Abstract
Although numerous studies have described the link between metabolic syndrome (MetS) and Coronary Artery Disease (CAD), no meta-analysis has been carried out on this relationship. Thus, the present study intended to address this limitation. A systematic search was carried out using electronic databases, such as PubMed, CINAHL Plus, Medline, and Web of Science. A sum of 10 studies (n = 9327) was incorporated in the meta-analysis. Compared with non-MetS, MetS was significantly associated with high CAD risk (OR = 4.03, 95% CI = 3.56–4.56). The MetS components were also significantly correlated with high CAD risk (OR = 3.72, 95% CI = 3.22–4.40). The presence of two (OR = 3.93, 95% CI = 2.81–5.49), three (OR = 4.09, 95% CI = 2.85–5.86), four (OR = 4.04, 95% CI = 2.83–5.78), or all five MetS components (OR = 3.92, 95% CI = 3.11–4.93), were significantly associated with a high risk of CAD. MetS and its individual or combined elements were linked with high CAD risk based on contemporary evidence. Thus, the assessment of MetS and its components might help identify people at a higher risk of advancing CAD in the future.
Keywords: metabolic syndrome, coronary artery disease, MetS, cardiovascular disease (CVD), CAD
1. Introduction
The World Health Organization (WHO), the European Group for the study of insulin resistance, the 2005 National Cholesterol Education Program (NCEP)-Adult Treatment Panel III (ATP-III), and the 2006 International Diabetes Federation formulated the definition of Metabolic Syndrome (MetS) after great debate [1,2]. MetS is a principal public health burden worldwide, and involves five cardiovascular hazard circumstances: obesity or high waist circumference (WC), high blood pressure (BP), hyperglycemia, hypertriglyceridemia, and low high-density lipoprotein cholesterol (HDL-c) levels [3,4]. MetS and its five individual components affect the blood vessels. As a result it is associated with extending the risk of cardiovascular disease by two-fold (CVD), type 2 diabetes mellitus (T2DM ) by five-fold [5], and all-cause mortality by 1.5 fold [6,7], along with elevating some specific cancer risks [8,9]. In recent years, the ubiquity and frequency of MetS have quickly progressed globally [10].
The enhanced pervasiveness and degree of MetS and its elements are causing harmful effects on coronary circulation [11]. However, the primary pathways connecting MetS and coronary artery disease (CAD) remain complex [12]. The connection between MetS and CVD in diverse communities is indicated [13,14,15]. However, no meta-analysis has been accompanied to examine the relationship between MetS and CAD risk. There is an urgent need to investigate this relationship by taking public health into account due to the high rate of MetS globally and the impact of CAD on coronary arteries the heart muscles.
While differently accepted definitions have been used in the published observational studies, the current meta-analysis of these studies tested the association of MetS and its segments with CAD risk. The primary hypothesis is that MetS would associate significantly with CAD risk. Furthermore, MetS components both individually and in combination would significantly associate with CAD risk.
2. Materials and Methods
The current meta-analysis was conducted based on a recommendation by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group [16]. Literature exploration, selection criteria, data extraction, and statistical analysis were carried out based on the Cochrane Collaboration guidelines [17].
2.1. Search Strategy
As advised by MOOSE [16], the search was carried using electronic databases, such as PubMed, CINAHL Plus, Medline, and Web of Science. These keywords or MeSH terms were utilized for the database search: MetS, CAD. The search was carried out for observational studies published till 25 September 2020. The search was also restricted to studies including adults aged 19 years or above and published as full-text in English.
2.2. Inclusion and Exclusion Criteria
The studies involved met the following inclusion criteria. The observational studies used for this work included MetS and its components as exposure and CAD as an outcome in adults aged 19 years and more. MetS components were as follows: (1) obesity or high WC, (2) advanced BP, (3) low HDL-c, (4) raised triglycerides (TG), and (5) raised hyperglycemia. MetS and its composition has been defined elsewhere [18].
Patients who have not experienced a recent acute incident of a known cardiovascular disease are defined as CAD [19]. CAD is also defined as restricted bloodstream to the heart muscle upon the build-up of fats, cholesterol, and plaque (atherosclerosis) in the heart’s arteries [20]. Clinically, CAD is determined as the presence of any coronary artery calcium score > 100, >75th percentile for one’s age and sex, or > 400 [21]. The development of CAD is determined according to the coronary artery stenosis as follows: (1) normal (no plaque and no stenosis to a plaque with < 25% stenosis); (2) mild (25%–49% stenosis); (3) moderate (50%–69% stenosis); (4) severe (70%–99% stenosis); and (5) occluded (100% stenosis) [22,23]. Table 1 presents the different accepted definitions of MetS and CAD in the studies incorporated in the meta-analysis.
Table 1.
MetS and CAD definitions as per the studies incorporated in this meta-analysis.
| Study | MetS | CAD |
|---|---|---|
| Iribarren et al. [24] | The 2001 NCEP-ATP-III definition (1) (WC ≥102 cm in men or ≥88 cm in women, fasting TG ≥150 mg/dL, HDL-c <40 mg/dl in men or <50 mg/dL in women, BP ≥130/85 mm Hg or use of BP medication, and FBG ≥110 mg/dL). The revised American Heart Association/National Heart, Lung, and Blood Institute definition incorporating the lower threshold for impaired fasting glucose (≥100 mg/dL) and FBG ≥126 mg/dL |
The ninth revision of the International Classification of Disease codes 410.x, 411.x, 413.x, or 414.x plus troponin. I > 4ng/dL, combination of creatine kinase fraction% >3.3, symptoms plus an electrocardiogram, and evidence of angiography during hospitalization. |
| Gui et al. [25] | The presence of ≥3 of the following five criteria: (1) WC: ≥90 cm in men or ≥80 cm in women; (2) TGs: ≥1.7 mmol/L or on drug treatment for elevated TGs; (3) HDL-c: <1.03 mmol/L in men or <1.3 mmol/L in women or on drug treatment for HDL-c; (4) BP ≥130 mm Hg, ≥85 mm Hg, or on antihypertensive drug treatment; (5) FBG ≥5.6 mmol/L or on drug treatment for elevated glucose. | Fifty percent or more lumen diameter reduction in at least one major coronary artery. |
