amniotic fluid.12 It is common to find excessive amniotic fluid, especially in children with large oropharyngeal teratomas.5 This phenomenon might be due to tumour compression blocking the pharynx and oesophagus, which in turn prevents the fetus from swallowing.13 MRI technology is being used more frequently in prenatal diagnosis. MRI can accurately diagnose fetal anatomical malformations, clarify the size and specific location of tumours, understand the anatomical relationship between the mass, trachea and oesophagus; and provide the necessary basis for evaluating the risk of delivery, enable careful surgical planning in the early stage and provide a prognosis.12 Preoperative CT examination of the oropharyngeal region is helpful for a differential diagnosis and to determine the extent of the tumour, to clarify the relationship between the tumour and peripheral nerves and blood vessels, and to make a comprehensive treatment plan.14 At present, the main method of prenatal diagnosis remains ultrasonography. Teratomas of the pharynx should be differentiated from lymphangioma, haemangioma, ectopic thyroid, salivary adenoma and cysts.
A caesarean section delivery is preferred for the fetus with a prenatal diagnosis of a pharynx tumour, because a large teratoma in the mouth and pharynx can cause complete airway obstruction. Fetal oxygenation is not affected during intrauterine placental circulation, but cord ligation during delivery may be fatal. Exutero intrauterine treatment (EXIT) can extend the placental circulation time, giving clinicians plenty of time to ensure that the airways are open, thus saving the child's life.15 It would appear to be feasible to use EXIT to perform tumour resection at the same time as the caesarean section, although the maintenance time of the placental circulation under EXIT may be less than 60 minutes.16 The survival rate for children may not be higher than 30–40%.17 However, the ability to resect the oropharyngeal tumour under EXIT has potential so should be investigated further. Effective perinatal intervention and timely surgery should improve the prognosis and survival rate of newborns with oropharyngeal tumours.
In conclusion, neonatal pharyngeal teratomas are rare and they are usually mature benign tumours. Early surgical intervention is still recommended,18 especially for teratomas that are causing an airway obstruction. Three-dimensional colour ultrasound, MRI and CT imaging can improve the accuracy of the prenatal diagnosis. Caesarean section delivery, multidisciplinary cooperation and EXIT might improve the survival and prognosis of newborns with oropharyngeal tumours.
Authors' contributions
P.Z. conceived the study, acquired, analysed and interpreted the data, provided final approval of the version of the manuscript to be published and agreed to be accountable for all aspects of the work; X.Y.L. acquired, analysed and interpreted the data, provided final approval of the version of the manuscript to be published and agreed to be accountable for all aspects of the work.
Footnotes
Declaration of conflicting interest: The authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Xiao-Yan Li https://orcid.org/0000-0001-6771-5586
References
- 1.Demajumdar R, Bhat N. Epignathus: a germ-cell tumour presenting as neonatal respiratory distress. Int J Pediatr Otorhinolaryngol 1999; 47: 87.–. [DOI] [PubMed] [Google Scholar]
- 2.Chiloiro S, Giampietro A, Bianchi A, et al. Clinical management of teratoma, a rare hypothalamic-pituitary neoplasia. Endocrine 2016; 53: 636–642. [DOI] [PubMed] [Google Scholar]
- 3.Paradis J, Koltai PJ. Pediatric teratoma and dermoid cysts. Otolaryngol Clin North Am 2015; 48: 121–136. [DOI] [PubMed] [Google Scholar]
- 4.Sertbaş İ, Karatay M. Enlarging teratoma syndrome. Childs Nerv Syst 2019; 35: 369–372. [DOI] [PubMed] [Google Scholar]
- 5.Celik M, Akkaya H, Arda IS, et al. Congenital teratoma of the tongue: a case report and review of the literature. J Pediatr Surg 2006; 41: E25–E28. [DOI] [PubMed] [Google Scholar]
- 6.Łuczak J, Bagłaj M. Ovarian teratoma in children: a plea for collaborative clinical study. J Ovarian Res 2018; 11: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parvin S, Sengupta M, Mishra PK, et al. Gastric teratoma: A series of 7 cases. J Pediatr Surg 2016; 51: 1072–1077. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Yin Y, Cai Z, et al. Pediatric pancreatic teratoma: A case report and literature review. Medicine (Baltimore) 2019; 98: e18001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carver BS, Al-Ahmadie H, Sheinfeld J. Adult and pediatric testicular teratoma. Urol Clin North Am 2007; 34: 245–251. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka Y, Koyama S, Shiki Y. Hand-assisted laparoscopic surgery for a mesenteric teratoma. JSLS 2014; 18: 160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiang YC, Shih JC, Peng SSS, et al. Tongue teratoma – a rare form of fetal extragonadal teratoma diagnosed at 30 weeks' gestation. Ultrasound Obstet Gynecol 2006; 28: 737–741. [DOI] [PubMed] [Google Scholar]
- 12.Vandenhaute B, Leteurtre E, Lecomte-Houcke M, et al. Epignathus teratoma: report of three cases with a review of the literature. Cleft Palate Craniofac J 2000; 37: 83–91. [DOI] [PubMed] [Google Scholar]
- 13.Tonni G, De Felice C, Centini G, et al. Cervical and oral teratoma in the fetus: a systematic review of etiology, pathology, diagnosis, treatment and prognosis. Arch Gynecol Obstet 2010; 282: 355–361. [DOI] [PubMed] [Google Scholar]
- 14.Lopes MA, Pereira CM, da Cruz Perez DE, et al. Benign teratoma of the buccal mucosa in a 9-year-old girl: report of case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100: 598–602. [DOI] [PubMed] [Google Scholar]
- 15.Ducloy-Bouthors AS, Marciniak B, Vaast P, et al. Maternal and foetal anaesthesia for ex utero intrapartum treatment (EXIT) procedure. Ann Fr Anesth Reanim 2006; 25: 638–643 [Article in French, English abstract]. [DOI] [PubMed] [Google Scholar]
- 16.Marwan A, Crombleholme TM. The EXIT procedure: principles, pitfalls, and progress. Semin Pediatr Surg 2006; 15: 107–115. [DOI] [PubMed] [Google Scholar]
- 17.Kontopoulos EV, Gualtieri M, Quintero RA. Successful in utero treatment of an oral teratoma via operative fetoscopy: case report and review of the literature. Am J Obstet Gynecol 2012; 207: e12–e15. [DOI] [PubMed] [Google Scholar]
- 18.Cardesa-Salzmann TM, Mora-Graupera J, Claret G, et al. Congenital cervical neuroblastoma. Pediatr Blood Cancer 2004; 43: 785–787. [DOI] [PubMed] [Google Scholar]