| Won et al. [26] | The presence of ≥3 of the following: (a) BP ≥130 mm Hg, ≥85 mm Hg diastolic, or on antihypertensive treatment; (b) HDL-c <40 mg/dL in men or <50 mg/dL in women; (c) TG ≥150 mg/dL; (d) BMI ≥25 kg/m2; and (e) FBG ≥100 mg/dL. | At least one of the symptoms, including typical angina, atypical angina, dyspnea, and excessive fatigue, but not an acute coronary syndrome, required emergent coronary intervention or surgery. |
| Kim et al. [27] | The presence of MetS was determined using the updated 2005 ATP-III of the NCEP criteria by considering WC ≥90 cm in men and ≥80 cm in women. Those who had ≥3 of the five components were classified as having MetS. | First elective coronary angiography for evaluation of chest pain. |
| Kim et al. [23] | The presence of ≥3 of the flowing five criteria: (1) WC ≥90 cm in men and ≥80 cm in women, (2) TG ≥150 mg/ dL (1.7 mmol/L); (3) HDL-c <40 mg/dL (1.0 mmol/L) in men and <50 mg/dL (1.3 mmol/L) in women; (4) BP ≥130/85 mm Hg or the use of antihypertensive medication; and (5) FBG ≥100 mg/dL (6.1 mmol/L) or the self-reported use of antidiabetic medication (insulin or oral agents). | CAD assessed by the degree of coronary artery stenosis, presence of plaques, and its characteristics. |
| Kim et al. [28] | The presence of ≥3 of the following: WC modified into a body mass index of more than 25 kg/m2. The BP >130/85 mm Hg or being already on antihypertensive medication. FBG ≥110 mg/dL or being already on oral hypoglycemic agents or insulin. HDL-c < 40 mg/dL in men and < 50 mg/dL in women. TG ≥150 mg/dL. | >50% luminal diameter stenosis of at least one major epicardial coronary artery. |
| Jacobs et al. [29] | According to the American Heart Association and the National Heart, Lung, and Blood Institute, it is defined. | Self-reported myocardial infarction, bypass surgery of the coronary arteries, balloon dilatation or stent placement, and/or the presence of signs of myocardial infarction (Minnesota codes 1–1 or 1–2) or ischemia (Minnesota codes 1–3, 4–1, 4–2, 4–3, 5–1, 5–2, 5–3 or 7–1) on a 12-lead electrocardiogram. |
| Anderson et al. [22] | A combination of ≥3 of the following features: FBG 110 mg/dL or more, TG 150 mg/dL or more, HDL-c <40 mg/dL in men or <50 mg/dL in women, BP 130/85 mm Hg or more and WC >40 inches in men or more than 35 inches in women. | The degree of maximal diameter stenosis of each of the three principal coronary arteries and their major branches was estimated to the nearest 10%. |
| Berenjy et al. [30] | WC >88 cm in women and >102 in men. TG ≥150 mg/dL or medication for treatment. HDL-c <50 mg/dL in men and <40 in women or medication for treatment. BP ≥ 130/85 mm Hg or medication for treatment. FBGF ≥ 100 mg/dL or medication for treatment. | >50% luminal diameter stenosis of at least one major epicardial coronary artery. |
| Vakil et al. [31] | As per the revised NCEP, the presence of ≥3 of the following: A WC >102 cm, BP ≥ 130/85 mm Hg or on treatment, FBG ≥ 100 mg/dL, HDL-c ≥ 40 mg/dL, TG ≥ 150 mg/dL. As per the International Diabetes Federation, the presence of a WC ≥ 94 cm and at least two following risk factors: BP ≥ 130/85 mm Hg or on treatment, FBG ≥ 100 mg/dL, HDL-c < 40 mg/dL, TG ≥ 150 mg/dL. |
The presence of reversible and/or irreversible perfusion defects on single-photon emission computed tomography or resting and/or stress-induced wall motion abnormalities on two-dimensional stress echocardiography. |
2.3. Data Extraction
Data were individually filtered by extracting potentially relevant studies based on the title and abstract. According to the eligibility criteria, the relevant studies were selected separately by reading the full-text. The final eligible studies were then chosen according to the inclusion and exclusion standards.
In this meta-analysis, we included prior studies that reported odds ratios (ORs) and 95% confidence interval (CI) for the association of MetS and its segments to CAD risk compared to non-MetS. The exclusion criteria, OR and CI participants with a diagnosis other than MetS and its components were not reported. Studies that did not explore the link between MetS, its components, and CAD risk were eliminated.
2.4. Statistical Analysis
The primary outcome was the OR of CAD in people with MetS compared to non-MetS subjects. The secondary outcome was the OR of CAD in individuals with any element of MetS. The territory outcome was the OR of CAD in individuals with two or more MetS segments. A satisfactory agreement was defined as adjusting at least two of six covariates, including age, sex, family records of CAD, body mass index (BMI), low-density cholesterol, and smoking status.
We scrutinized multivariate-adjusted outcome data, displayed as OR and 95% CI. The reversed variation method was applied for investigation after log-transformation of study-specific assessments. For example, 95% CI was converted into standard error (SE) employing the following equation: SE = upper CI - lower CI/3.92. The I2 statistic was applied to test heterogeneity. The heterogeneity between studies was interpreted as moderate (30%–59%), substantial (60%–89%), or considerable (90%–100%) [17]. Studies were combined, applying a fixed-effect model, if there was a relevant, later state of heterogeneity among studies. Otherwise, a random-effects model was used. The potential publication bias for primary and secondary outcomes was assessed utilizing funnel plots [32]. All analyses were completed using RevMan software version 5.4 for Windows (The Cochrane Collaboration, Copenhagen, Denmark) [33]. The p < 0.05 was described as of statistical importance.
3. Results
3.1. Selected Studies and Characteristics
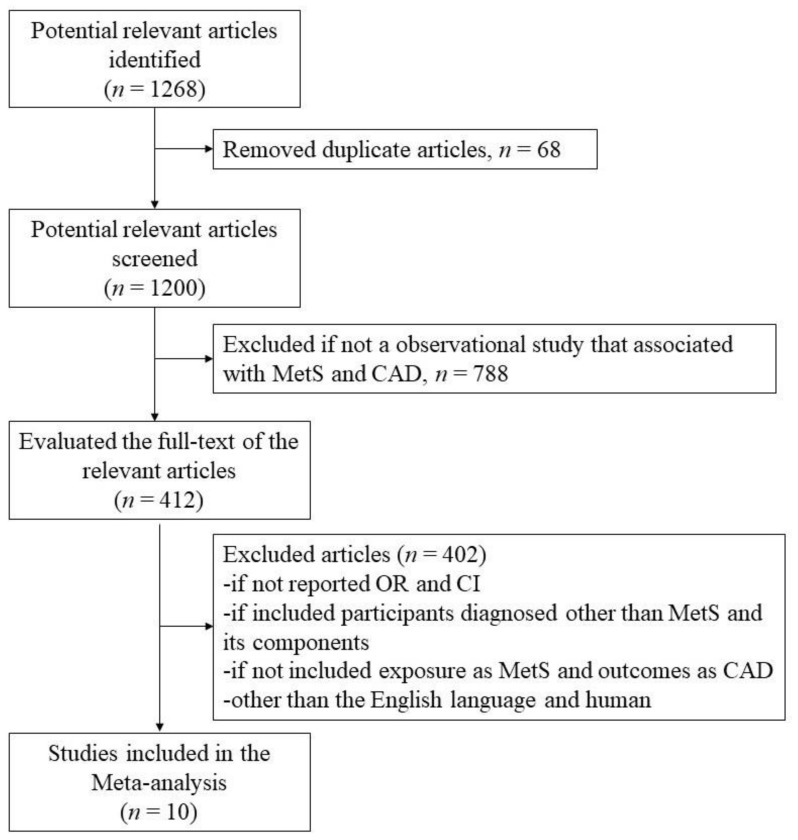
Out of 1268 studies identified in a database search, a total of 10 studies [22,23,24,25,26,27,28,29,30,31] were incorporated in the meta-analysis after eliminating those not falling within the eligibility criteria. Excluded articles and the reason for their exclusion are illustrated in Figure 1. The features of the incorporated studies are described in Table 2. A total of 9327 subjects participated in the ten included studies. Four studies were from South Korea [23,26,27,28], and three studies were from the United States of America (USA) [22,24,30]. Of 9327 subjects, 3969 had MetS and are referred to as cases, while 5358 had no MetS and are referred to as controls. Out of 3969 cases, 1948 were men, and 2021 were women. Men, n = 3048 and women, n = 2310 were controls. The average age of all participants was above 45 years.
Figure 1.
Flowchart of studies identified through a database search.
Table 2.
Descriptive characteristics of included studies.
| Author | Study Design |
Country | Sample Size | Age in Year Mean (Standard Deviation) |
Exposure | Risk Factors Adjusted | Outcome |
|---|---|---|---|---|---|---|---|
| Irribarren et al., [24] | Case-control | USA |
n = 393 (women = 239) cases n = 393 (women = 239) control |
Case: 45.8 (6.5) Control: 45.2 (5.6) |
Metabolic Syndrome (MetS) | Age, educational attainment, cigarette smoking, alcohol consumption, and body mass index | Early-onset Coronary Artery Disease (CAD) |
| Gui et al., [25] | Retrospective | China |
n = 296 (women = 91) without MetS n = 330 (women = 141) with MetS |
58 (9) without MetS 60 (9) with MetS |
MetS score, MetS, and its components | Age and sex | Angiographic CAD |
| Won et al., [26] | Cross-sectional | S. Korea |
n = 1515 (men = 749) without MetS n = 793 (men = 406) with MetS |
57 (9) with no MetS 57 (9) with MetS |
MetS and its components | Age, sex, current smoking, and low-density cholesterol | Severity of CAD |
| Kim et al., [27] | Cross-sectional | S. Korea |
n = 185 (male = 100) without MetS n = 178 (male = 96) with MetS |
61.8 (11.5) without MetS 62.2 (10.6) with MetS |
MetS score in the subject without diabetes included | Age and sex | Angiographic CAD along with high sensitivity C-reactive protein, interleukin-6, resistin, and adiponectin |
| Kim et al., [23] | Retrospective cohort | S. Korea |
n = 825 (male = 661) with MetS n = 1601 (male = 1278) without MetS |
56.6 (7.5) with MetS 56.2 (7.2) without MetS |
MetS | Age, sex, smoking status, family history of CAD, body mass index, and low-density cholesterol | Progression of CAD |
| Kim et al., [28] | Retrospective | S. Korea |
n = 349 (male = 223) without MetS n = 283 (male = 171) with MetS |
61 (10.8) without MetS 61 (10.4) with MetS |
MetS and its components | MetS components | Angiographic CAD |
| Jacobs et al., [29] | Cohort | The Netherlands |
n = 225 (male = 149) without MetS n = 305 (male = 194) with MetS |
58.8 (7.4) without MetS 60.2 (6.6) with MetS |
MetS | Age, sex, and smoking | CAD |
| Anderson et al., [22] | Retrospective | USA |
n = 69 male without MetS n = 69 male with MetS |
63 (13) without MetS 63 (12) with MetS |
MetS and its components | Age, sex, smoking status, family history of CAD, body mass index, and low-density cholesterol | Angiographic CAD |
| Berenjy et al., [30] | Case-control | Malaysia |
n = 258 cases with MetS n = 190 control without MetS |
- | MetS components | - | CAD |
| Vakil et al., [31] | Retrospective | USA | n = 1071 male with or without silent CAD | 61 (11) | MetS and its component, such as waist circumference | - | Silent CAD |
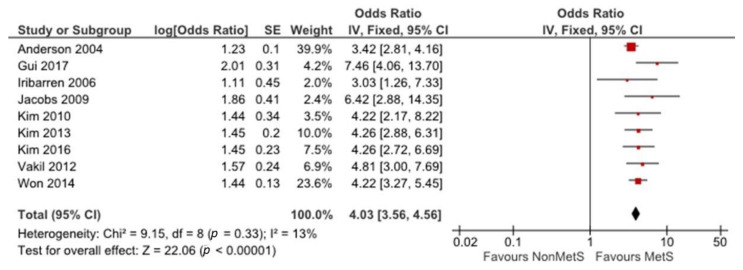
3.2. Association between MetS and CAD
Figure 2 shows the link between MetS and CAD. Nine studies [22,23,24,25,26,27,28,30,31], with 8879 participants reported CAD ORs with MetS groups compared with non-MetS groups. The fixed-effect pattern was applied to analyze the correlation between MetS and CAD. There was no notable heterogeneity between all studies (I2 = 13%, p = 0.33). MetS was significantly associated with high CAD risk (OR = 4.03, 95% CI = 3.56–4.56).
Figure 2.
The association between MetS and CAD risk. The red symbols indicate individual studies’ odds ratios and black line shows 95% CI. The horizontal points of the diamond show the studies average limits of the 95% CI.
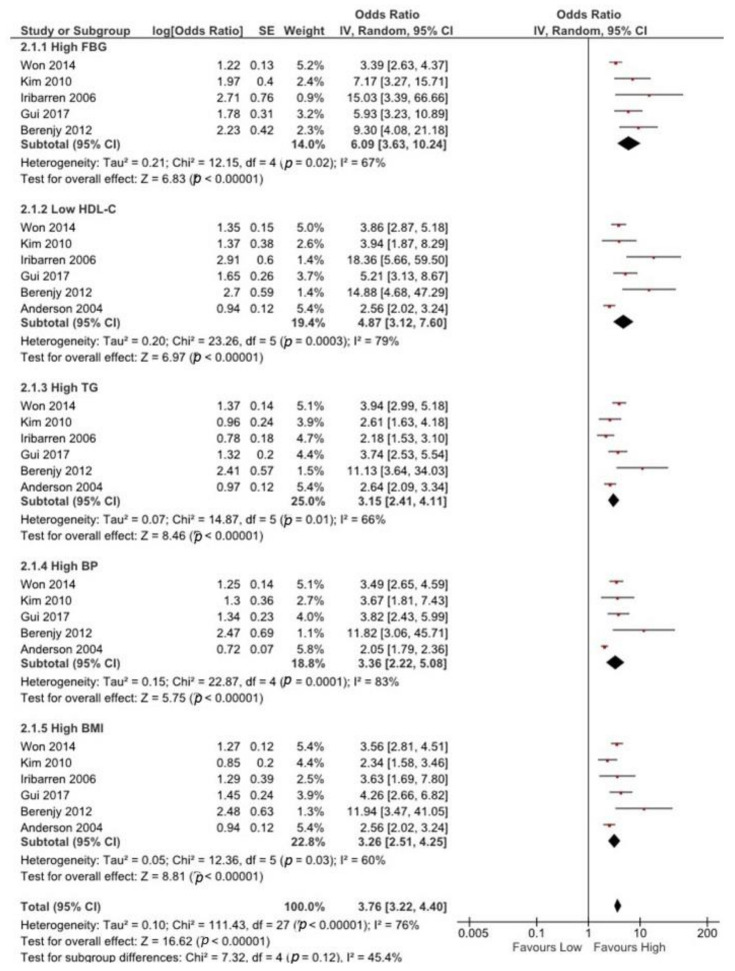
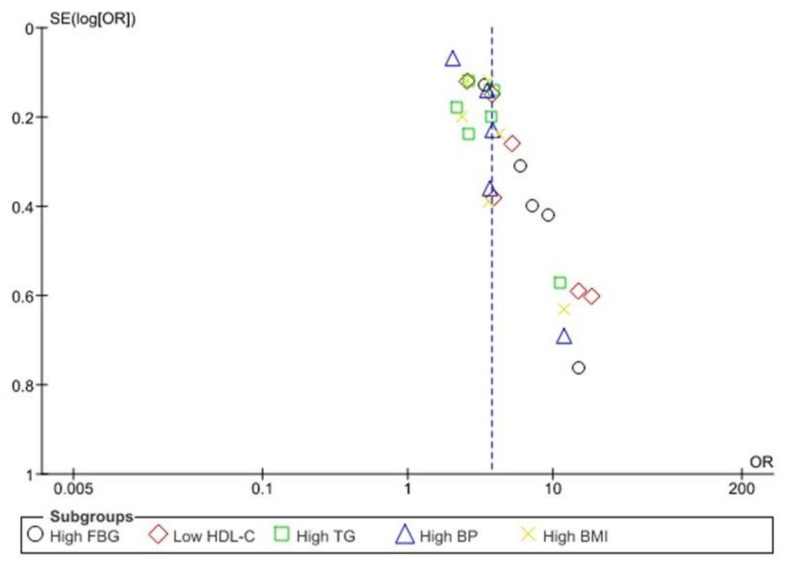
3.3. Association between Any MetS Component and CAD
Figure 3 exhibits the association between different MetS components and CAD risk. Five studies [24,25,26,28,30] with 4527 participants reported CAD ORs with high fasting blood glucose (FBG) groups compared to low FBG groups. The random-effect design was employed to analyze the connection between high FBG and CAD risk due to substantial heterogeneity between studies (I2 = 67%, p = 0.02).
Figure 3.
The association between any MetS component and CAD risk. The red symbols indicate individual studies’ odds ratios and black line shows 95% CI. The horizontal points of the diamond show the studies average limits of the 95% CI.
Six studies [22,24,25,26,28,30] with 4389 participants reported ORs of CAD with low HDL-c, high TG, and high BMI groups compared with high HDL-c, low TG, and low BMI groups. Significant heterogeneity was found in low HDL-C (I2 = 79%, p = 0.003), high TG (I2 = 66%, p = 0.01), and high BMI (I2 = 60%, p = 0.03) groups, within the six studies.
Five studies [22,25,26,28,30] with 3603 participants reported ORs of CAD with a high BP group compared with the low BP group. Notable heterogeneity was found between all five studies (I2 = 83%, p = 0.01). Significant heterogeneity was found among all studies that reported ORs of CAD with any component of MetS (I2 = 76%, p = 0.01). Thus, any MetS component was correlated significantly with high CAD risk (OR = 3.72, 95% CI = 3.22–4.40).
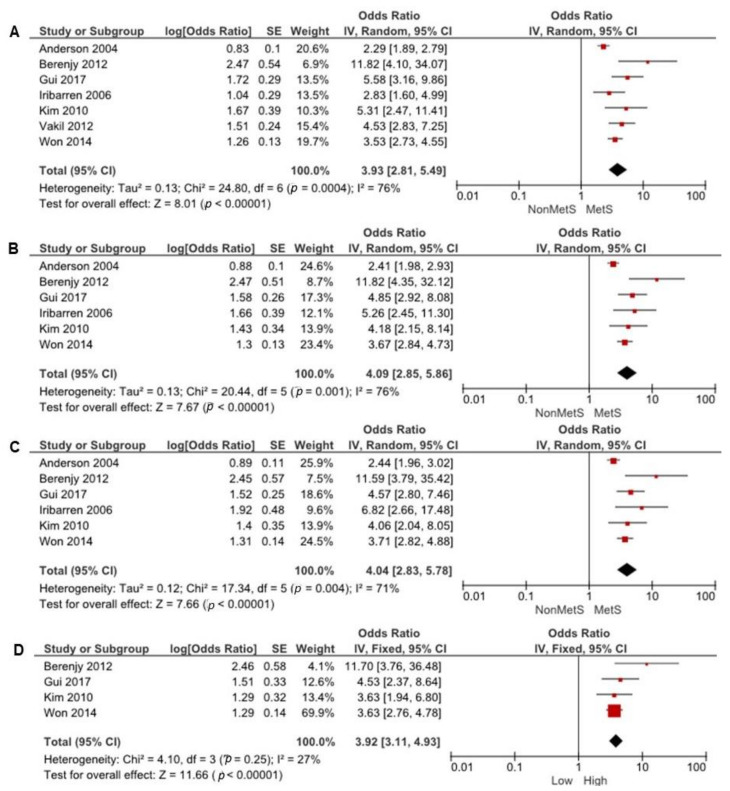
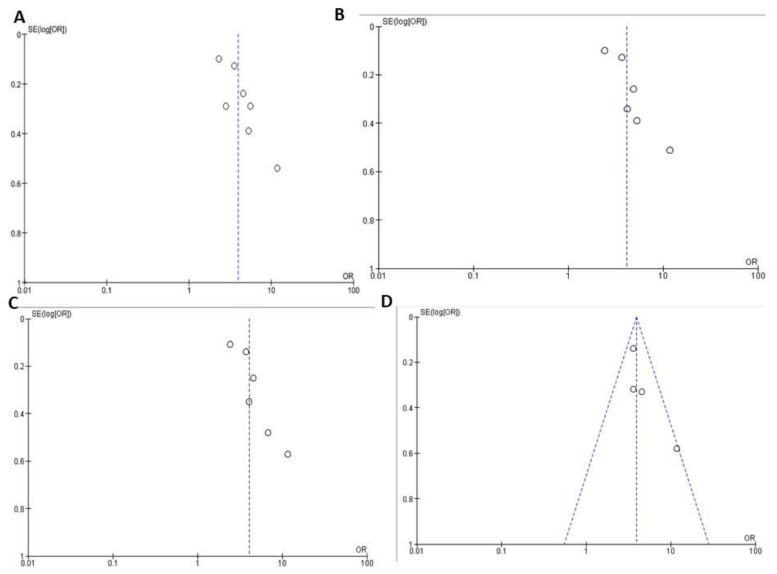
3.4. Association between Multiple MetS Components and CAD
Figure 4 represents the association between two or more MetS elements and CAD risk. Seven studies [22,24,25,26,28,30,31] with 5598 participants reported CAD ORs with two MetS component groups compared to non-MetS groups. There was important heterogeneity between all seven studies (I2 = 76%, p = 0.004). Thus, two MetS components’ presence was significantly associated with high CAD risk (OR = 3.93, 95% CI = 2.81–5.49).
Figure 4.
The association of (A) two, (B) three, (C) four, and (D) all five MetS elements with CAD risk. The red symbols indicate individual studies’ odds ratios and black line shows 95% CI. The horizontal points of the diamond show the studies average limits of the 95% CI.
Six studies [22,24,25,26,28,30] with 4389 participants reported CAD ORs with three MetS components compared with non-MetS component. Significant heterogeneity was found between all six studies (I2 = 75%, p = 0.001). The presence of three MetS components was significantly associated with high CAD risk (OR = 4.09, 95% CI = 2.85–5.86). Six studies [22,24,25,26,28,30] with 4389 participants reported CAD ORs with four MetS components compared with non-MetS component. Significant heterogeneity was found between all six studies (I2 = 71%, p = 0.04). The presence of four MetS components was significantly associated with high CAD risk (OR = 4.04, 95% CI = 2.83–5.78).
Four studies [25,26,28,30] with 3741 participants reported CAD ORs with all five MetS components compared with non-MetS components. The fixed-model was adopted for the analysis due to no significant heterogeneity between all four studies (I2 = 27%, p = 0.25). The presence of all five MetS components was significantly associated with high CAD risk (OR = 3.92, 95% CI = 3.11–4.93).
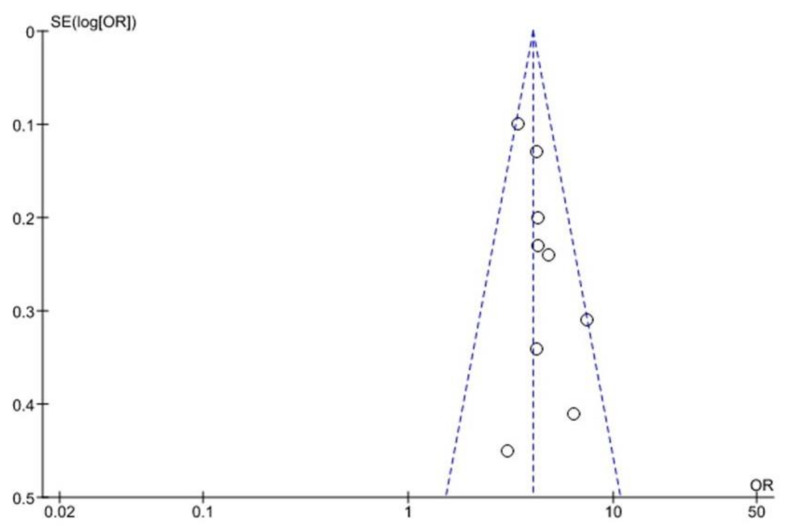
3.5. Funnel Plot Analysis
There is no bias between the studies in the funnel plot associated with MetS, any of the five MetS, and CAD (Figure 5). The association of two, three or four MetS components and CAD reveals an asymmetric scatter plot (Figure 6 and Figure 7A–C). Figure 7D illustrate the association between all five MetS elements and CAD.
Figure 5.
Association between MetS and CAD outcome. The dashed lines indicate the funnel and open circles represents effect from individual studies.
Figure 6.
Association between MetS individual components and CAD outcome.
Figure 7.
Association between the presence of (A) 2, (B) 3, (C) 4 and (D) all 5 MetS components and CAD outcome. The dashed lines indicate the funnel and open circles represents effect from individual studies.
4. Discussion
The current meta-analysis examined the association of MetS and its five elements with CAD risk among adult populations. The findings revealed that MetS correlated significantly with high CAD risk compared to non-MetS. Furthermore, any individual MetS element was significantly linked with high CAD risk. The attendance of two or more MetS components was also connected with high CAD risk compared to the absence of any component. The presence of from two to four MetS components significantly increased the correlation in the severity of CAD. To our understanding, this is the first meta-analysis that presented evidence on the association of MetS and its elements with CAD risk.
A longitudinal study concentrated on the consequences of MetS on BP control and its function in stimulation of arterial aging in hypertensive treated people [34]. The results revealed that the presence of MetS presents a worse BP control than non-MetS and is correlated with accelerated aortic stiffening. These findings may be partially linked to change in BP. However, this finding must be interpreted with caution due to the lack of BP measures other than supine BP when the pulse wave velocity evaluation is 24 h-Ambulatory BP.
MetS is likely to result in the non-alcoholic fatty liver condition, T2DM, and vascular conditions such as stroke, peripheral vascular disease, and CVD [35]. Initial meta-analysis showed some limited evidence that MetS is a significant risk factor for CVD [36,37]. Another meta-analysis showed that MetS might be a significant hazard factor for stroke [38]. However, to date, no meta-analysis was carried out to evaluate the association of MetS and its elements with CAD risk. Therefore, the current meta-analysis was conducted with every published study to date.
There were no randomized control trials (RCTs) observed during the literature search on this subject. The majority of the published retrospective studies fitted the inclusion standards added to this meta-analysis [22,25,28,31]. There were only two published case-control studies [24,30] that were included. A careful review of all the incorporated studies was conducted for any potential bias.
The relation between MetS and CAD risk has been noted in individual studies among various populations aged 50 years or above. These studies vary considerably in their methodology and MetS definition. Various stratified analyses were conducted to examine possible heterogeneity causes, and the outcomes helped our overall conclusions. The sign of a relationship between MetS and CAD risk appeared with no significant heterogeneity between the studies.
Our findings are comparable with preliminary proof regarding MetS elements. Waist circumference [39], elevated BP [40,41], low HDL-c levels [42,43,44], elevated triglycerides [45,46], and high hyperglycemia [47,48] are individually associated with CAD risk. A study also exhibited a significant connection between one component of MetS and CAD risk development compared two components of MetS in older people [49]. However, all these studies differ from our investigation concerning gender participation and age. A study finding demonstrates that MetS and high BP are linked with enhanced carotid atherosclerosis more than MetS without high BP. The determination of MetS per se might not sufficiently identify subjects at raised cardiovascular risk [50]. Therefore, it might be essential to examine the relationship between MetS elements and CAD risk.
In the meta-analysis, as mentioned earlier, the association of two or more MetS components with CAD risk was similar to an earlier study [51]. That confirmed the association of low levels of HDL-c and high levels of TG to CAD risk. Another study indicated that abdominal obesity and related atherogenic dyslipidemia modulate CAD risk related to hyperglycemia [52]. However, previous study results revealed a significant rise in MetS elements, such as low-HDL-c, high-FBG, and WC, in patients with CAD [37]. This study concluded that hyperglycemia, dyslipidemia, and obesity are indispensable predictors of MetS in patients with CAD.
This meta-analysis’ major strength included studies that defined MetS well, along with its elements (such as WC, BP, HDL-c, TG, and hyperglycemia), and CAD. Another strength of this investigation is the large sample size of 9327 participants from 10 incorporated studies. However, some limitations have been acknowledged when understanding the results of this meta-analysis. First, there were no prospective studies on this topic. This kind of evidence may give more precise evaluations than retrospective studies, because they usually have more reliable controls for possible confounders, including socioeconomic, lifestyle, and health factors related to MetS progress. They also have adequate continuance of follow-up to identify MetS cases.
Moreover, these studies collect susceptibility information before the appearance of diseases. Therefore, the temporal causal relationship can be examined. Secondly, subgroup analyses, such as sex (men versus women) and follow-up duration, were not performed due to the lack of data concerning sex and variation in the study design. Thirdly, inter-study variations in MetS definition and patients’ demographics might also influence the results. Fourthly, the studies that did not show output in OR and 95% CI were excluded. This might decrease the validity of this study. Overall, this is an observational meta-analysis study showing the association, but not the interconnection significance.
The current findings are significant for public health since the ubiquity and frequency of MetS have rapidly increased globally [10]. A possible reason for the increase of MetS incidence might be the western lifestyle, marked by extensive consumption of red and treated meat [53], processed grains and deep-fried foods [54], and sugar-sweetened drinks, such as soft drinks, fruit drinks, iced tea, and energy and vitamin water drinks [55]. Another possible reason might be that many people worldwide do not meet their dairy requirements, especially in the developing countries [56,57], and lack physical activity [54]. The results from this meta-analysis with recent evidence on T2DM [5], all-cause mortality [6,7], and specific cancer risks [8,9] provide further support for public health advice on increasing the consumption of dairy products [58], fruits/vegetables [59], and increasing physical activity [54], limiting the risk of MetS, its components, and CVD, especially CAD, in the global population.
The relationship between MetS, all five components of MetS, and CAD indicates a symmetrical scatter pattern with no publication bias. A potential reaction could be a fixed-effect analysis that assumes little or low heterogeneity and a single underlying effect across studies [32]. Asymmetrical scatter plots of the association between two, three or four MetS components and CAD indicate a publication bias between the studies. this may be due to the studies’ quality, the different intensity of the intervention, and the underlying risk [32]. In addition, random-effect analysis allows for variability and average treatment effect across studies. Although the Funnel plots’ purpose is to detect publication bias, the components of MetS relating to CAD risk, demonstrating an asymmetry of high FBG and low HDL-c, suggests that these components might pose higher CAD risk than high TG and high BP.
5. Conclusions
In conclusion, the present meta-analysis intended to examine the association of MetS and its five elements with CAD risk. This meta-analysis shows that MetS and its elements are significantly associated with high CAD risk. The initial evaluation of MetS and its five components might help identify individuals at higher risk of CAD. The current findings suggest that MetS and its components can be tested to validate CAD risk. Future study is required for establishing high-quality evidence by including RCTs or prospective cohort studies in the identification of the link between MetS and CAD risk among the global population.
Author Contributions
Conceptualization, A.F.A.; K.K.A.; V.V. and I.A.K.; methodology, A.F.A.; K.K.A.; V.V. and I.A.K.; software, A.F.A.; N.J.A. and V.V.; validation, A.F.A.; K.K.A.; V.V. and I.A.K.; formal analysis, A.F.A.; K.K.A. and V.V.; investigation, A.F.A.; K.K.A. and V.V.; resources, A.F.A.; and K.K.A.; data curation, A.F.A.; N.J.A.; V.V. and I.A.K.; writing—original draft preparation, V.V. and I.A.K.; writing—review and editing, A.F.A.; K.K.A.; V.V. and I.A.K.; visualization, A.F.A.; K.K.A.; V.V. and I.A.K.; supervision, A.F.A. and K.K.A.; project administration, A.F.A.; N.J.A. and K.K.A.; funding acquisition, A.F.A. and K.K.A. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to continue their honest gratitude to Scientific Research’s Deanship at King Saud University for funding this research through the Research Group Project No. RGP-244.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Saklayen M.G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 2018;20:12. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ansarimoghaddam A., Adineh H.A., Zareban I., Iranpour S., HosseinZadeh A., Kh F. Prevalence of metabolic syndrome in Middle-East countries: Meta-analysis of cross-sectional studies. Diabetes Metab. Syndr. Clin. Res. Rev. 2018;12:195–201. doi: 10.1016/j.dsx.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Alberti K., Eckel R.H., Grundy S.M., Zimmet P.Z., Cleeman J.I., Donato K.A., Fruchart J.-C., James W.P.T., Loria C.M., Smith S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 4.Eckel R.H., Grundy S.M., Zimmet P.Z. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 5.Saely C., Rein P., Drexel H. The metabolic syndrome and risk of cardiovascular disease and diabetes: Experiences with the new diagnostic criteria from the International Diabetes Federation. Horm. Metab. Res. 2007;39:642–650. doi: 10.1055/s-2007-985822. [DOI] [PubMed] [Google Scholar]
- 6.Hirode G., Wong R.J. Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. Jama. 2020;323:2526–2528. doi: 10.1001/jama.2020.4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tørris C., Bjørnnes A.K. Duration of Lactation and Maternal Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients. 2020;12:2718. doi: 10.3390/nu12092718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao P., Xia N., Zhang H., Deng T. The Metabolic Syndrome Is a Risk Factor for Breast Cancer: A Systematic Review and Meta-Analysis. Obes. Facts. 2020;13:384–396. doi: 10.1159/000507554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mariani M., Sassano M., Boccia S. Metabolic syndrome and gastric cancer risk: A systematic review and meta-analysis. Eur. J. Cancer Prev. 2020 doi: 10.1097/CEJ.0000000000000618. [DOI] [PubMed] [Google Scholar]
- 10.Cameron A.J., Shaw J.E., Zimmet P.Z. The metabolic syndrome: Prevalence in worldwide populations. Endocrinol. Metab. Clin. 2004;33:351–375. doi: 10.1016/j.ecl.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Rocha E. Metabolic syndrome and cardiovascular risk. Rev. Port. De Cardiol. 2019;38:333–335. doi: 10.1016/j.repc.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Climent B., Santiago E., Sánchez A., Muñoz-Picos M., Pérez–Vizcaíno F., García-Sacristán A., Rivera L., Prieto D. Metabolic syndrome inhibits store-operated Ca2+ entry and calcium-induced calcium-release mechanism in coronary artery smooth muscle. Biochem. Pharmacol. 2020:114222. doi: 10.1016/j.bcp.2020.114222. [DOI] [PubMed] [Google Scholar]
- 13.Montazerifar F., Bolouri A., Mozaffar M.M., Karajibani M. The prevalence of metabolic syndrome in coronary artery disease patients. Cardiol. Res. 2016;7:202. doi: 10.14740/cr507w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahalle N., Garg M., Naik S.S., Kulkarni M.V. Association of metabolic syndrome with severity of coronary artery disease. Indian J. Endocrinol. Metab. 2014;18:708. doi: 10.4103/2230-8210.139238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neeb Z.P., Edwards J.M., Alloosh M., Long X., Mokelke E.A., Sturek M. Metabolic syndrome and coronary artery disease in Ossabaw compared with Yucatan swine. Comp. Med. 2010;60:300–315. [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Jama. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 17.Higgins J., Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1. The Cochrane Collaboration. [(accessed on 20 August 2020)];2011 Available online: https://handbook-5-1.cochrane.org/
- 18.Tillin T., Forouhi N., Johnston D., McKeigue P., Chaturvedi N., Godsland I. Metabolic syndrome and coronary heart disease in South Asians, African-Caribbeans and white Europeans: A UK population-based cross-sectional study. Diabetologia. 2005;48:649–656. doi: 10.1007/s00125-005-1689-3. [DOI] [PubMed] [Google Scholar]
- 19.Fox K.A., Metra M., Morais J., Atar D. The myth of ‘stable’coronary artery disease. Nat. Rev. Cardiol. 2020;17:9–21. doi: 10.1038/s41569-019-0233-y. [DOI] [PubMed] [Google Scholar]
- 20.Mendis S., Puska P., Norrving B. In: World Atlas on Cardiovascular Disease Prevention and Control. Mendis S., Puska P., Norrving B., editors. World Health Organization; Geneva, Switzerland: 2013. pp. 1–163. [Google Scholar]
- 21.Members W.G., Lloyd-Jones D., Adams R.J., Brown T.M., Carnethon M., Dai S., De Simone G., Ferguson T.B., Ford E., Furie K. 22. Glossary. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 22.Anderson J.L., Horne B.D., Jones H.U., Reyna S.P., Carlquist J.F., Bair T.L., Pearson R.R., Lappé D.L., Muhlestein J.B. Which features of the metabolic syndrome predict the prevalence and clinical outcomes of angiographic coronary artery disease? Cardiology. 2004;101:185–193. doi: 10.1159/000076695. [DOI] [PubMed] [Google Scholar]
- 23.Kim L.K., Yoon J.W., Lee D.-H., Kim K.M., Choi S.H., Park K.S., Jang H.C., Kim M.-K., Park H.E., Choi S.-Y. Impact of metabolic syndrome on the progression of coronary calcium and of coronary artery disease assessed by repeated cardiac computed tomography scans. Cardiovasc. Diabetol. 2016;15:92. doi: 10.1186/s12933-016-0404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iribarren C., Go A.S., Husson G., Sidney S., Fair J.M., Quertermous T., Hlatky M.A., Fortmann S.P. Metabolic syndrome and early-onset coronary artery disease: Is the whole greater than its parts? J. Am. Coll. Cardiol. 2006;48:1800–1807. doi: 10.1016/j.jacc.2006.03.070. [DOI] [PubMed] [Google Scholar]
- 25.Gui M.-H., Ling Y., Liu L., Jiang J.-J., Li X.-Y., Gao X. Effect of metabolic syndrome score, metabolic syndrome, and its individual components on the prevalence and severity of angiographic coronary artery disease. Chin. Med J. 2017;130:669. doi: 10.4103/0366-6999.201611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Won K.-B., Chang H.-J., Sung J., Shin S., Cho I.-J., Shim C.-Y., Hong G.-R., Kim Y.J., Choi B.-W., Chung N. Differential association between metabolic syndrome and coronary artery disease evaluated with cardiac computed tomography according to the presence of diabetes in a symptomatic Korean population. BMC Cardiovasc. Disord. 2014;14:105. doi: 10.1186/1471-2261-14-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim J.-Y., Choi E.-Y., Mun H.-S., Min P.-K., Yoon Y.-W., Lee B.K., Hong B.-K., Rim S.-J., Kwon H.M. Usefulness of metabolic syndrome score in the prediction of angiographic coronary artery disease severity according to the presence of diabetes mellitus: Relation with inflammatory markers and adipokines. Cardiovasc. Diabetol. 2013;12:140. doi: 10.1186/1475-2840-12-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim J.-Y., Mun H.-S., Lee B.K., Yoon S.B., Choi E.-Y., Min P.-K., Yoon Y.-W., Hong B.-K., Rim S.-J., Kwon H.M. Impact of metabolic syndrome and its individual components on the presence and severity of angiographic coronary artery disease. Yonsei Med. J. 2010;51:676–682. doi: 10.3349/ymj.2010.51.5.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobs M., Van Greevenbroek M., Van Der Kallen C., Ferreira I., Blaak E., Feskens E., Jansen E., Schalkwijk C., Stehouwer C. Low-grade inflammation can partly explain the association between the metabolic syndrome and either coronary artery disease or severity of peripheral arterial disease: The CODAM study. Eur. J. Clin. Investig. 2009;39:437–444. doi: 10.1111/j.1365-2362.2009.02129.x. [DOI] [PubMed] [Google Scholar]
- 30.Berenjy S., Rahmat A.B., Yassin Z.B., Sann L.M., Sahebjamee F., Hanachi P. Metabolic syndrome and risk of Coronary Artery Disease in west of Iran. Life Sci. J. 2012;9:706–717. [Google Scholar]
- 31.Vakil K.P., Malhotra S., Sawada S., Campbell S.R., Sayfo S., Kamalesh M. Waist circumference and metabolic syndrome: The risk for silent coronary artery disease in males. Metab. Syndr. Relat. Disord. 2012;10:225–231. doi: 10.1089/met.2011.0099. [DOI] [PubMed] [Google Scholar]
- 32.Sterne J.A., Harbord R.M. Funnel plots in meta-analysis. Stata J. 2004;4:127–141. doi: 10.1177/1536867X0400400204. [DOI] [Google Scholar]
- 33.Alderson P., Green S., Higgins J.P.T. Cochrane Reviewers’ Handbook 4.2.2 [updated March 2004] [(accessed on 20 August 2020)]; Available online: http://www.cochrane.org/resources/handbook/hbook.htm.
- 34.Maloberti A., Bruno R., Facchetti R., Grassi G., Taddei S., Ghiadoni L., Giannattasio C. THE role of metabolic syndrome in blood pressure control and pulse wave velocity progression over a 3.5 years in treated hypertensive PATIENTS. Eur. J. Intern. Med. 2020;76:107–109. doi: 10.1016/j.ejim.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 35.McNamara A. Metabolic syndrome. InnovAiT. 2019;12:582–588. doi: 10.1177/1755738019864615. [DOI] [Google Scholar]
- 36.Galassi A., Reynolds K., He J. Metabolic syndrome and risk of cardiovascular disease: A meta-analysis. Am. J. Med. 2006;119:812–819. doi: 10.1016/j.amjmed.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 37.Mottillo S., Filion K.B., Genest J., Joseph L., Pilote L., Poirier P., Rinfret S., Schiffrin E.L., Eisenberg M.J. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010;56:1113–1132. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 38.Li X., Li X., Lin H., Fu X., Lin W., Li M., Zeng X., Gao Q. Metabolic syndrome and stroke: A meta-analysis of prospective cohort studies. J. Clin. Neurosci. 2017;40:34–38. doi: 10.1016/j.jocn.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 39.Dimitriadis K., Tsioufis C., Mazaraki A., Liatakis I., Koutra E., Kordalis A., Kasiakogias A., Flessas D., Tentolouris N., Tousoulis D. Waist circumference compared with other obesity parameters as determinants of coronary artery disease in essential hypertension: A 6-year follow-up study. Hypertens. Res. 2016;39:475–479. doi: 10.1038/hr.2016.8. [DOI] [PubMed] [Google Scholar]
- 40.Denardo S.J., Gong Y., Nichols W.W., Messerli F.H., Bavry A.A., Cooper-DeHoff R.M., Handberg E.M., Champion A., Pepine C.J. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: An INVEST substudy. Am. J. Med. 2010;123:719–726. doi: 10.1016/j.amjmed.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lieb W., Jansen H., Loley C., Pencina M.J., Nelson C.P., Newton-Cheh C., Kathiresan S., Reilly M.P., Assimes T.L., Boerwinkle E. Genetic predisposition to higher blood pressure increases coronary artery disease risk. Hypertension. 2013;61:995–1001. doi: 10.1161/HYPERTENSIONAHA.111.00275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cordero A., Moreno-Arribas J., Bertomeu-González V., Agudo P., Miralles B., Masiá M.D., López-Palop R., Bertomeu-Martínez V. Low levels of high-density lipoproteins cholesterol are independently associated with acute coronary heart disease in patients hospitalized for chest pain. Rev. Española De Cardiol. (Engl. Ed. ) 2012;65:319–325. doi: 10.1016/j.recesp.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 43.Gotto A.M., Jr. Low high-density lipoprotein cholesterol as a risk factor in coronary heart disease: A working group report. Circulation. 2001;103:2213–2218. doi: 10.1161/01.CIR.103.17.2213. [DOI] [PubMed] [Google Scholar]
- 44.Weverling-Rijnsburger A.W., Jonkers I.J., Van Exel E., Gussekloo J., Westendorp R.G. High-density vs low-density lipoprotein cholesterol as the risk factor for coronary artery disease and stroke in old age. Arch. Intern. Med. 2003;163:1549–1554. doi: 10.1001/archinte.163.13.1549. [DOI] [PubMed] [Google Scholar]
- 45.Harchaoui K., Visser M., Kastelein J., Stroes E., Dallinga-Thie G. Triglycerides and cardiovascular risk. Curr. Cardiol. Rev. 2009;5:216–222. doi: 10.2174/157340309788970315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarwar N., Danesh J., Eiriksdottir G., Sigurdsson G., Wareham N., Bingham S. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2006;115:450–458. doi: 10.1161/CIRCULATIONAHA.106.637793. [DOI] [PubMed] [Google Scholar]
- 47.Ding D., Qiu J., Li X., Li D., Xia M., Li Z., Su D., Wang Y., Zhang Y., Zhang J. Hyperglycemia and mortality among patients with coronary artery disease. Diabetes Care. 2014;37:546–554. doi: 10.2337/dc13-1387. [DOI] [PubMed] [Google Scholar]
- 48.Nielson C., Lange T., Hadjokas N. Blood glucose and coronary artery disease in nondiabetic patients. Diabetes Care. 2006;29:998–1001. doi: 10.2337/dc05-1902. [DOI] [PubMed] [Google Scholar]
- 49.Ahmadi A., Leipsic J., Feuchtner G., Gransar H., Kalra D., Heo R., Achenbach S., Andreini D., Al-Mallah M., Berman D.S. Is metabolic syndrome predictive of prevalence, extent, and risk of coronary artery disease beyond its components? Results from the multinational coronary CT angiography evaluation for clinical outcome: An international multicenter registry (CONFIRM) PLoS ONE. 2015;10:e0118998. doi: 10.1371/journal.pone.0118998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irace C., Cortese C., Fiaschi E., Carallo C., Sesti G., Farinaro E., Gnasso A. Components of the metabolic syndrome and carotid atherosclerosis: Role of elevated blood pressure. Hypertension. 2005;45:597–601. doi: 10.1161/01.HYP.0000158945.52283.c2. [DOI] [PubMed] [Google Scholar]
- 51.Wilson P.W. High-density lipoprotein, low-density lipoprotein and coronary artery disease. Am. J. Cardiol. 1990;66:A7–A10. doi: 10.1016/0002-9149(90)90562-F. [DOI] [PubMed] [Google Scholar]
- 52.St-Pierre J., Lemieux I., Vohl M.-C., Perron P., érald Tremblay G., Després J.-P., Gaudet D. Contribution of abdominal obesity and hypertriglyceridemia to impaired fasting glucose and coronary artery disease. Am. J. Cardiol. 2002;90:15–18. doi: 10.1016/S0002-9149(02)02378-0. [DOI] [PubMed] [Google Scholar]
- 53.Kim Y., Je Y. Meat consumption and risk of metabolic syndrome: Results from the Korean population and a meta-analysis of observational studies. Nutrients. 2018;10:390. doi: 10.3390/nu10040390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dunkley A., Charles K., Gray L., Camosso-Stefinovic J., Davies M., Khunti K. Effectiveness of interventions for reducing diabetes and cardiovascular disease risk in people with metabolic syndrome: Systematic review and mixed treatment comparison meta-analysis. Diabetesobesity Metab. 2012;14:616–625. doi: 10.1111/j.1463-1326.2012.01571.x. [DOI] [PubMed] [Google Scholar]
- 55.Malik V.S., Popkin B.M., Bray G.A., Després J.-P., Willett W.C., Hu F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care. 2010;33:2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ge K. The transition of Chinese dietary guidelines and the food guide pagoda. Asia Pac. J. Clin. Nutr. 2011;20:439. [PubMed] [Google Scholar]
- 57.Schönfeldt H., Hall N., Bester M. Relevance of food-based dietary guidelines to food and nutrition security: A South African perspective. Nutr. Bull. 2013;38:226–235. doi: 10.1111/nbu.12027. [DOI] [Google Scholar]
- 58.Chen G.-C., Szeto I.M., Chen L.-H., Han S.-F., Li Y.-J., Van Hekezen R., Qin L.-Q. Dairy products consumption and metabolic syndrome in adults: Systematic review and meta-analysis of observational studies. Sci. Rep. 2015;5:14606. doi: 10.1038/srep14606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tian Y., Su L., Wang J., Duan X., Jiang X. Fruit and vegetable consumption and risk of the metabolic syndrome: A meta-analysis. Public Health Nutr. 2018;21:756–765. doi: 10.1017/S136898001700310X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.